Plague: Epidemiology, Pathogenesis, Clinical Manifestations, Diagnosis, Treatment And Prevention
Buboes In Plague

Epidemiology And Pathogenesis Of Plague
This disease used to occur in the form of epidemics in the early parts of this century, but now its incidence is very rare. It is a disease of animals which is transmitted to man by the infected rat flea Xenopsylla cheopis. The causative organism is Yersinia pestis previously known as pasteuralia pestis. The organism remains viable for long periods in human sputum and dried flea feces when protected from sunlight and heat.
Epidemiology: Man gets the infection while handling the carcases of infected animals. Animals harbouring plague bacilli (rats, mongoose, rabbits etc) serve as long-term reservoirs and start off enzootics.
The infection persists as a chronic disease of wild rodents (sylvatic plague) and it is maintained by the insect vector. Epizootics breakout periodically and from animals the disease spreads to man, so also from man to man.
Human epidermics usually arise from infected domestic rodents such as Rattus norvegius, Rattus rattus and Mus musculus. The common rat flea Xenopsylla cheopis gets infected by taking blood from the infected animal and transmits the organisms to man. In the alimentary tract of the flea, the organisms multiply and these regurgitate into the mouth parts when the flea bites its victim. Organisms are also passed in the feces of the flea, which may be inhaled. Bubonic plague develops as a result of infection from the flea. Pneumonic plague can be transmitted by droplet infection from man to man or by inhalation of dried flea feces. Under suitable conditions the fleas live for 1 to 2 years and may remain infective for prolonged periods.
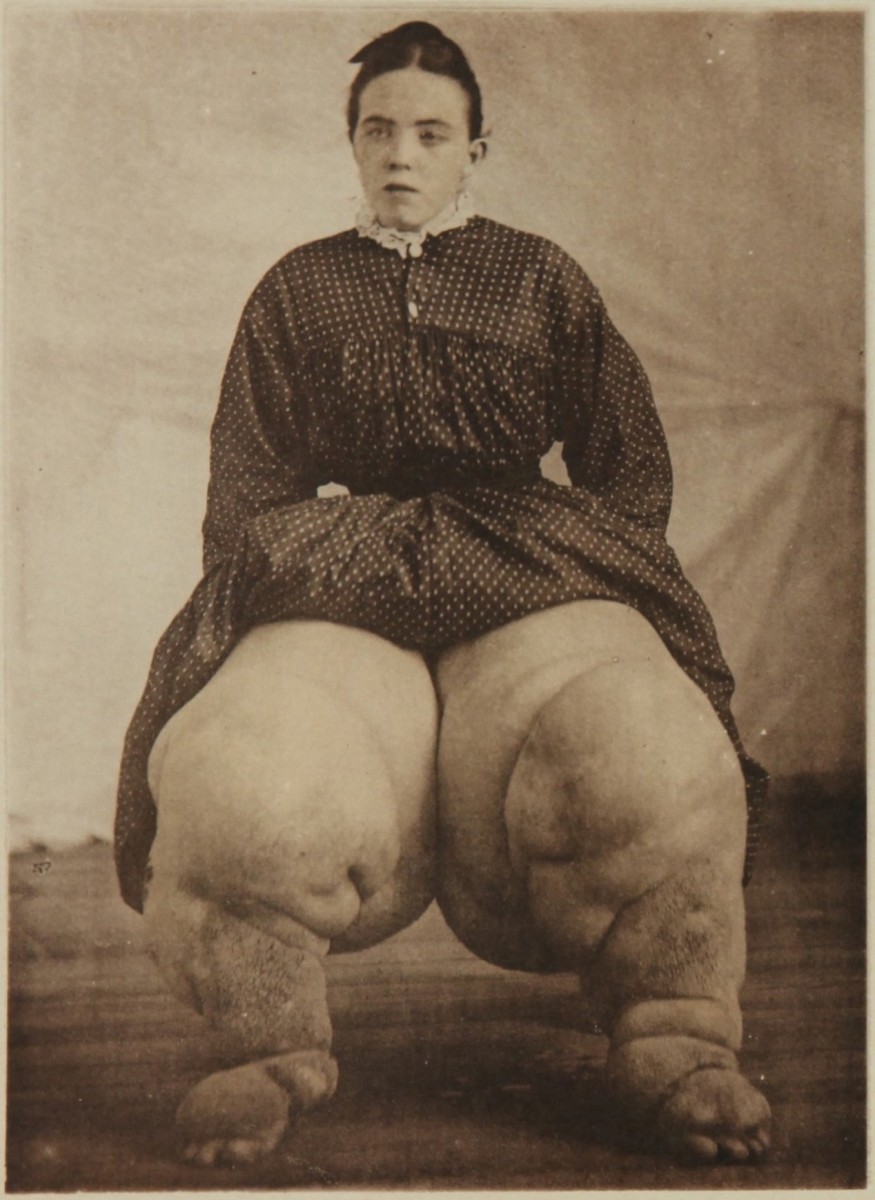
Pathogenesis: The organisms enter through the skin. At the site of entry, a papule or pustule may form. The bacilli reach the local lymph nodes which enlarge and suppurate. This constitutes the bubo. Bacilli proliferate and enter the blood stream to produce metastatic lesions in other lymph nodes, liver, Kidneys, meninges, brain and lungs. The spleen may be enlarged twice or thrice its normal size. In primary pneumonic plague, the organisms reach the lungs through the respiratory tract.
A Plague Infected patient

Infectious Diseases
Clinical Manifestations Of Plague
General symptoms: These include abrupt onset of high fever, tachycardia, malaise and backache. The patient is toxic and delirious.
Bubonic plague: Incubation period is 2 to 6 days. It begins with fever and lymphadenopathy. Buboes are seen most frequently in the inguinal or axillary regions. The buboes may slowly suppurate and discharge the contents. Death may occur due to peripheral circulatory failure.
The term “pestis minor” refers to milder cases seen during epidemics. These present only with buboes which suppurate and discharge in due course or may resolve without significant systemic manifestations.
Septicemic plague: Primary septicemic plague resembles severe bubonic plague with sudden onset of chills, fever, tachycardia, headache, vomiting and delirium. Several organs may be affected. Death may occur within a few days before localizing lesions are evident.
Plague pneumonia: Two types of pneumonia occur in plague- primary and secondary types. In the former case, the organisms reach the lungs by inhalation, and in the latter case, the organisms reach the lungs through the blood stream. The primary form is more fulminant and rapidly fatal. The onset is abrupt with high fever, tachycardia and dyspnea. In comparison to the severity of symptoms and respiratory distress, physical signs are less marked. Sputum may be scanty or bloodstained and frothy.
Diagnosis: Clinically, plague should be suspected in circumstances where the possibility of human contact with dead rates or other rodents exists. Diagnosis is confirmed by demonstrating the organisms by smear, cultures or animal inoculation studies. The bubo-fluid can be aspirated and stained for the organisms. Sputum can be stained for the organisms and cultured. The organisms appear as Gram-negative bipolar staining short rods. In septicemic plague, blood culture yields the organisms. Sometimes, suitably stained blood films may also reveal the bacilli. There is neutrophil leuckocytosis. Specific antibodies develop in patients who recover from the disease.
Differential diagnosis: Early treatment with antibiotics is very effective. The organism responds to large disease of streptomycin, chloramphenicol and tetracycline. Streptomycin is given in a dose of 0.5g every 4 hours for two days and then 0.5 g every 6 hours for 10 days.
Prognosis: Prognosis is grave in septicemic and pneumonic varieties with a mortality of 60 to 90% in the pre-antibiotic era. In the case of bubonic plague, the mortality ranges from 10 to 30%. Modern antibiotic therapy has improved the prognosis considerably.
Prevention: Preventive measures include elimination of the rodent population and improvement in living standards. The fleas can be eliminated by the use of DDT or other insecticides. A heat-killed vaccine (Haffkine) is available for immunizing the population at risk. An aerosol vaccine is also under use.
Persons exposed to this infection can be protected with sulphadiazine 6g daily or tetracycline 2g daily for a period of 10 days.
© 2014 Funom Theophilus Makama