Age Specific Care - Neonates to One Year Old

Neonate to One Year Old
This is the first article of a series written for healthcare workers on age specific care. Nurses, nursing students, nursing assistants, caregivers and parents alike will benefit from the following information.
Normal Vital Signs for a Child
Rectal Temperature
| 97.9-100° F
| |
|---|---|---|
Respiratory Rate
| Initially 40-60 breaths per minute, dropping to 30-40 after the first few minutes of life and up to 1 year
| |
Heart Rate
| 140 beats per minute up to 3 months, and 130 from 3 months to 1 year
| |
Blood Pressure
| 60/30-70/45 at birth ; 68/22-104/60 at one year
|
Vital signs for a child differ from those of an adult.
Physical Growth and Characteristics
The first four months of a child's growth centers around the head: smiling, following objects with eyes, maintaining head control and oral activities such as sucking. A fontanelle is an area of the skull which has not closed yet to allow the rapid growth of the brain. The two pairs of fontanelles on the sides of the head, lateral, close by the second or third month. The fontanelle in the back, posterior, closes by 6-8 months. Birth weight drops by about 5-10% in the first week of life due to excretion of fluids. Exceeds birth weight by second week, doubles birth weight within 4-6 months, and triples by one year. An infants head accounts for 25% of their total weight. Infants have rapid growth in the first year, especially in the brain. They learn through playing, exploring, and using their senses. They have strong coordinated suck and gag reflexes. Extremities move equally when the infant is stimulated.
Between 5 and 7 months, teething begins. They have increased development of the distal limb portions demonstrated by creeping, standing, and walking with assistance. Passive immunity is based on maternal antibodies, provided the infant is breast-fed. Airways in infants are narrower, shorter, and more easily obstructed. Infants are primarily nose breathers until 4 weeks of age. Noisy breathing can indicate restricted airflow and the need to reposition the airway or nasal suctioning with a bulb syringe.
Special Considerations
Respiratory rate should never be over 60 in any child. Rapid respiratory rates can lead to rapid heat and fluid loss. Slow heart rate, less than 60 beats per minute, MAY indicate the need for external cardiac compressions. Tub baths should only be given after the umbilical cord falls off. Infants have very sensitive skin that dries easily, so moisturize while still damp from the bath to protect the skin. In between baths, keep face and bottom very clean. Immunization schedules should be followed closely, as should routine medical screenings.
Safety Concerns
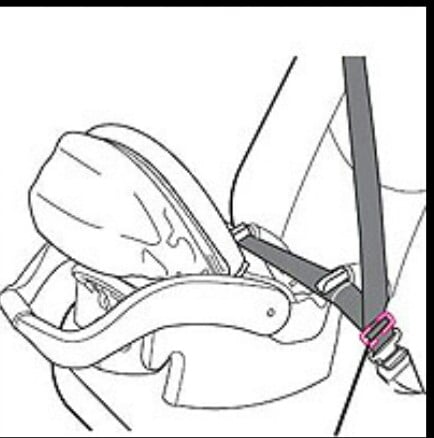
Utlize equipment that is specific to size and age. To help prevent the possibility of sudden infant death syndrome (SIDS), remember to lay the infant on their back or side, NEVER on their belly. Crib side rails should be kept up at all times. Never leave an infant alone on a changing table, bed, sofa or chair. Never leave an infant unattended near water. When giving an infant a bath, never use hot or cold water. The water should be warm. If a toy or detachable part will fit into a toilet paper tube, it is too small for a child this age. A car seat, rear-facing' in the back seat is required. Never place a child's car seat where an air bag can deploy.
Psychosocial Needs-Communication
The infant learns to communicate through facial expressions, crying, cooing and babbling. Eventually the child will learn to vocalize syllable sounds like "ma-ma", "da-da", and will imitate adult sounds. The infant likes to be held, touched, cuddled, smiled at and talked to. He/she cries strongly when hungry or uncomfortable, and learns to show emotion such as frustration, fear, anger, jealousy and affection. Call the infant by name and never approach too quickly so as not to startle.
Psychosocial Needs-Infant Stress
Infant stress can be brought on by over-stimulation. Stranger and seperation anxiety emerge at six to eight months. Physical indicators of stress include: the closing of eyes, fretting, turning away, increased formation of stool, increased motor activity, change in color or hyper-alertness. In the healthcare setting, try to assign the same staff to the patient daily and encourage parents to stay with the child as much as possible. To reduce stress in any situation you can 1. Incorporate the concept of play into the environment. 2. Attend to physical needs promptly and provide consistency in routines and responses. 3. Social interactions like talking, reading, or singing can reduce stress. 4. Keep the infant on the parent's lap if possible.

Psychosocial Needs-Parental Stress
Parents often suffer from stress when their little one is ill. This stress may be exhibited as anger, hostility, fear, rudeness, demanding behavior, lack of cooperation, or feeling suspicious toward healthcare staff. Try to stay calm and show your understanding. You can relieve stress through flexibility- by modifying care, making changes when possible, and showing the parent that you consider them a partner in the child's care.
Parental Education
Provide education to parents (without belittling their knowledge base) on the following: 1.Car seats are required. 2. Never leave infants unattended near water or on changing tables, sofas, or chairs, or anywhere they may fall from and cause injury. 3. Provide a safe environment for exploring and playing. For example: Crawl proof and baby proof by covering electrical plates, removing small objects that could be potential choking hazards (remember the toilet paper tube rule), and cords and/or ropes that could strangle. This includes long cords on blinds and window coverings. 4. Infants younger than six months old should not be exposed to direct sunlight, and those older than this should use sunscreen when in the sun. 5. Encourage proper nutrition, oral health, skin care, and follow immunization and screening schedules.
© 2012 Cynthia








