Shigella Infections (Bacterial Dysentery): Bacteriology, Epidemiology, Clinical Manifestations And Complications
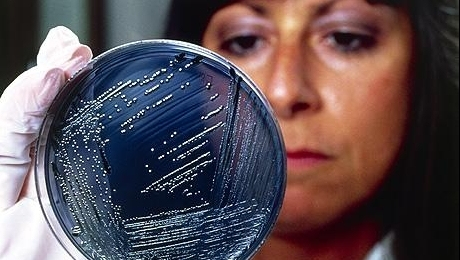
Diagnosing Shigellosis
Epidemiology And Pathology
Bacterial dysentery is caused by infection by organisms belonging to the genus Shigella and clinically characterized by diarrhea, (stools contain mucus and gross blood) fever, vomiting and abdominal pain. The disease is very common in the tropics where environmental sanitation is poor and food hygiene is low.
Bacteriology: Shigella are classified into four species based on the biochemical and serological features. These are Shigella dysenteriae (types I and II, i.e, S. Shigae and S. Schmitzii), S. flexneri, S. sonnei and S. boydii. Shigella shigae produces a powerful exotoxin with neurotoxic, enterotoxic and cytotoxic effects causing the most serious infection. Shigella sonnei is the mildest among this group.
Epidemiology: The organisms are spread from man to man by ingestion in food or water which may be contaminated directly or indirectly. Man is the main host and organisms are excreted in the feces of cases and carriers. In developing countries, especially in India, S. flexneri is the commonest pathogen accounting for 50 to 85% of cases. Shigella sonnei accounts for 2 to 24%, S. dysenteriae for 8 to 25% and S. boydii for 0 to 8%. Overcrowding and adverse conditions like famine and war lead to outbreaks. Apart from contamination of food and water, the organisms can be acquired through formites, lavatory seats and door handles of privies.
Pathogenesis and pathology: The organisms adhere to the mucosal surface after reaching the colon and penetrate the epithelial cell lining where they multiply. It is rare for the infection to extend deep. The entire colon may be affected. A fibrinous exudates is formed. Shallow ulcers are formed due to necrosis of the mucosa. The clinical manifestations are mainly due to the invasiveness and production of intestinal lesions. Toxins are produced which are responsible for some of the systemic manifestations. Sometimes, large areas of the mucosa may be necrosed and these are passed as intestinal casts. Loss of blood and electrolytes worsen the clinical picture.
Incubation Period Of Shigellosis

Infectious Diseases
Clinical Manifestations
The incubation period varies from 1 to 7 days and in severe cases, it may be as short as a few hours. The onset is abrupt with abdominal discomfort, nausea, vomiting, fever and diarrhea. The stools passed early in the disease contain fecal material but subsequently, they consist almost entirely of tenacious blood-stained mucus. Microscopic examination reveals large numbers of erythrocytes, polymorphs and macrophages and these are collectively called cellular exudates. Urgency, griping and tenesmus are marked. The number of stools exceed 20 to 30 in 24 hours and in severe cases, there may be a continuous diarrhea. In the ordinary case, symptoms subside after a week. Some cases may be mild and ambulatory. Fulminant dysentery is characterized by toxemia, severe thirst, electrolyte loss, prostration and severe bloody diarrhea. In this group, mortality is very high.
Complications: General complications are dehydration, electrolyte imbalance, circulatory failure and renal failure.
Local complications consist of intestinal perforation, rectal bleeding, paralytic ileus, intussusceptions and passage of intestinal casts. Pneumoperitoneam, portal pyemia and multiple abscesses in the liver may occur rarely. Sequelae include arthritis (post- dysenteric arthritis), conjunctivitis, iritis and peripheral neuropathy.
© 2014 Funom Theophilus Makama