Shigella Infections (Bacterial Dysentery): The Clinical Significance Of Its Diagnosis, Treatment And Prevention
Sometimes Amebic Dysentery And Bacillary Dysentery Co-exist

Diagnosis Of Bacterial Dysentery
Clinically, the disease should be suspected when dysentery occurs with fever and signs of toxemia. Diagnosis is confirmed by microscopic examination of stools which reveals cellular exudates predominantly. The organisms are isolated by culture of rectal swab or fresh feces transported to the laboratory in special medium. Sigmoidoscopy reveals superficialulcer all along the rectal mucosa, the intervening areas also show hyperemia.
Differential Diagnosis: This includes amebic dysentery, staphylococcal food poisoning, salmonellosis, viral enteritis cholera, fulminant ulcerative colitis, and necrotizing enterocolitis. In amoebic dysentery, which is so common in developing countries, the number of stools rarely exceed 15 per day. Examination of stools will help in establishing amebic dysentery by demonstrating E.histolytica. Sometimes amebic dysentery and bacillary dysentery co-exist.
Staphylococcal food poisoning is characterized by nausea, vomiting and more watery stools. Cholera and gastroenteritis are suspected when the stools are watery without blood and mucus. Acute attacks of ulcerative colitis may closely resemble bacterial dysentery. Presence of other signs of ulcerative colitis, recurrence over long periods, occurrence in adults, and sigmoidoscopic appearances and biopsy should suggest the diagnosis. Local conditions in the distal large intestine such as carcinoma, diverticulitis and proctocolitis should be differentiated by suitable investigations.
Differentiation Between Bacterial And Amebic Dysentery
Bacterial dysentery
| Amebic dysentery
| |
|---|---|---|
Onset
| Sudden
| Slow
|
Incubation Period
| A few days
| Weeks to months
|
Number of stools in 24 hours
| Over 20
| Less than 15
|
Nature of feces
| Mucus And Blood
| Fecal matter mixed with mucus and blood
|
Reaction of feces
| Alkaline
| Acidic
|
General symptomatology
| Dehydration and toxemia are marked
| General symptoms are milder
|
Course
| Acute with higher mortality
| More subacute or chronic, tends to be recurrent
|
Microscopic examination of feces
| Erythrocytes and cellular exudates
| Erythrocytes and a few leucocytes; Entamoeba histiolytica are demonstrable in fresh smears
|
Culture
| Amebae can be cultured by special techniques
|
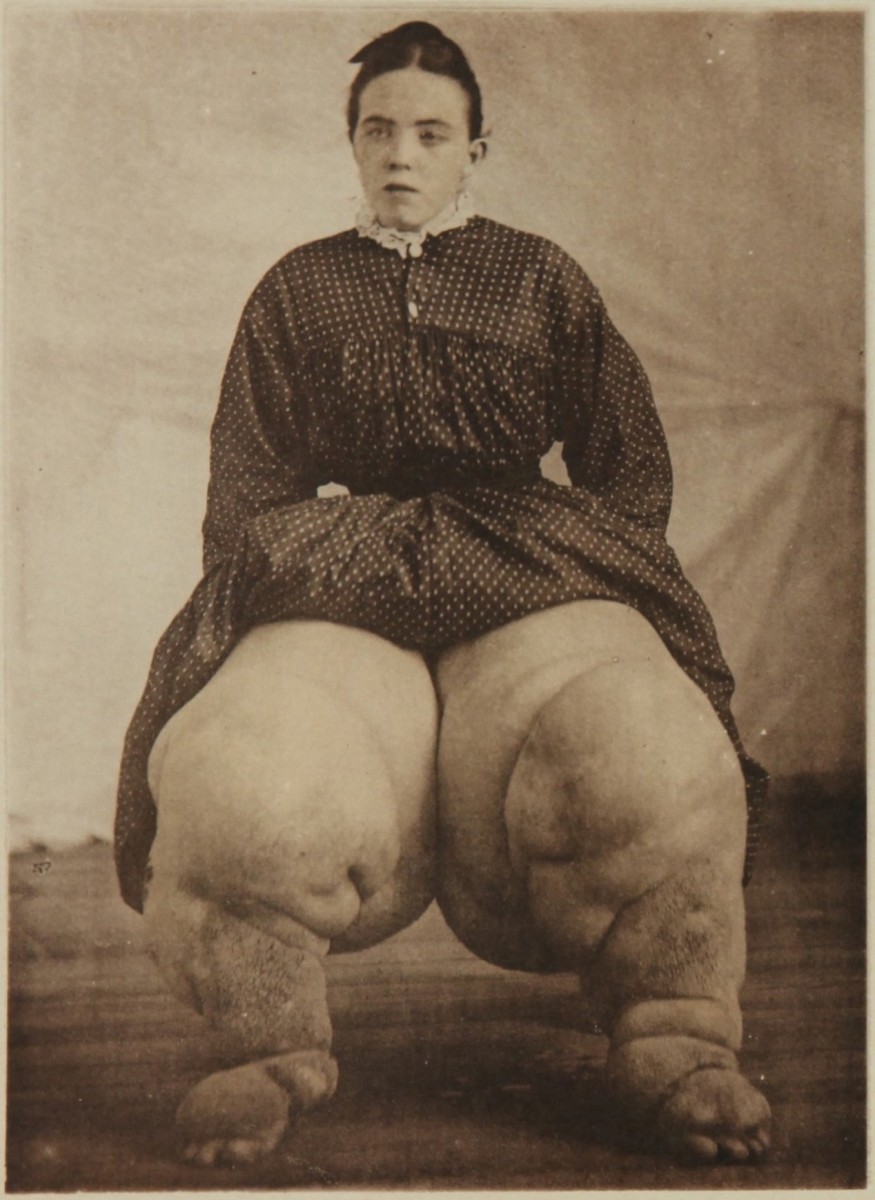
A Pediatric Case Of Dysentery

Treatment Of Shigellosis
In severe cases, the patient should be hospitalized. General treatment is aimed at correction of dehydration and toxemia. Hypokalemia may develop due to loss of excessive quantities of mucus which is rich in potassium. Blood transfusion may be required in severe cases where blood loss is considerable. Oral administration of fluid and nutrients should be maintained. The diet should consist of high calorie, low-fat and non-residue foods. Curds (yoghurt), buttermilk, banana, apple, cereals and honey are usually well tolerated.
Drug treatment: Till a decade ago, many strains of shigella used to be sensitive to non-absorbable sulphonamides and these drugs were employed routinely. At present, many strains prevalent in developing countries are drug resistant. Being a self-limiting disease, specific antibacterial therapy may not be required in mild cases. When the condition is severe and general toxemia is present, combinations such as erythromycin 500 mg thrice daily or tetracycline, 250 mg every 6 hours with cotrimoxazole 1g thrice daily may be beneficial. If there is evidence of severe toxemia or systemic infection by other gut organisms, gentamicin may be given intravenously or intramuscularly in disease of 80 mg every 8 hours. Though, there is no objective evidence that antibiotics hasten recovery in a severely toxic patient, these drugs are employed since empirical observation do favour them. Severe abdominal pain can be allayed by the used of antispasmodics like propantheline bromide in a dose of 15 mg given orally or atropine 0.5 mg intramuscularly.
Prevention: Personal and environmental hygiene should be strictly enforced. Oral vaccines which offer type-specific local immunity have been developed. The presence of several serotypes of Shigella in the same community seems to reduce the importance of the vaccine. These vaccines are not available for general use in India in particular.
Cases of shigellosis should be followed up for detecting the carrier state which is usually short-lived and subsides within 2 to 4 weeks.
© 2014 Funom Theophilus Makama