Myths, Facts and Naked Truth About Breast Cancer
Myths, facts and naked truth about breast cancer
One of the most commonly believed myth is that wearing deodorant causes breast cancer. This is not a fact. But there have been some reports that chemicals found in deodorants and antiperspirants can enter the skin and cause changes in the breast cells that could cause or lead to cancer. But luckily, research does not support a link between deodorant use and breast cancer.
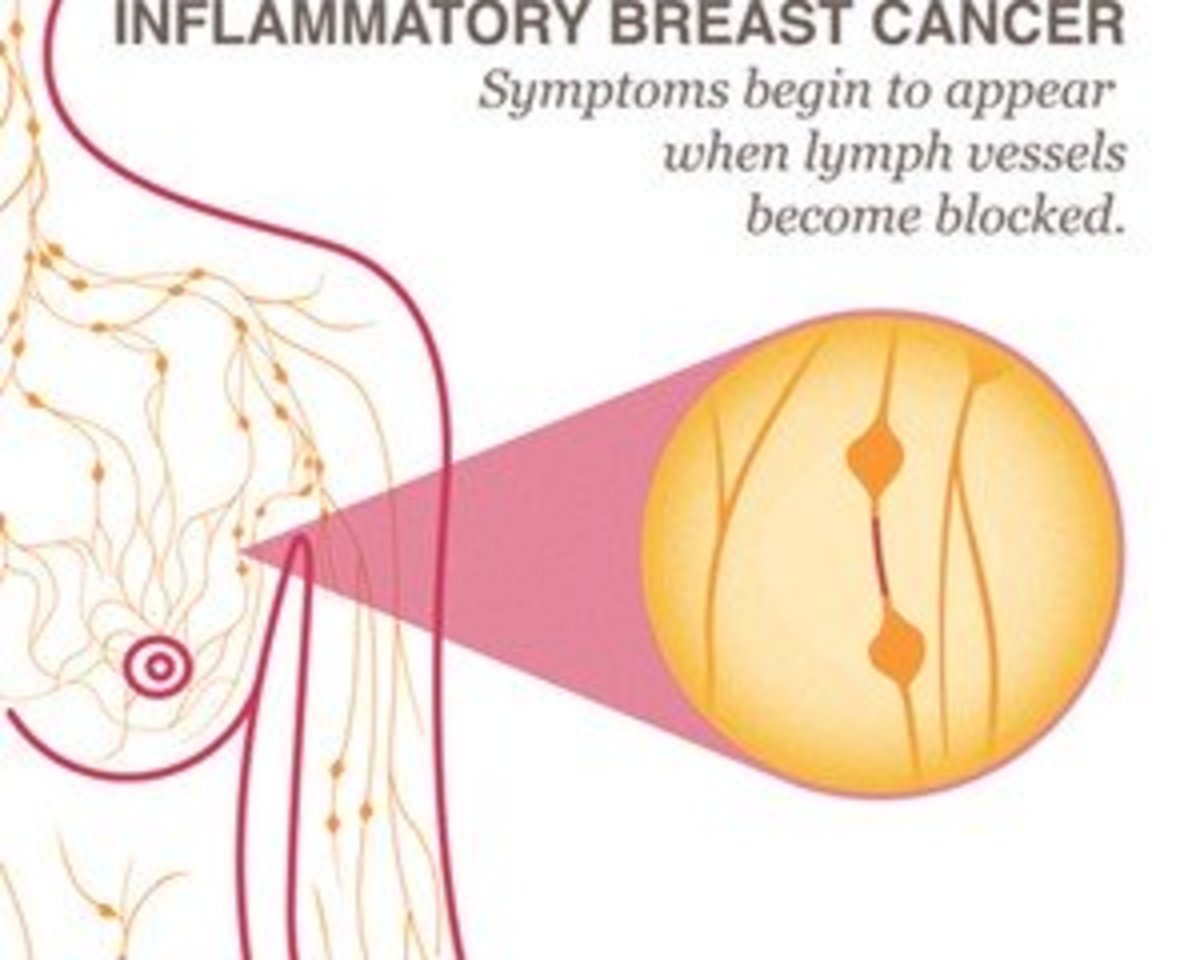
The staging of breast cancer refers to the extent of the disease. The cancer stage is based on several factors, including the size of the tumor, any lymph nodes are involved. State zero is considered a non-invasive breast cancer. Breast cancer is often classified into two types: non-invasive, (not tending to spread undesirably or harmfully), and invasive (tending to spread very quickly and undesirably or harmful). Breast cancer is a disease in which cells in the breast grow out of control. There are different kinds of breast cancer. Most breast cancers begin in the ducts or lobules. Breast cancer can spread outside the breast through blood vessels and lymph vessels.
Today, the most commonly believed myth is wearing a bra causes breast cancer. Scientific evidence does not support any evidence or link between wearing an underwire bra, or any type of bra can cause a risk.
The most commonly believed myth is injury or trauma to the breast, like getting hit on the breast could cause breast cancer. There is no such link or fact known that getting hurt would bring on the risk of cancer.
In the same line another strong myth is having a family history of breast cancer may cause one to believe that they would also be prone to breast cancer. A family history of certain types of cancer can increase your risk of breast cancer. However, most women with breast cancer do not have a family history of the disease. In fact, only about 13 percent of women with breast cancer have a close relative (mother, sister or daughter) with breast cancer. Though, a person without a family history should be aware that she can be a victim of breast cancer. Yet, it is not known which factors come together to cause breast cancer.
The most common myth is breast cancer always forms a lump. Most people know that a lump in the breast may be a sign of breast cancer, but there are actually other warning signs one need to know about. Most of the warning signs are visual changes that cannot be felt.
Breast Cancer Risk Factors
Family history: The risk of developing breast cancer doubles if your mother, sister, or daughter has been diagnosed.
Race: White women are more susceptible than African Americans to develop breast cancer; however, African American women are more likely to die from breast cancer partly because their tumors seem to grow faster.
- Additional factors are dense breast tissue.
- Previous radiation treatment to the chest (for another illness, lesion or lymphoma)
- A greater than average number of menstrual periods (starting before age 12, or reaching menopause after age 55).
- No pregnancies, or having your first pregnancy after the age of 30.
- Post-menopausal hormone therapy: Avoiding this treatment decreases your risk of breast cancer.
- Smoking.
- Excessive alcohol consumption.
- Not breastfeeding.
- Being overweight and having a high-fat diet.
- Lack of exercise.
The goal of breast cancer screening is to find cancer early before it has a chance to grow, spread, or cause problems. Studies show that being screened for breast cancer lowers the cancer that a woman will die from the disease.
Recommendations
The most current recommendations are to:
- Perform monthly breast self-exams.
- Yearly mammograms starting at age of 40.
- Obtain a yearly clinical breast exam performed by a health professional at age of 40.
- Women in their 20s and 30s should have a clinical breast exam as part of a periodic health exam by a health professional preferably every three years.
The BRCA gene test is a blood test that uses DNA analysis to identify harmful changes (mutations) in either one of the two breast cancer susceptibility genes. The BRCA test is offered only to people who are likely to have an inherited mutation based on the personal or family history. The BRCA gene test is not routinely performed on women at average risk of breast and ovarian cancers.
Having a BRCA gene mutation is uncommon. Inherited BRCA gene mutations are responsible for about 5 percent of breast cancers and about 10 to 15 percent of ovarian cancers.
False positives – mammograms sometimes give “false positives” meaning they suggest a woman might have cancer when she does not. This can lead to unneeded worry and to more tests possibly including a biopsy which can be painful and expensive. False positive results are more likely to happen in women younger than 50 than they are in older women.
False negative results occur when mammograms appear normal even though breast cancer is present. Overall, screening mammograms miss about 20 percent of breast cancers that are present at the time of screening. The main cause of false-negative results is high breast density. High breast density tissue and tumors have similar density so tumors can be harder to detect in women with denser breasts. False-negative results occur more often among younger women than among older women, because younger women are more likely to have dense breasts. False-negative results can lead to delays in treatment and a false sense of security for affected women.
Some of the cancers missed by screening mammograms can be detected by clinical breast exams (physical exams of the breast done by a health care provider).
Women with breast implants should continue to have mammograms. Implants can hide some breast tissue making it more difficult for the radiologist to detect an abnormality on the mammogram. A special technique called implant displacement views may be used. If the mammogram was abnormal or the image was not clear enough to interpret the results, the patient will be called back for a follow-up visit. This may include a more detailed mammogram, an ultrasound or a breast MRI. In some cases, a biopsy may be needed. It is not uncommon to be called back for an abnormal finding. On an average nearly 10 percent of women are called back. Sometimes, women with an abnormal mammogram turn out NOT to have breast cancer.
The patient should undergo a breast exam on a regular basis as part of the breast cancer screening. During the exam, the doctor will examine the breasts, and the area under both arms. The doctor will look for lumps, nipple changes, or any changes in the tissue or skin that could signal cancer.
This content is accurate and true to the best of the author’s knowledge and is not meant to substitute for formal and individualized advice from a qualified professional.
© 2019 Putcha Venu Madhav