Rhinosporidiosis And Aspergillosis: Etiology, Clinical Manifestations, Diagnosis And Treatment
The Clinical Manifestation Of Rhinosporidiosis

Rhinosporidiosis
It is a chronic localized proliferative lesion caused by Rhinosporidium seeberi which affects the mucous membranes of the nose, larynx, eyes, ears, mouth, genitalis, rectum and skin.
Etiology: The etiological agent which is most probably a fungus was included under the class phycomycetes. The source of infection is stagnant water or acquatic life. The disease is endemic in Sri Lanka and India, but only rarely seen in other parts of the world. Mode of infection is also not clearly known.
Pathology: Typical lesions are soft, nodular and polypoid with grayish-white areas over the surface. Chronic inflammatory cell infiltration may be demonstrable. Histology shows a large number of fungal spherules containing endospores, embedded in a stroma of vascular connective tissue.
Clinical Features
The incubation period is not clearly known. The patients often seek medical help only when polypoid masses have developed. The symptoms depend on the site of affection. Nasal cavity is affected most commonly. Symptoms include local pruritus, presence of mass, nasal block and epistaxis. The polyps are soft, pink, friable and easily bleeding on touch. Their sizes vary and they show small yellowish dots on the surface. Cutaneous lesions resemble warts and are initially painless but become painful later.
Diagnosis: It can be made clinically in endemic areas. Nasal discharge may show free spores demonstrable microscopically. Histology is confirmatory. Treatment consists of surgical removal.
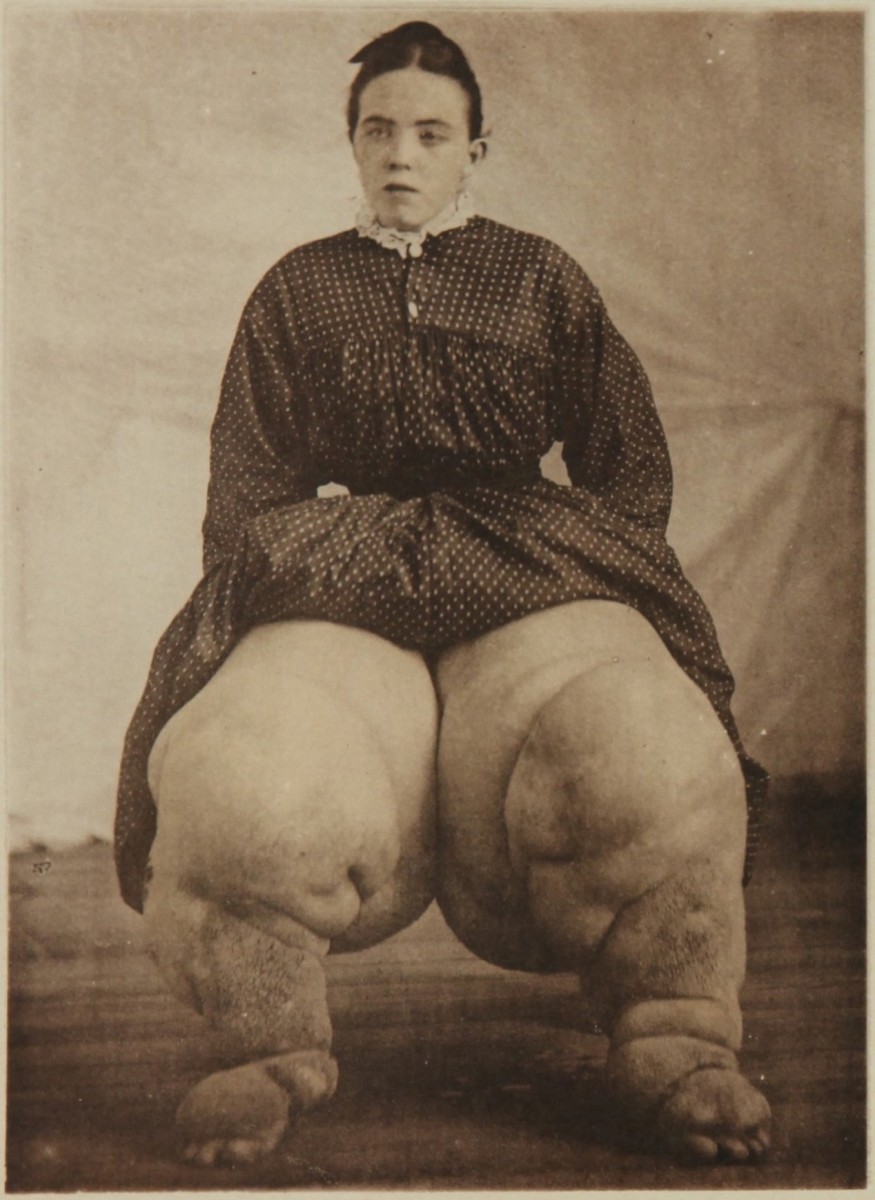
Foot Affected by Aspergillosis

Infectious Diseases
Aspergillosis
It is an opportunistic infection caused by Aspergillus fumigates which is occasionally invasive in man, when general resistance is lowered or local disease favours superinfection. Aspergilli are very widespread in nature and their spores are found in dust. Both superficial and systemic lesions may develop. The commonest superficial lesion is otomycosis. Systemic infection may be pulmonary or disseminated. Major portal of entry is the respiratory tract.
Pulmonary form: Allergic alveolitis may develop due to inhalation of fungal spores in sensitized individuals. Aspergillus may grow in the bronchi to produce bronchopulmonary disease. The hyphae may obstruct the lumen. Healed tuberculous cavities or other types of cavities may be the seat of colonization by the fungus. The mycelia grow to form a tangled fungal ball which is recognizable in X-rays. It may remain asymptomatic or may cause massive hemoptysis. Invasive aspergillosis occurring in immunosuppressed individuals leads to widespread pulmonary necrosis with marked systemic symptoms.
Other sites of lesion are the central nervous system and naso-labial cavities. Diagnosis can be made by histological demonstration of the fungus and isolation of the organism from the exudates. Since Aspergillus is a common contaminant in respiratory secretions, mere isolation does not prove its pathogenic role. Precipitating antibodies can be demonstrated by gel diffusion test and this test is of great value in diagnosis.
Treatment: Amphotericin B in a dose of 1 mg/Kg/day is effective in systemic aspergilloma. Amphotericin B and 5-flurocytosine are effective in CNS disease. The underlying predisposing factor should be attended to. Cavities containing aspergilloma producing intractable hemoptysis have to be removed surgically. Other drugs like Clotrimazole which are also effective in vitro are being evaluated.
© 2014 Funom Theophilus Makama