Overview of Iron Deficiency Anaemia
Iron Deficient Red Blood Cells
Overview
Anaemia is highly prevalent in Australian society. This blood disorder caused by a lack of iron that results in a deficiency of oxygen circulation effects all age groups as well as displaying larger effects on society, families and individuals. This article aims to give a brief overview of the symptoms, causes, effects, support as well as management of Iron Deficiency anaemia.
Sources
Symptoms and causes are based on information provided by the following organisations; Dietitians Association Australia (DAA), the Australian Red Cross Blood Service (ARCBS), Primal Pitchers (PPL) and the Australian Bureau of Statistics (ABS). Effects are derived from personal diary entries, the Medical Journal of Australia (MJA) as well as conclusions drawn from the effects of the disorder in regards to the impact on society, families and individuals. Support groups include MD Junction (MDJ) and Daily Support (DS). A dietary plan is provided in relation to management of the disorder and draws further information from (DAA) and (ARCBS).
Agenda
- Symptoms: Physical and Psychological.
- Causes: Social/Interpersonal and Cultural.
- Impact on Society, Families, & Individuals: Socio-Demographic Factors and Effects of Society, Family's and Individuals.
- Support Groups: Effectiveness and Strengths and Weaknesses.
- Diet Managment: Nutritionally Balanced Diet and Requirement for Healthy Eating
Symptoms
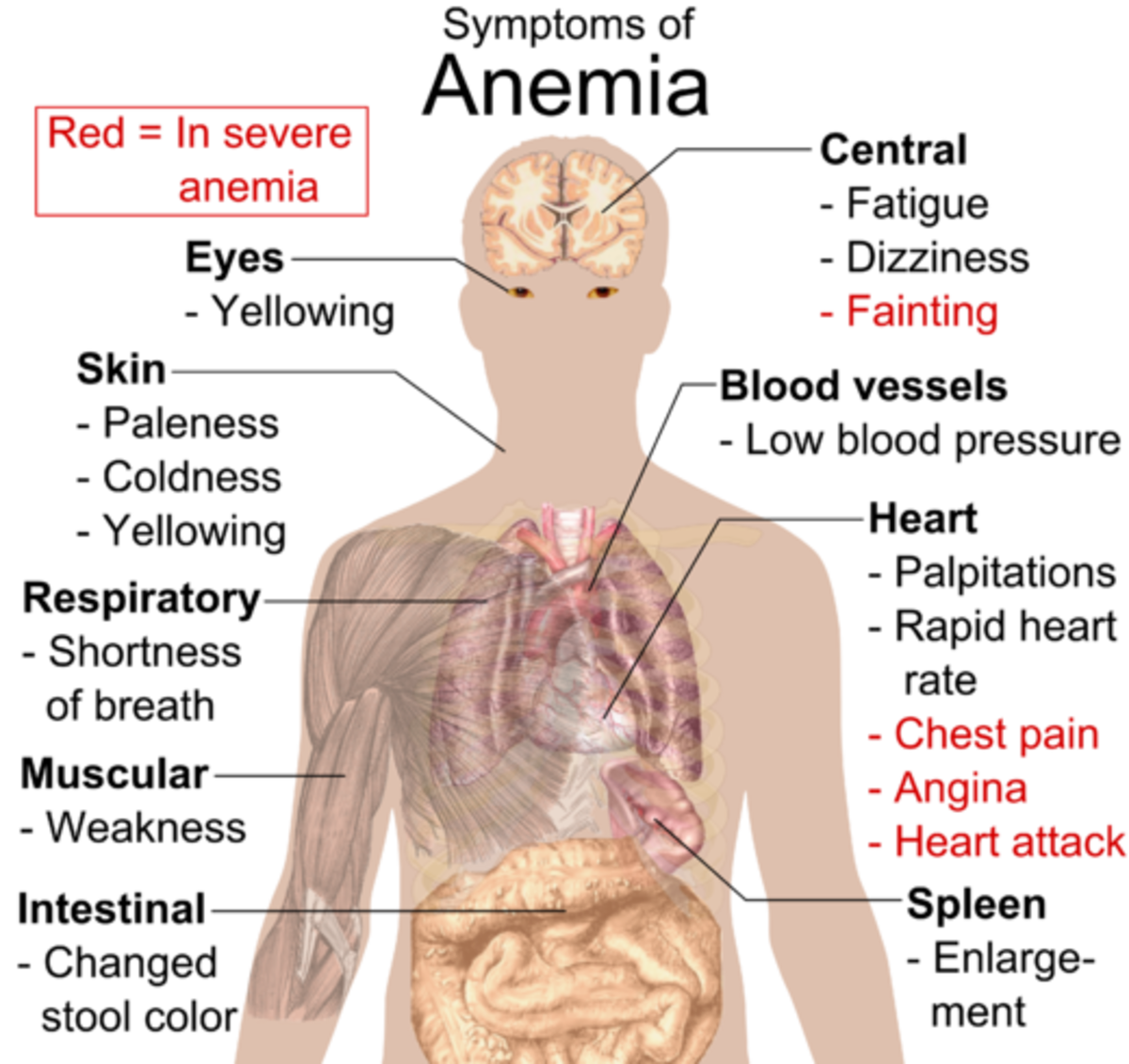
It is widely agreed that anaemia causes a variety of unpleasant symptoms.
Common symptoms of anaemia include: “tiredness, fatigue, pale skin, irritability, and increased sensitivity to the cold” (DAA). The Australian Red Cross Blood Service does not mention fatigue, pale skin or increased sensitivity, however they do include breathlessness and chest pain (ARCBS). These symptoms are attributed to tissue hypoxia (PPL).
Uncommon symptoms include: “headaches, palpitations, altered taste and ringing in the ears” (ARCBS). The most identifiable symptom of anaemia is pale skin which can be seen most easily by examining the inside of the eyelid (PPL). This method of indication is commonly used by medical practitioners to determine the level of risk to the individual in regards to whether emergency attention is required.
Table 1 Symptoms
Common Symptoms
| Uncommon Symptoms
|
|---|---|
Tiredness
| Headaches
|
Fatigue
| Palpitations
|
Irratability
| Altered Taste
|
Pale Skin
| Ringing in the ears
|
Breathlessness
| |
Chest Pain
|
Personal Experiences with Anaemia
Have you experienced Anaemia in your lifetime?
Causes
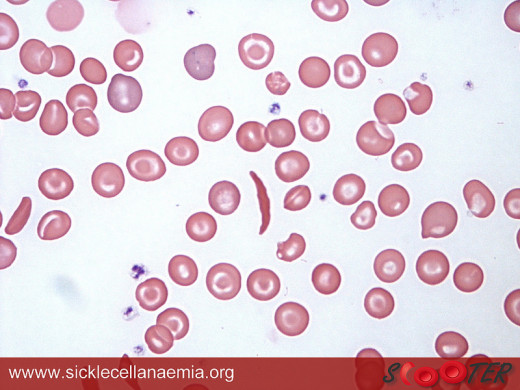
Many things can be responsible for causing Iron Deficiency anaemia. Most commonly it is caused by a nutrition deficiency which can be a result of a number of factors and usually more than one combined. Factors include decreased iron intake or absorption and/or increased iron requirement or blood loss. This unstable balance is what results in malnutrition (ARCBS). A blood test is most commonly used to examine heameglobin levels when testing for anaemia. This is due to the fact that the body requires iron to produce heameglobin which is then used to produce blood. Blood circulates oxygen around the body.
Table 2 Causes
Increased Requirement/Loss
| Reduced Intake/Absorbtion
|
|---|---|
Increased Requirement
| Decreased Intake
|
Increased Blood loss
| Decreased Absorbtion
|
Risk Groups
People at risk of developing anaemia include:
- Underweight children, developing children;
- Menstruating women;
- Athletes; and
- Most impactful the elderly generation.
The elderly have a steep risk increase for individuals aged over 65. That more than doubles when an individual surpasses the age of 75 (ABS).
Other nutrients that play a role in upsetting the balance of iron stores are folic acid and vitamin b12 (DAA).

Current Issues
Socio demographic evidence of anaemia is shown but the Australian Bureau of Statistics as well as information provided by the Medical Journal of Australia.
Ages 12-17 show 2.8% effected by the disorder, 18-24 show 3.4%, 25-34o show 3.7%, 35-44 show 4.2%, 45-54 show 3.4%, 55-64 show 2.7%, 65-74 show 6.1% and most 75+ are 16% (ABS).
Studies indicating the prevalence within Australia 1-6% of toddlers, Asian heritage: 14%, non-pregnant women: 10%, pregnant women not ingesting supplements: 11%, aboriginal decent are 55% for women and 18% for men (MJA). Another high risk group includes blood donors, more specifically up to 20% of Female donors (MJA).
Table 3 Anemia Statistics from the ABS
Ages 12-17
| Ages 18-24
| Ages 25-34
| Ages 35-44
| Ages 45-54
| Ages 55-64
| Ages 65-74
| Ages 75+
|
|---|---|---|---|---|---|---|---|
2.8%
| 3.4%
| 3.7%
| 4.2%
| 3.4%
| 2.7%
| 6.1%
| 16%
|
Sourced from: (ABS)
Demographics of Audience
What Demographic Do you Fall Into?
Research
Although up to date research on the consequences of iron deficiency in Australia is scarce, there is evidence that IDA negatively impacts child development as well as adult cognition and behaviour (MJA). IDA is also known for its impact on physical activity due to energy depletion emerging again from a deficiency of oxygen circulating in the blood stream which may impact societal productivity. However, more longitudinal studies are required to confirm and assess these correlations.
Another Issue
Another important health issue in relation to Anaemia is the cost of blood transfusions particularly unnecessary transfusions where an immediate increase of oxygen is not needed. The cost to society is admittedly largely unknown. However, the cost of blood-based products does exceed six hundred million dollars annually within Australia (ARCBS). This cost is non-inclusive of the transfusion procedure or any complications which may arise (ARCBS).
Major Concerns
The other major concern in relation to the effects of IDA on families is the increased risk of complications during pregnancy. Not only do pregnant women require more iron than usual, but are at “increased risk of low birth weight, prematurity and maternal morbidity” (MJA). Breastfeeding also poses an increased requirement. However, this is negated by lactation-induced amenorrhoea meaning missed periods in some individuals (MJA).
Support Groups
Support groups though hard to find are available for anaemia. The two I have selected to compare are MD Junction and Daily Strength. Both groups allow members to communicate with other members who also suffer from the disorder. This appears to be the most self-evident indication of the group’s effectiveness as journal entries and diary posts show members deeply depressed and isolated.
Daily strength has implemented a goals section showing over six hundred members have chosen to create their own goals with a sizable proportion having also completed them. In contrast to the positive traits of the sites which undoubtable add to their effectiveness, weaknesses are still present. Information provided by Daily strength in relation to the treatment of Anaemia is sourced from Wikipedia and as a result unreliable.
Another concern in regards to user interactions on forums and discussion topics within both support groups is that other member’s advice may not be medically viable and or anecdotal. However both sites do indicate a disclaimer stating that the information it provides does not and should not replace the advice of a trained medical professional.
Support Group

Table 4 Comparison
MD Junction
| Daily Strength
| |
|---|---|---|
Stengths
| Communication tools
| Communication tools
|
Informative Information.
| Informative Information.
| |
Goal Section (Motivation).
| ||
Weaknesses
| Information Difficult to Verify.
| Information Difficult to Verify.
|
Members Advice may be Anecdotal.
| Members Advice may be Anecdotal.
| |
Uses Wikipedia
|
Diet Management
Eating a balanced diet in accordance with iron-rich food is a useful post treatment option, however supplements should still be used if appropriate for the cause when diagnosed with IDA. It is important to note that animal based iron is not only absorbed more easily but also increases the absorption of plant based iron. Following this trend it is handy to eat a serve of green leafy vegetables as a side dish to meat/poultry or fish meal choice.
Foods that decrease iron absorption are tea, coffee and cola drinks which should subsequently be consumed in-between meal times. During meals, drinking juices high in vitamin c can also assist in increased absorption. Other foods that increase absorption are citrus fruits, red capsicum and kiwi fruit.
Breakfast meal options include wholegrain breads and cereals. Whole grain toast with citrus jam or eggs. Lunch should include green leafy salads with green vegetables with the added option of dried beans and lentils. Dinner should contain at least one serve of concentrated iron such as red meat, poultry or fish.
As an alternative to animal products, green vegetables should be increased and/or supplements taken to offset the absence of animal based iron. A side of salad is also recommended with main meals and as a healthy snack. Other snack alternatives are nuts, seeds and citrus fruits.



Table 5 Diet Management
Breakfast
| Lunch
| Dinner
| Snacks
|
|---|---|---|---|
Wholegrain brads and cereals.
| Green leafy salads with green vegetables.
| At least one serve of concentrated iron such as red meat, poultry or fish.
| Green vegetables.
|
Whole Grain toast with citrus jam or eggs.
| With the added option of dried beans and lentils.
| As an alternative to animal products, green vegetables should be increased and/or supplements taken.
| Nuts/seeds.
|
And/or citrus fruits.
|
References
Australian Bureau of Statistics. (2013). Australian health survey: biomedical results for chronic diseases (No. 4364.0.55.005). Retrieved from http://www.abs.gov.au
Australian Red Cross Blood Service. (2012). Anaemia. Retrieved from http://mytransfusion.com.au/node/learn-about-anaemia
DailyStrength. (n.d.). Aneamia support group. Retrieved from http://www.dailystrength.org/c/Anemia/support-group
Dietitians Association of Australia. (n.d.). Anaemia. Retrieved from http://www.daa.asn.au/for-the-public/smart-eating-for-you/nutrition-a-z/anaemia/
MDJunction. (n.d.). Anemia support group. Retrieved from http://www.mdjucntion.com/anemia
Pasricha, S. S., Flecknoe-Brown, S. C., Allen, K. J., Gibson, P. R., McMahon, L. P., Olynyk, J. K., … Robinson, K. L. (2010). Diagnosis and management of iron deficiency anaemia: a clinical update Medical Journal of Australia, 193(9), 525-532. Retrieved from https://www.mja.com.au/journal/2010/193/9/diagnosis-and-management-iron-deficiency-anaemia-clinical-update
Primal Pictures Ltd: Clinical. (2010). Anemia. Retrieved from http://www.primaonlinelearning.com