On the Public - Stigma of Schizophrenia Spectrum
Importance of studying schizophrenia
The biological factors, the environmental elements, the brain functioning, the drug usage, the family history of mental illnesses and many other significant reasons, as well. Over the years, scientists try to examine the holistic etiology of schizophrenia and so, they have conducted a variety of scientific studies. Interventions are an important topic for the schizophrenia spectrum as they can have an impact on the lives of people with such mental illnesses and their family and also the social environment. In general, the mental illnesses is a very sensitive field, in which many types of research and psychiatrists have disagreed for many reasons.
Schizophrenia cannot be understood without understanding despair.
— R. D. LaingSchizophrenia spectrum is a severe mental disorder which is identified in more than 21 million people worldwide (World Health Organization, 2016). The population that is more affected by this specific disorder is the men, which is 12 million, whereas females are 9 million (WHO, 2016). Although schizophrenia spectrum disorder is not a common broadly mental disorder like other mental disorders are, it has stimulated the interest of many mental health scientists and continues to find new treatment prospects (Jablensky, 2010). Until now, schizophrenia remains an elusive mental disorder. Nowadays, new research is being carried out on functional psychopathology so that the present disease of schizophrenia can be reworked (Ban, 2004).
Furthermore, schizophrenia causes a variety of dysfunctions in emotions, in the cognition and in the behavior, as well (National Institute of Mental Health, 2017). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), has added the term ‘spectrum’ near schizophrenia (American Psychiatric Association, 2013). Many times, the patients who suffer from this kind of severe mental disorder, think that their family or their social environment may want to hurt them or are against them (NIMH, 2017). Moreover, a lot of times these people give the impression that they live in their own fantasy world.
The symptoms of schizophrenia are classified into 3 categories. These categories include the
- positive symptoms,
- also the negative symptoms and
- finally, the cognitive symptoms (Addington, Addington & Maticka – Tyndale, 1991).
The positive symptoms are these symptoms which include psychotic experiences which are difficult to be differentiated from the reality. These are the delusions, the hallucinations, also the disorganized speech. The negative symptoms are being characterized by a dysfunctional in emotions and behaviors. These symptoms include the reduced satisfaction for life, the emotional flatness and the reduced speaking (Addington, Addington & Maticka – Tyndale, 1991). Finally, the cognitive symptoms include problems with the memory and also with the thinking.
Additionally, some people tend not to have severe problems, while others are facing serious issues. Cognitive symptoms are the low ability to understand (executive functioning), the difficulties in focusing and the issues with memory (Addington, Addington & Maticka – Tyndale, 1991). Hence, there are five types of schizophrenia. Firstly, the paranoid type, secondly the disorganized, the catatonic type, the undifferentiated and also the residual schizophrenia (Psycom, 2017).
In addition, the causes of schizophrenia are still unclear. However, the scientists are still examining this mental disorder, since old times. Schizophrenia has come from the ancient times. The oldest description of schizophrenia is coming from the 1550 B.C. in the Ebers papyrus, in Egypt. Moreover, in the Stone Age, there have been discovered skulls with holes into them (Burton, 2012; Howe, 1991). According to scientists, this phenomenon had to do with the disappearance of evil spirits from the individual’s mind and body. Although there have been conjectures about some kind of possession by evil spirits, experts faced the madness like a mental issue (Yip, 2006).
Furthermore, many episodes which were included hearing voices and also seeing visions had made their appearance in the literature from the 17th century (Cutting & Charlish, 1995). Swiss psychiatrist Paul Eugen Bleuler (1911) was the one who coined the term “schizophrenia”. He believed that the schizophrenia tends to provide a better consciousness of experiences and also memories. The medical term for schizophrenia comes from Greek words. The ‘schizo’ which means split and the ‘phren’ which means mind (Ashok, Baugh & Yeragani, 2012). Schizophrenia is considered to be a very serious and also confused about its nature mental disorder.
By the middle of 19th century, European psychiatrists started to describe and also give medical terminologies to mental disorders, especially of those which were for unknown reasons (Jablensky, 2010). Some of this psychiatrist is the following. Morel (France) referred to the mental disorders as démence précoce (Morel, 1860). Clouston (Scotland) gave the term adolescent insanity (Clouston, 1904). Kahlbaum (Germany) named it as the catatonic syndrome (Kahlbaum, 1863). Hecker (Germany and Kahlbaum’s disciple) gave the name hebephrenia (Hecker, 1871).
However, Emil Kraepelin (1909) was the one who after completed a series of observations and researchers on many individual cases, he finally named the mental disorders.
He supported the idea that additional studies were needed in neuropathology, physiology, and biochemistry of the brain, as well, in order to conclude to a specific medical term (Kraepelin, 1909). His specific term was dementia praecox (Kraepelin, 1909).
In a population, the distribution of any mental disorder is measured in incidence and prevalence. In the case of schizophrenia, although it is difficult to get clear investigations because of the specificity of this disorder, however, surveys in 10 different countries have shown that adults are affected by between 0.1 and 0.4 per 1000 individuals (WHO, 1997). The frequency of schizophrenia is the same in different countries (Warner & de Girolamo, 1995). High rates are observed in the United States of America (Tien & Eaton, 1992). Europe has the same percentages as Western countries respectively. A study that took place in Europe in 2010 showed that 38.2% each year people experience some kind of mental disorder, either severe or mild (Wittchen et al., 2011).
Specifically, International Epidemiologic studies have shown that the incidence of the schizophrenia varies from 0.11 to 0.69 per 1000 people and the prevalence is between 0.6 to 0.8%. In 98% of the cases, the schizophrenia has been diagnosed in a population under the 45 years old (Girard & Simard, 2008). It is important to be noticed that schizophrenia is more common in men rather than women (Abel, Drake & Goldstein, 2010). According to a study by World Health Organization in 2000, schizophrenia has almost the same age and prevalence over the world (Ayuso – Mateos & Jose, 2013). The peak years which schizophrenia can be appeared and becoming more obvious, are from 20 – 28 years old to men and 26- 32 years old to females (Castle, Wessely, Der & Murray, 1991).
Schizophrenia is considered to be the most severe psychiatric disorder, affecting around 1% of the world’s population, with the prevalence rates, as it was mentioned above, is similar across all cultures and ethnicities (Bener, Daffeah & Samson, 2012; Meli, Ottl, Paladini & Cataldi, 2012).
Nevertheless, the causes of the schizophrenia spectrum are still unclear (Abel, 2004; Tomasik, Schwarz, Guest & Bahn, 2012). However, there have been conducted a range of studies and also researches, over the years on this specific topic. According to scientists, schizophrenia’s etiology includes many factors. It is believed that the elements which play a major role to the development of the schizophrenia spectrum are genetic, environmental, biological and physiological (Abel, 2004; Tomasik, Schwarz, Guest & Bahn, 2012).
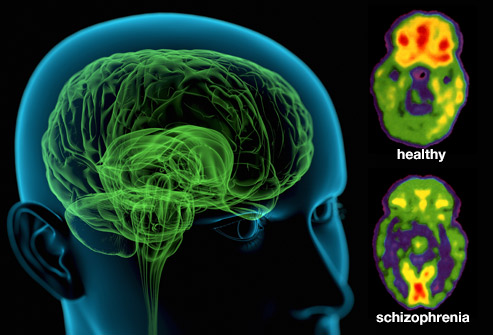
Schizophrenia tends to have a high heritability, as well (Schwab & Wildenauer, 2013; Sullivan et al., 2008). On the other hand, the 1st-degree relatives had not shown this mental disorder (Moore et al., 2011). According to other studies, it has been identified that the environmental factors contribute to the development of the schizophrenia spectrum disorder (Van Os, Rutten & Poulton, 2008). Biological factors are also very important and they are involving to the development and even the progress of schizophrenia (Brown, 2011). These factors can be the abnormal neurodevelopment during the early stages of life.
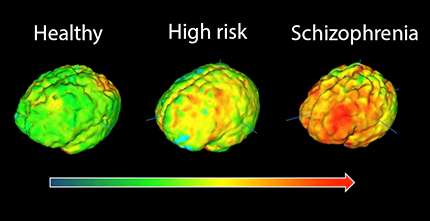
According to Dr. Pasca, it is very challenging the examination of the development of the brain, as well (Sloan et al., 2017). The investigation of the role of the astrocytes in the mental disorders and also in the normal development has shown important results for the understanding of disorders. The lab-grown cells change over time during early lifetime. As a consequence, the deviations can cause either schizophrenia or autism (Siloan et al., 2017).
Another important element is the hormones (Fernandez – Egea et al., 2011; Ko et al., 2007). The hormones can be affected by schizophrenia, such as the sex hormones (estrogen, progesterone, and testosterone). Furthermore, the schizophrenia spectrum is being affected also by the environmental factors (Liang & Chikritzhs, 2012). Moreover, a study has shown that the individuals who had been hospitalized more than twice in their first three years of their life, they tend to have higher levels of showing and developing schizophrenia (Liang & Chikritzhs, 2012).
What is more important to be mentioned is that not only the genetic factors affect the schizophrenia spectrum disorder but also many other external factors. One of those factors which were mentioned before is the environmental factors (Liang & Chikritzhs, 2012).
Consequently, many studies have been conducted in the past, but also continue to be done until now. A cross-sectional study with 204 participants in China showed higher ratings of public stigma for schizophrenia spectrum than other mental illnesses such as depression and psychosis-like experiences (Lee et al., 2016).
Moreover, another study in Central Europe and also in North Africa showed diversity in the results (Angermeyer et al., 2015). The two countries where the study was done were Germany and Tunisia. In Tunisia, people face in another way with schizophrenia. They tend to make the patient absolutely responsible for the disturbance he owns. However, the social environment does not show any particular behavior for these people (Angermeyer et al., 2015). But a certain distance exists in the family environment. In Germany, there is the social isolation of these people. So, as it is observed, there is a difference in culture (Angermeyer et al., 2015).
Other Global Context – Belgian Mental Health study with 728 individuals using face to face interviews, proved that there is the public stigma for mental illnesses (Pattyn et al., 2014). Ιn the present study it was observed that some kind of prevention and also the possible treatment of a psychiatric disorder is avoided by people (Pattyn et al., 2014). Whereas, in 340 Amazon Mechanical Turk survey takers, by using a brief measurement it was proved that there is negative reaction about the medical term ‘stigma’ (Sheehan et al., 2015).
Further study, to 153 urban college respondents using questionnaires, showed that there is the more negative behavior to people with schizophrenia, greater social distance and finally, less intention for seeking help (Yang et al., 2013). Semi-structured interviews have done to 16 mental health clinicians from public mental health services in New South Wales, in Austalia. (Outram et al., 2014). These interviews indicated that τhere is a kind of fear and protection towards patients suffering from schizophrenia (Outram et al., 2014).
Further study to 65 relatives of patients with schizophrenia, by using the ISE (Stuart, Koller & Milev, 2008) and the Burden Inventory for Relatives of Persons with Psychotic Disturbances (Hjärthag, Helldin & Norlander, 2008), had negative results (Allerby et al., 2015). The quality of life (QoL) among relatives had many issues.
On the other hand, according to many studies, individuals who suffer from schizophrenia spectrum are facing a lot of difficulties in their daily life (Link et al., 2001). They have low levels of self – esteem. They tend to show also depressive symptoms. Researchers have conducted many studies so as to focus on the psychology of schizophrenics (Berenbaum & Oltmanns, 1992; Kring et al., 1993; Kring and Neale, 1996). These studies have shown that people with schizophrenia also do not participate in many activities.
To continue it is the very important issue the interventions which will be used for the schizophrenia spectrum. Those people who suffer from schizophrenia and are showing ups and downs almost every day to their mood and behavior need to follow a stable special medical prescription for the appropriate treatment. (Lavretsky, 2008). For the improvement of the quality of life (QoL) to people with schizophrenia and also their family and social environment, need some changes in many aspects. These aspects have to do with the pharmacological and psychosocial treatments (Lavretsky, 2008). Also, with the way in which society treats these people. Also, how the relatives cope with their people.
There are a lot of mental cases [on the streets]. A lot of them have schizophrenia and they tend to use drugs a lot.
— David DavisA very important topic is the suitable medical drugs which are very significant for schizophrenia, to be taken. A lot of products had developed for schizophrenia spectrum and such psychotic disorders, as well. For instance,—ITI-007 (Intra-Cellular Therapies), MIN-101 (Minerva Neurosciences), and NaBen (SyneuRx)—for the negative symptoms. In addition, AVN-211 (Avineuro Pharmaceuticals), for the cognition impairments and Lu AF35700 (Lundbeck). To sum up, three formulations of risperidone—risperidone implant (Braeburn Pharmaceuticals), risperidone ISM (Rovi), and RBP-7000 (Indivior), (Michaelidis, Markwick & Robbins, 2016). On the other hand, another important intervention which is suggested from the experts, is the avoidance of street drugs, especially when there is family history with mental disorders.
Furthermore, it is important to be identified the problems which are being caused by the usage of cannabis and related drugs. Thirty different studies took place in UK, Australia, and Sweden over the past 20 years to 50.000 members of Swedish Army. Those who were users of cannabis at the age of 18 years old had 600% more possibilities to be diagnosed with schizophrenia later in their life (Zammit et al., 2002). The 8% and 13% of schizophrenia cases are because of the usage of cannabis and marijuana, especially during teen years. This is happening, because the brain is still developing and is very sensitive, as well (Ecognitive.com, 2017). Moreover, the family history of mental illnesses is the very suspicious element for the development of schizophrenia.
Additionally, according to psychiatrists, the users of cannabis are 80% more likely to develop schizophrenia, while heavy users have higher possibilities to develop psychosis (Mac Donald, 2011). As the researchers supported, this is happening because the cannabis boosts the chemical dopamine in the brain and this is a serious reason for leading to schizophrenia (Matthysse & Kety, 2014).
Symptoms of Schizophrenia
Positive Psychotic Symptoms
| Postive Disorganization Symptoms
| Negative Symptoms
|
|---|---|---|
Hallucinations
| Disorganised speech, thought, language
| Alogia (poverty of speech)
|
Delusions
| Thought disorder characterization: thought blockibng, loosening of associations, tangentiality
| Flat affect
|
Disorganized behavior
| Poor attention
| |
Avolition (loss of motivation)
| ||
Anhedonia (lack of pleasure)
| ||
Loss of social interest
| ||
Attentional deficits
|
“Social situations were almost impossible to manage. I always came across as aloof, anxious, nervous, or just plain weird, picking up on inane snippets of conversation and asking people to repeat themselves and tell me what they were referring to.”
— Surviving Schizophrenia: A Manual for Families, Patients and ProvidersThe DSM – 5 includes a chapter of schizophrenia which is also sequenced with bipolar and other related disorders (Cross-Disorder Group of the Psychiatric Genomics Consortium, 2013). Also, bipolar disorder occupies a place between schizophrenia and other psychotic disorders (Goldberg, Krueger, Andrews & Hobbs, 2009).
There is a huge gap about the mental illness hypothesis. The researchers often tend to disagree with each other about mental disorders, either severe or no.
Nevertheless, it is widely known that any kind of mental illness can impact the quality of life (QoL). Many do not want to receive the appropriate medical attention because of the public stigma. Public stigma is extremely painful for those who suffer from a mental illness and specifically, those who have schizophrenia.

By improving the reliability of mental disorders will aim to better help the treatment of patients suffering from mental disorders. In addition, psychiatrists support responsibility towards patients. Therefore, they believe that improving their communication with their colleagues will contribute to ways of dealing with mental disorders, information about patients and their family and possible new therapies and interventions, as well (Almoshawah, 2010). As noted before, mental disorders are an important part of human health. Scientists have been researching for many years to understand the nature of this disorder. Addressing these people's societies clearly and positively calls for new, more positive debt and new scientific interventions for its greater effectiveness so that it will be a positive factor for individuals and also for the public stigma.
© 2018 Chrysi Stamou