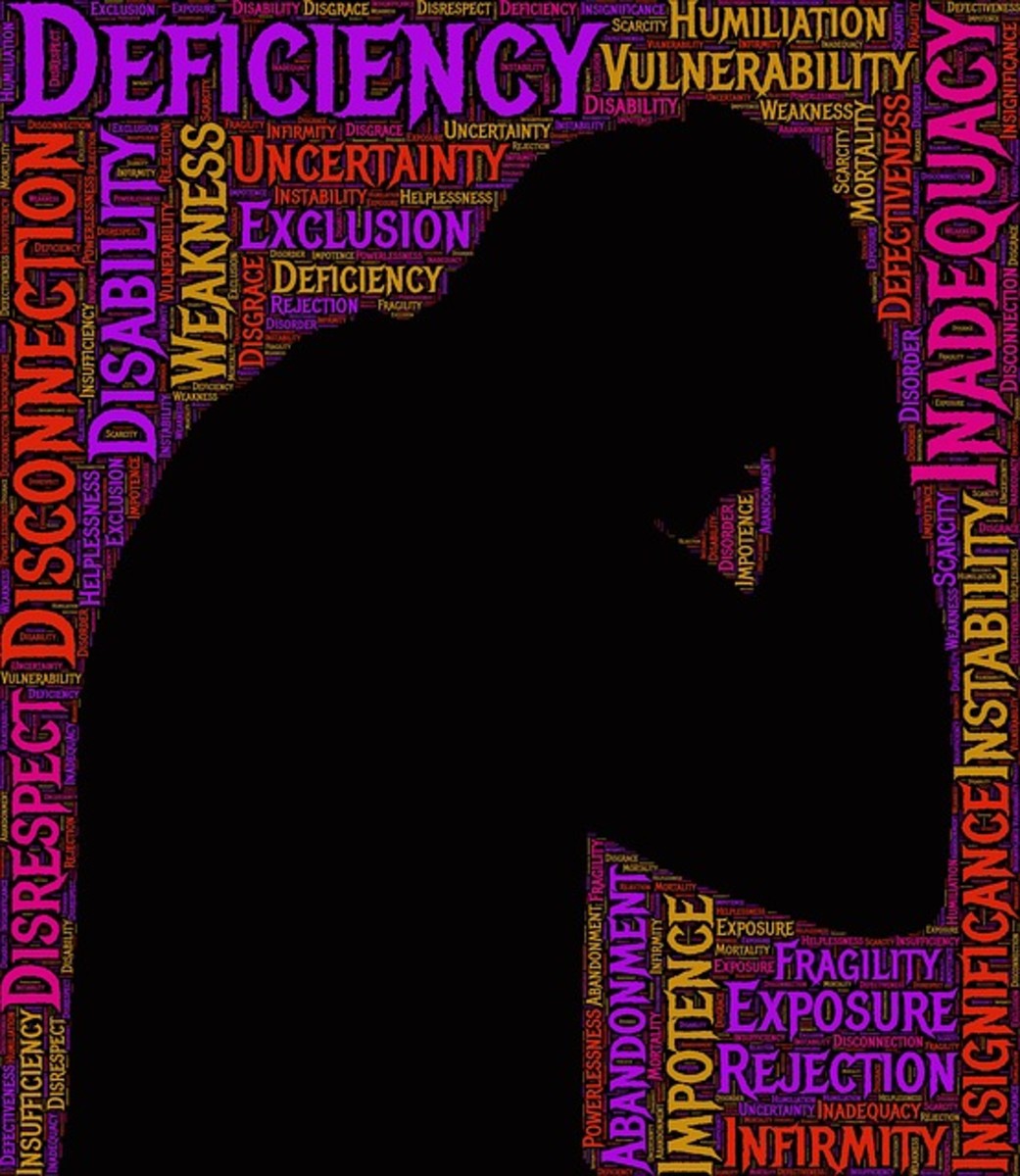
Post-natal depression symptoms: what it is and how to deal with it.
The mental agony of post-natal depression.
It is estimated that between 10 and 15 women out of every 100 are unlucky enough to get post-natal depression after childbirth. The risk is higher if they were already susceptible to bouts of depression before pregnancy.
For many women having post-natal depression is a shameful thing, bearing the stigma of a mental illness. The shame is greatly compounded by the fact that they feel guilty that they cannot enjoy their child as much as they expected they would.
They feel they are not the wonderful mother they thought they would be and, perhaps worse, they feel they are not the mother that our society seems to expect them to be.

The dangers of hiding post-natal depression.
Sadly, the shame of what these women see as ‘unnatural feelings' can lead many mothers to hide their symptoms from their family, friends and health workers, the very people who may be able to help them effectively.
The one person who tends to lose out most is the innocent baby caught up in the middle of what can be a highly confusing and emotional time for the mother.
Post-natal depression can have long term effects on a child's emotional development which the mother may never be able to assuage no matter how much love and time is subsequently given once the mother has recovered.
Having postnatal depression (PND) is most certainly nothing to be ashamed of but it is vital that prompt action is taken to tackle it.
The perfect mother ...
... does not exist. Truly. Despite the best efforts of magazines and television to persuade us that we will bloom during pregnancy, come out of labour looking flushed and provocatively tousled with eyeliner still in place and then go on to be the glamorous, capable 'mom' that every child is expected to have, real life is just not like that.
This scenario is an unrealistic fantasy for most women and midwives should be honest with the prospective mothers in their charge. Whilst there is no need to frighten women with tales of the travails of labour there is a definite need to prepare them for the possible after-effects of it.
Being honest about motherhood.
It is a fact that whilst most of us do realise that you can be fiendishly sick during pregnancy, that you do feel bloated and uncomfortable and that giving birth is definitely going to be the proverbial 'pain in the ass', few of us will ever admit to being what we see as an ‘inadequate' mother.
This is one hurdle prospective mothers need to get over as few of us will ever live up to the expectations we have of motherhood. Being a good mother can still feel as if you have the word 'guilt' tattooed across your forehead forever and the best we can do is just ... the best we can do.
Mothers are human beings too with all the mistakes and bad judgements that being human entails.
Symptoms of postnatal depression.
To give midwives their due most of them do warn new mothers that they may get the 'baby blues' a few days after giving birth.
This feeling is easily identifiable by its mood swings and emotions can include tearfulness, irritability, anxiety, listlessness and depression. It is a natural phenomena and lasts for only a few days.
But this twee little phrase does not cover the full-on version of post-natal depression and telling the difference between the two is vital as the earlier help is sought the sooner the symptoms can be tackled.
Any ‘baby blues’ that last longer than ten days are cause for concern although most PND starts one or two months after giving birth. It can also start quite a few months afterwards so it is important for new mothers to be aware of their mental state.
The warning signs to look out for are :
- Irritability
-
Low mood/depression - often weepy - sometimes at specific times of the day
-
Tiredness - difficult to identify from normal new baby sleep deprivation
-
Sleeplessness - despite often being dog-tired
-
Anxiety - about your baby's health etc. and your own inabilities as a mother
-
Inability to feel anything for your child - this is considered so socially unacceptable that it naturally ramps up the anxiety levels
-
Changes to eating habits - forgetting to eat/not feeling hungry or, conversely, comfort eating
-
Lack of interest in sex - this however may simply be a natural reaction to tiredness
-
Disinterest in life in general/lack of hope - this can be as deep as despair
-
Avoidance of other people - specifically apparently 'successful' mothers
-
Negative thoughts about yourself and the baby
-
Panic attacks
-
Thoughts of suicide - often as an alternative to the thought that you might harm your baby.
- Psychotic symptoms (Pueperal or Postpartum Psychosis) - which can include hallucinating/hearing voices and irrational beliefs.
What is puerperal psychosis?
Pueperal psychosis is the most severe form of PND and requires non-negotiable and immediate medical intervention. It can come on very quickly after childbirth and can be life-threatening.
Fortunately, only 1 in 1000 women will go on to develop this form of PND and it is possible to make a full recovery.


How to deal with PND.
This will vary from sufferer to sufferer. From personal experience I would offer the following advice:
-
Talk honestly to your midwife/health visitor/GP
Do this immediately you think things are not right. Tell them how you feel and describe your symptoms accurately, remember this will be confidential. This is not the time to hide your emotions.
The more you tell them the more easily they can find a way of helping you through PND in as short a time as possible. Accept their advice. Take the antidepressants, go to counselling/group therapy etc. Do whatever it takes ...
-
Ask for help from your husband, friends and family.
This may be the single hardest thing to do as it often seems like an admission of inadequacy and many of us are too proud to admit this ... especially to our mothers-in-law.
- Give up any idea of being 'Supermum' for the time being.
This is when you must remember that you will get through this given time and you will be able to regain your credibility as a mother. Right now your immediate concern is to just get through it.
Always remember: 'This too shall pass'. Write this on a Post-it note and stick it on the fridge and really 'see' it everyday so that you take it to heart.
- Distract yourself.
If you find it too hard to mix with the other, apparently more successful, mothers do something that pleases you for a short time everyday, usually whilst baby is napping. Be creative.
Creativity accesses a different area of your brain and you can find yourself 'in the flow' as it were. This is where you can lose track of time and forget your problems for a while.
Writing and painting can be extremely helpful 'right-brain' pastimes for this sort of self-healing. It doesn’t have to be award-winning, you are only doing it to help yourself. Once you are through PND, who knows?
- Do not beat yourself up.
Please, this is so important. You did not fail. For most of us there is no way we could have done anything different to avoid it. It is simply a lottery.
Give yourself love and understanding and know deep down that you will get through it intact and return to being your loveable, sunny self.
My credentials for writing this piece.
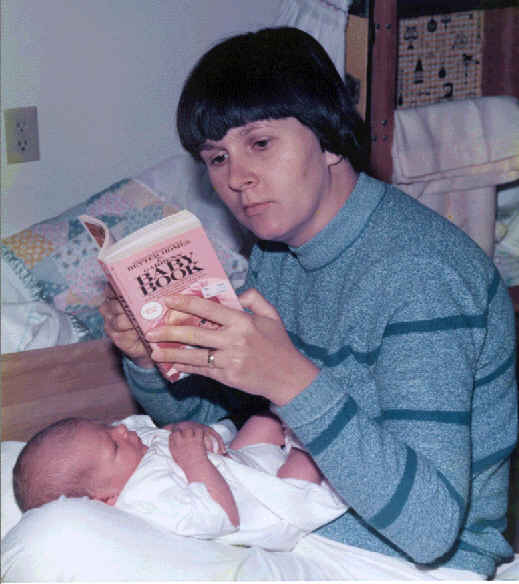
Sadly I have the correct credentials for writing this piece as I suffered with PND with my first child. Nothing had prepared me for it as my pregnancy was wonderfully relaxed and easy and I supremely happy and looking forward to my child's arrival.
She arrived a month early, a breech birth after 24 hours in labour and was whisked away to a warm nursery. I was not given her to hold at birth and I believe I lost the chance to bond with her.
At the time I needed to persuade myself that getting PND was not my fault and this was the justification I gave myself.
The value of good medical care.
My doctor was my lifeline for many months. He called to check on me everyday despite censure from his senior practice partner over the amount of time he spent with me. He told me, over and over again, that I would get through it.
'This too shall pass' became my mantra, even as I begged my doctor to section me and commit me to an insane asylum because I feared that I might harm my daughter. I often contemplated suicide because I felt that my not existing would be best for her.
Looking back, even from a distance of almost forty years, all my memories of that time are seen 'through a glass darkly’ and each remembered scene is surrounded by a diffused and shadowy border.
Eventually I was persuaded by my doctor to go as an out-patient to the nearest mental hospital (we had them in those days) and join a group therapy class to talk about my problems. I went but I couldn’t bring myself to tell the group about my ‘shameful’ disorder and I didn’t see how talking about it could help me.
Despite my resistance I still went once a fortnight in the hope that I would have some sort of epiphany and obtain some sort of healing.
The epiphany comes.
One day I came away thinking as usual how pointless it all was when I suddenly found myself determined to sort it out for myself. I felt a strange wash of strength flood through me which was so startling that I knew immediately that I was starting to recover.
I had survived and my daughter had survived and we would go on together but I had lost a lot of valuable time with her. In all it had taken me well over a year to get through it.
The constant memory of that lost year meant that it took me five years to pluck up the courage to have another baby. This time I planned everything as carefully as I could in an attempt to try to avoid post-natal depression.
I made many stipulations to my doctor about the delivery in the hope that I would at least bond with my child this time and, despite complications towards the end of my pregnancy and during the birth, I did manage to hold my son from the moment of his birth.
I was on cloud nine, I had my child, my baby boy in my arms. I was being given the chance to do it right this time.
The memory of the bliss of that moment lasts to this day ...
And just in case you underestimate the seriousness of PND ...
- BBC News - Stacey Solomon: Why I thought I was the 'worst mum'
There is still a stigma surrounding post-natal depression, with some young women afraid to speak out or ask for help says singer and TV personality Stacey Solomon, as she shares her experience of the illness. - BBC News - Postnatal depression mothers 'need more support'
The search for a mother-of-three suffering with post-natal depression (PND) ended yesterday after police found a body. Bethany Reynolds, who had PND with her first son and antenatal with her second son, reflects on the disease and Rachel Dobson, who - Postnatal Depression - The Angela Harrison Charitable Trust
- PANDAS - Help & support with Pre (ante), Postnatal depression & Psychosis
PANDAS - Pre (Antenatal), Postnatal depression & Psychosis, support groups, helpline and email support.