Meningoceccemia: General Overview, Diagnosis, Laboratory Investigations, Treatment, Prognosis And Prevention
The Physical Presentation Of Meningococcemia

Clinical Overview
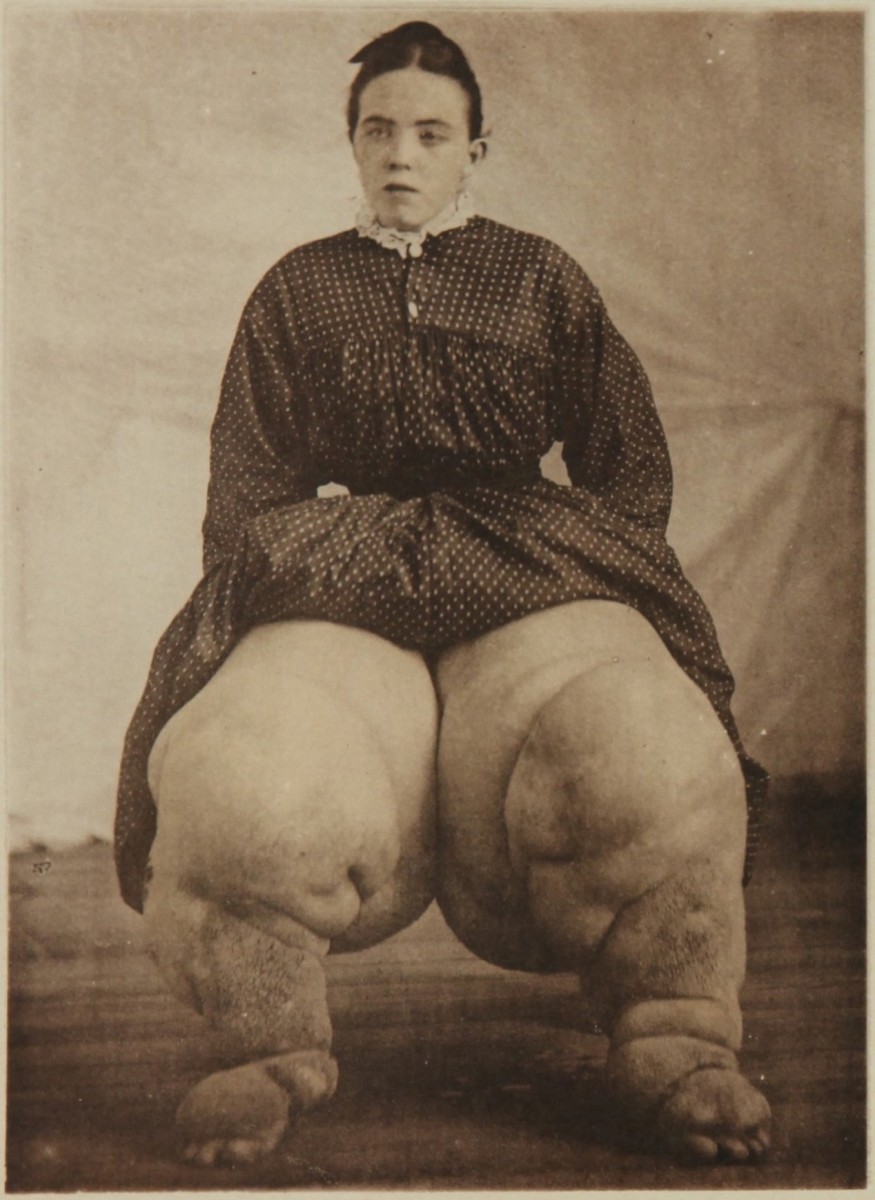
Meningococcemia may be fulminant or chronic. The fulminant form is characterized by abrupt onset, severe constitutional disturbances, peripheral vascular collapse, shock and sometimes myocarditis. The skin rashes are extensive and may even ulcerate. Though in many cases, there is associated meningitis, the signs of meningeal irritation may be absent due to shock. In some cases, the illness may progress rapidly so that toxemia and shock may occur within hours- these features are collectively called Waterhouse Friderichsen syndrome. This syndrome is caused by hemorrhage into the adrenal glands resulting in acute adrenal failure. Toxic vasculitis aggravates the hypotension. Complications include endocarditis, allergic polyarthritis, pneumonia and osteomyelitis.
Chronic meningococcemia is characterized by intermittent fever lasting for several weeks, maculopapular rashes, erythema nodosum, arthralgia or arthritis and splenomegaly in 20%. If left untreated, the infection may either subside or progress to meningitis.
Other rare meningococcal lesions include pneumonia, genitourinary infection, endocarditis, osteomyelitis and purulent conjunctivitis. In acute meningococcal infections, polymorphonuclear leucocytosis with total counts going up to 12,000 to 40,000/cu.mm is common. In chronic meningococcemia, the leucocyte count may be normal.
Diagnosis: Clinically, meningitis is diagnosed when there is fever, severe headache and signs of meningeal irritation. This has to be distinguished from meningism which is seen in toxic febrile states where the signs of meningeal irritation are present but the CSF is normal. Meningitis has to be distinguished from encephalitis, subarachnoid hemorrhage and other causes of coma. Meningococcal meningitis has to be distinguished from other causes of purulent meningitis. At the slightest suspicion of meningitis, lumbar puncture should be done and the CSF should be examined to establish the diagnosis. Since early diagnosis and institution of specific antibacterial treatment is the most important single factor in determining the outcome, lumbar puncture should not be delayed.
Diagnosis Of Meningitis And meningococcemia

Laboratory Investigations
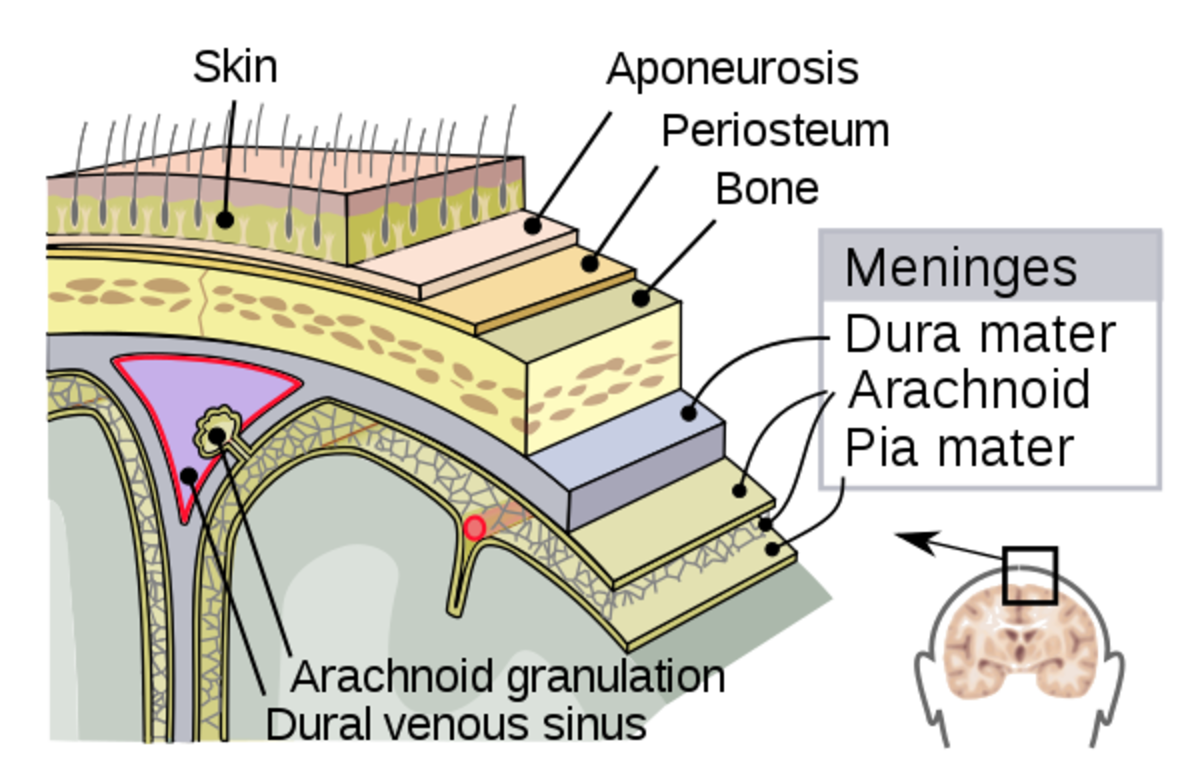
The diagnosis of meningitis is established by examination of the cerebrospinal fluid. The CSF is under pressure, turbid and shows large number of polymorphs (100 to 10,000/cu.mm) containing intracellular Gram negative diplococcic. When the organisms are small in number, immunofluorescence method helps in identification. Meningococcal antigen is demonstrable by counter-immunoelectrophoresis of the CSF. The CSF has to be collected carefully before administering antibiotics to get a positive culture. In the early stages of meningitis and in meningococcemia blood culture, may yield the organism. Material taken from the rashes shows stainable diplococcic.
Carrier state is diagnosed by isolating the organisms from material collected from the nasopharynx using a West’s postnasal swab. The swab has to be transported to the laboratory in a special medium (Stuart’s medium). Sera of convalescent patients show antibodies to meningococci and these can be demonstrated by complement fixation test, passive hemagglutination or by radioactive antigen binding tests. These tests are helpful in retrospective diagnosis.
Cerebrospinal Fluid Biopsy On A Child With Meningitis

Treatment
As early as possible, specific treatment should be started. Penicillin G is the antibiotic of choice and should be administered intravenously in a dose of 12 to 24 million daily in divided doses. In children, the dose is 16 million units/m2. Treatment should be continued for several days. Ampicillin in a dose of 200 to 400 mg/Kg body weight daily is also equally effective. Since penicillin and ampicillin enter the CSF through the inflamed meninges, intrathecal administration is not necessary. In penicillin- allergic patients, chloramphenicol in a dose of 4 to 6g daily in divided doses can be used intravenously.
The administration of antibiotics is continued at high disease till the CSF becomes clear and cell count comes down. Thereafter the drug is continued at a lower dose till all symptoms subside and the CSF returns to normal. Return of the CSF sugar level to normal indicates full recovery.
Supportive treatment consists of the maintenance of nutrition, fluid and electrolyte balance, treatment of shock and the management of convulsion. Adrenal crisis should be managed with large doses of hydrocortisone.
Course and prognosis: The disease was invariably fatal before the advent of specific antimicrobial therapy. At present, the mortality is reduced to 10%. Early institution of therapy also prevents the development of complications.
Prevention: During epidermics, it should be the aim to reduce the carrier state among the susceptible population. Chemoprophylaxis using sulphasomidin, 0.5g every 6 hours for 5 days is effective, when the organisms are sensitive. Rifampicin 600 mg given daily for four days prevents the development of meningitis in contacts.
Immunoprophylaxis: A vaccine prepared against the high molecular weight polysaccharide antigen from serogroups A and C is available for subcutaneous use. This vaccine has been shown to induce specific antibody response.
© 2014 Funom Theophilus Makama