Recognizing RLS (restless leg syndrome)

A person suffering from restless legs syndrome (RLS) is aware of the fact, but may not seek help for the condition. Like fibromyalgia, this is a disorder which cannot be quantitatively verified. The person has uncomfortable feelings in his calves, thighs or feet which seem to be impossible to allay except by walking, stretching or exercising. Soon after the relief of exercise, the symptom returns. The discomfort arises after rest, either from sitting for a long period of time, or after falling asleep. This restlessness interrupts the sleep, so it is often referred to as a sleep disorder.
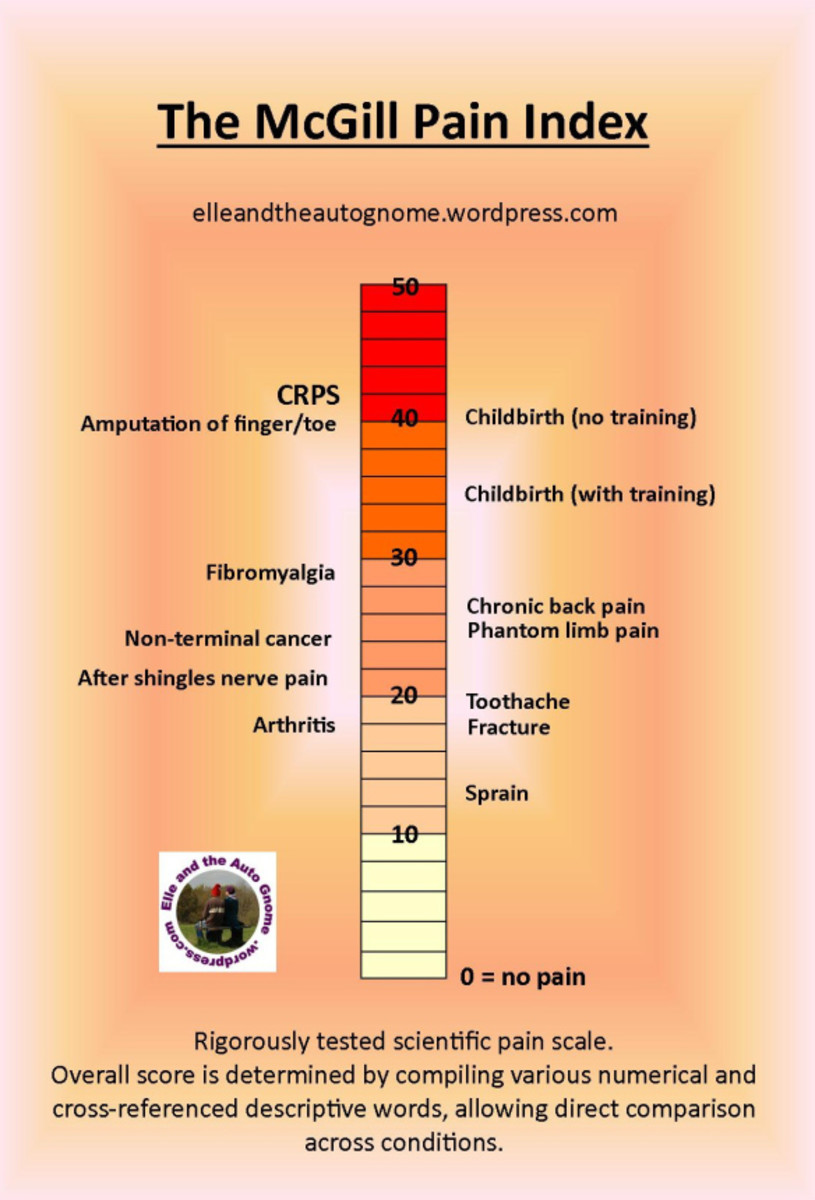
Sufferers describe the symptoms in many different ways – itching, burning, pins and needles, “creepy crawly” feelings, throbbing, pulling, tugging, gnawing or downright pain. These discomforts are often mild, but can become intolerable, at which point the person will finally give in and seek medical help. The symptoms can be experienced as young as childhood, but appear to be most common as one gets older, especially after the age of forty. It is believed to affect about 10% of the population, but this is only a guess; due to the nebulous feelings, many people do not report it to their doctors. Symptoms can come and go, always more severe in the evening or night and nonexistent in the morning. Slightly more women tend to suffer from this syndrome, but it does affect both genders and may occur in other body parts.
The sufferer can hesitate to run to a doctor with the problem, for fear of not being taken seriously. Doctors may credit the problem to stress, nervousness, insomnia or muscle cramps. Recent attention from the pharmaceutical community has lent some credence to the existence of a real problem. Probably the patient’s best advocate is himself. By keeping a simple diary of incidents, the patient can find those things which may trigger the syndrome, such as being over tired, which causes a round-robin of restlessness, exercise and loss of sleep. On days when the patient has been walking a lot, there may be a remission of the symptoms. Some sleeping positions can aggravate the symptoms. Several studies indicate a genetic connection, so the patient should inquire within his family of others who may also suffer from the syndrome. The patient should note any occurrence which lasts an hour or more, and any occurrence in the upper legs or arms. He should note if it occurs during prolonged sitting, such as a road trip, classroom, movie theater or airline ride. He should also note if he is under stress or emotional upset.
Sometimes RLS is a side effect of certain drugs, so the patient should bring a list of those medications to the doctor. Antinausea drugs, antipsychotic drugs, antidepressants, and even allergy medications containing antihistamines are suspected of worsening if not causing RLS. The symptoms are recognized as being part of other illnesses such as diabetes and dopamine-related diseases such as Parkingson’s disease; there seems to be a relationship between restless legs and dopamine uptake. It is possible that a chemical imbalance of dopamine, which crosses the blood-brain barrier, may be at fault.
About the strongest suspicions of cause are related to the body’s iron uptake. Pregnancy’s high usage of iron (ferritin) may be the reason RLS arises during gestation and subsides after birth. The patient should monitor his intake of high-iron foods, and discuss iron supplements with the doctor. The Mayo Clinic and Johns Hopkins Hospital are currently studying iron treatment for RLS.
Other contributing factors can be peripheral neuropathy from chronic diseases such as diabetes and alcoholism as well as kidney failure. The patient should evaluate all these possible causes and then determine his next moves. He should approach treatment according to the severity of the syndrome. Even mild RLS causes daytime fatigue, unclear thinking and depression. There is a great deal the patient can do before turning to the medical profession, where it is often misdiagnosed, and where medication treatment has had limited success if any.
After determining which causes apply to himself, the patient can do a lot at home to cope with the situation and ease the symptoms. First, set up the bedroom as a comfortable place, retiring and rising at the same time each day. Use hot or cold packs on the legs to relax them (or try alternating the two), and practice gentle stretches, massage and warm baths before bed. During the day, make a decided effort to relax, perhaps with yoga or meditation to ease tension. Avoid alcohol, tobacco and caffeine, since they may aggravate the symptoms. Tell others about your condition, so that they will understand your pacing and standing when others sit. Don’t fight the urge to move – get up, move around, find a productive activity to achieve something while exercising. Take walking breaks when travelling. Adapt your workspace to work from a standing position by elevating the desktop. Begin and end your day with stretching or massage. Over-the-counter pain relievers such as ibuprofen can help. Try all of these and decide which to continue, since there is no “cure” for RLS and you are facing a permanent and possibly worsening syndrome. All the over-the-counter creams and pills being advertised seem to have no effect other than to legitimize the syndrome.
If these tactics are not sufficient, a visit to the doctor is in order. When medical help is sought, the doctor cannot diagnose this syndrome with any accuracy. What she can do is eliminate similar and more serious ailments as the cause of the symptom. Blood tests should be run, and a thorough history of the symptoms, family, and medications needs to be taken down and analyzed. Some doctors may request a sleep evaluation, watching for twitching or periodic limb movements during sleep.
A blood test to look for underlying nutritional deficiencies should be performed. Under the doctor’s eye (for complications of these and prescription medications) supplements may be suggested for iron, folic acid, vitamin B and magnesium. There are many types of prescription drugs being tried for RLS, but results are mixed and controversial, so if the doctor decides to opt for this treatment, it will probably be experimental in nature.
Restless leg syndrome has also been called Willis-Ekbom disease, after two of the physicians who studied the disorder in depth and encouraged further research. The patient can join the Willis-Ekbom Foundation (formerly the RLS Foundation) to get access to support and news by signing up here. Because of all the uncertainties and controversies over cause and treatment the patient himself needs to evaluate and handle this newly-recognized syndrome.
© 2014 Bonnie-Jean Rohner