Sinus Tachycardia.things You Need to Know About It

What is sinus Tachycardia?
Sinus tachycardia is a sinus rhythm with an ascending rate of impulses, defined as a rate greater than 100 beats/min in an average adult. The normal resting heart rate in the average male adult ranges from 60–100 beats/minute and women 60-90beats /minuteNote that the normal heart rate varies with age, with infants having normal heart rate of 110–150 bpm, in contrast to the elderly, who have slower Mechanism.The normal adult heart rate, arising from the sinoatrial (SA) node, has been considered historically to range from 60 to 100 beats per minute, with sinus tachycardia being defined as a sinus rhythm with a rate exceeding 100 beats per minute. However, the "normal" heart rate is, in part, the result of the complex interplay between the sympathetic and parasympathetic nervous systems.
Definition of Sinus Tachycardia:(NORMAL)
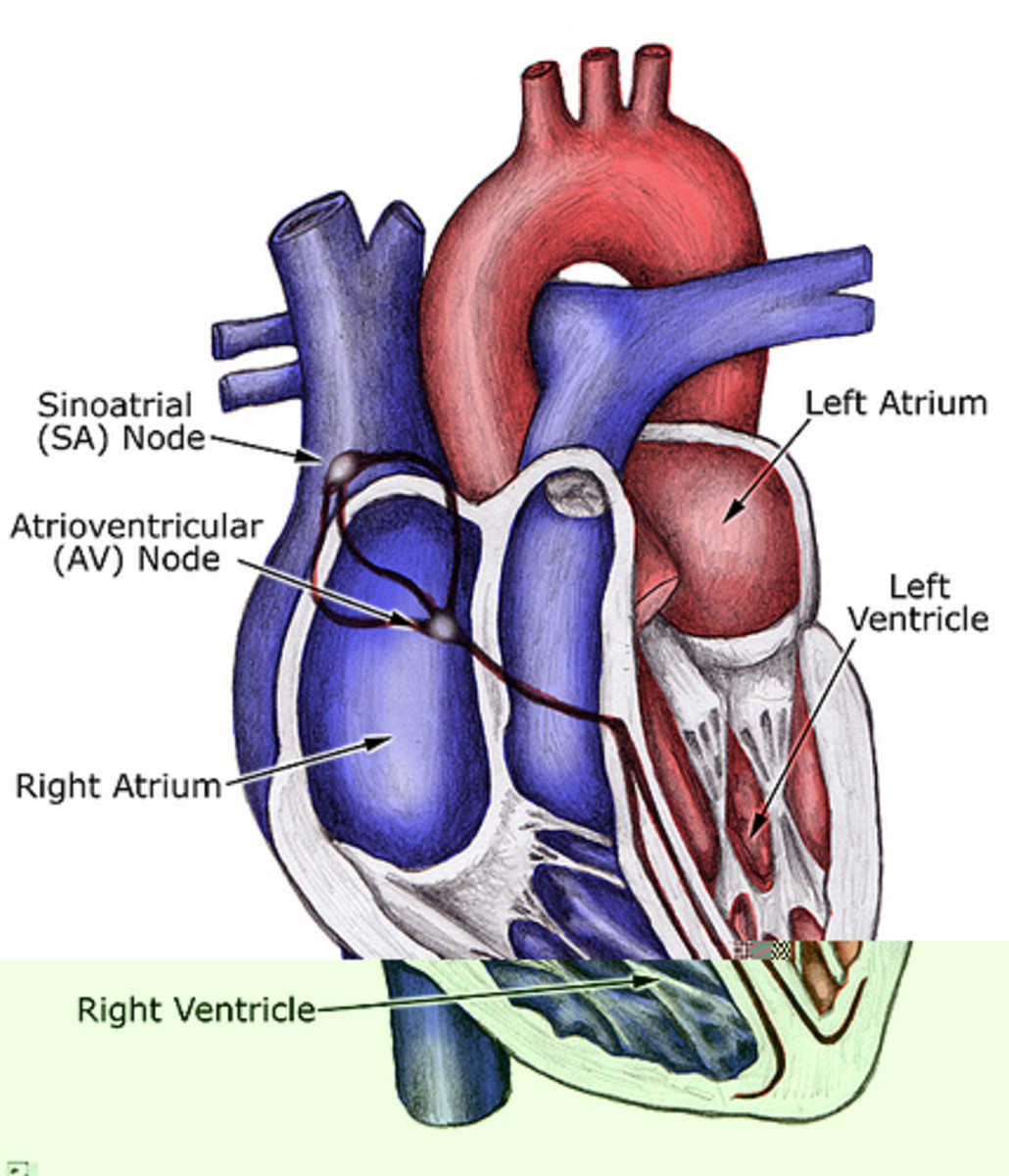
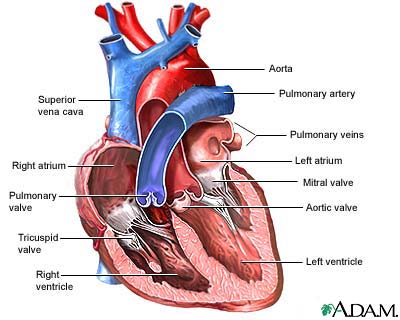
In a normal heart rhythm, the sinus node generates an electrical impulse which travels through the right and left atrial muscles producing electrical changes which is represented on the electrocardiogram (ECG) by the p-wave. The electrical impulse then continue to travel through specialized tissue known as the atrioventricular node, which conducts electricity at a slower pace. This will create a pause (PR interval) before the ventricles are stimulated. This pause is helpful since it allows blood to be emptied into the ventricles from the atria prior to ventricular contraction to propel blood out into the body. The ventricular contraction is represented electrically on the ECG by the QRS complex of waves. This is followed by the T-wave which represents the electrical changes in the ventricles as they are relaxing. The cardiac cycle after a short pause repeats itself, and so on.
Normal sinus Tachycardia not only indicate that the rhythm is normally generated by the sinus node and traveling in a normal fashion in the heart, but also that the heart rate, i.e. the rate at which the sinus node is generating impulses is within normal limits. There is no one normal heart rate, but this varies by age. It is normal for a newborn to have a heart rate up to 150 beats per minute, while a child of five years of age may have a heart rate of 100 beats per minute. The adult's heart rate is even slower at about 60-80 beats per minute.
Your heart rate is controlled by electrical signals sent across heart tissues. Tachycardia occurs when an abnormality in the heart produces rapid electrical signals that quicken the heart rate, which is normally about 60 to 100 beats a minute at rest.
In some cases, tachycardia may cause no symptoms or complications. But if left untreated, tachycardia can disrupt normal heart function and lead to serious complications, including
- Heart failure
- Angina
- Stroke
- Blood vessels getting damagaed
Inappropriate Sinus Tachycardia:
Inappropriate Sinus Tachycardia (IST) is a condition in which an individual’s resting heart rate is abnormally high – greater than 100 beats per minute or rapidly accelerating to over 100 beats per minute without an identifiable cause; although small amounts of exercise, emotional or physical stress are triggering factors. An electrocardiogram (EKG) does not show any abnormalities as IST arises within the sinus node where the normal heart rhythm is generated. It is a relatively new disorder (first recognized in the late 1970s) that is underappreciated by many in the medical profession and many doctors consider it to be a psychological condition. Individuals with this condition can find themselves increasingly disabled and experiencing high levels of anxiety. IST is not a life threatening condition but it can be very debilitating. Where sinus tachycardia is identified it is important to rule out other treatable conditions before making the diagnosis of IST – it may be that there is a curable cause. IST is frequently mistaken for another condition called Postural Tachycardia Syndrome (PoTS). More information on PoTS can be found by visiting the Syncope Trust And Reflex anoxic Seizures
IST is primarily experienced by young women in their thirties, who may have been suffering symptoms for a few years. The main symptoms of IST include:
- Palpitations
- Shortness of breath
- Exercise intolerance
- Fatigue
- Resting heart rate of greater than 100bpm
- Sleeping heart rate of 70 – 90bpm
- Minimal exertion, heart rate will rapidly reach 150bpm
- Drop in blood pressure upon standing
- Blurred vision
- Dizziness
- Syncope
- Pre-syncope
- Sweating
With IST, the resting heart rate is most often greater than 100 beats per minute, but during deep sleep, it may drop to 80 or 90 beats per minute, or even lower. With even minimal exertion the heart rate rapidly accelerates to as high as 140 or 150 beats per minute. Palpitations are a prominent symptom even though (as is often the case) there are no "abnormal" heart beats occurring. (That is, each heartbeat arises from the sinus node, just as with the normal heart rhythm.) The symptoms experienced by sufferers of IST can be quite disabling and anxiety-producing.
IST was recognized as a syndrome only as recently as 1979 and has been generally accepted as a true medical entity only since the late 1980s. And even today, while IST is fully recognized as a genuine medical condition by every university medical center, many practicing physicians either haven't heard of it or write it off as a psychological problem (namely, "anxiety").
The Type of Tachycardia:
There are many different types of abnormal tachycardia. They're classified according to the origin and cause of the abnormally fast heartbeat. Common types of tachycardia include:
Atrial fibrillation:
Atrial fibrillation causes the heart to beat much faster than normal, and the upper and lower chambers of the heart do not work together. When this happens, the lower chambers do not fill completely or pump enough blood to the lungs and body. This can make you feel tired or dizzy, or you may notice heart palpitations or chest pain. Blood also pools in the heart, which increases your risk of having a stroke or other complications. Atrial fibrillation can also occur without any signs or symptoms. Untreated fibrillation can lead to serious and even life-threatening complications.
Sometimes atrial fibrillation goes away on its own. For some people, atrial fibrillation is an ongoing heart problem that lasts for years. Over time, it may happen more often and last longer. Treatment restores normal heart rhythms, helps control symptoms, and prevents complications. Your doctor may recommend medicines, medical procedures, and lifestyle changes to treat your atrial fibrillation.
In atrial fibrillation, the heart rate is irregular and can sometimes be very fast. In some cases, it can be considerably higher than 100 beats a minute.
This can cause problems including dizziness, shortness of breath and tiredness.
You may be aware of noticeable heart palpitations, where your heart feels like it's pounding, fluttering or beating irregularly, often for a few seconds or, in some cases, a few minutes.
Sometimes atrial fibrillation does not cause any symptoms and a person who has it is completely unaware that their heart rate is irregular.
When the heart beats normally, its muscular walls contract (tighten and squeeze) to force blood out and around the body.
They then relax so the heart can fill with blood again. This process is repeated every time the heart beats.
In atrial fibrillation, the heart's upper chambers (atria) contract randomly and sometimes so fast that the heart muscle cannot relax properly between contractions. This reduces the heart's efficiency and performance.
Atrial fibrillation occurs when abnormal electrical impulses suddenly start firing in the atria.
These impulses override the heart's natural pacemaker, which can no longer control the rhythm of the heart. This causes you to have a highly irregular pulse rate.
The cause is not fully understood, but it tends to affect certain groups of people, such as those over 65.
It may be triggered by certain situations, such as drinking too much alcohol or smoking.
Many people live for years with atrial fibrillation without problems. However, atrial fibrillation can lead to future problems as listed below:
- Because the atria are beating rapidly and irregularly, blood does not flow through them as quickly. This makes the blood more likely to clot. If a clot is pumped out of the heart, it can travel to the brain, resulting in a stroke. People with atrial fibrillation are 5 to 7 times more likely to have a stroke than the general population. Clots can also travel to other parts of the body (kidneys, heart, intestines), and cause other damage.
- Atrial fibrillation can decrease the heart’s pumping ability. The irregularity can make the heart work less efficiently. In addition, atrial fibrillation that occurs over a long period of time can significantly weaken the heart and lead to heart failure.
- Atrial fibrillation is associated with an increased risk of stroke, heart failure and even death.
Atrial flutter:
The electrical system of the heart is the power source that makes the heart beat. Electrical impulses travel along a pathway in the heart and make the upper and lower chambers of the heart (atria and the ventricles) work together to pump blood through the heart.
A normal heartbeat begins as a single electrical impulse that comes from the sinoatrial (SA) node, a small bundle of tissue located in the right atrium. The impulse sends out an electrical pulse that causes the atria to contract (squeeze) and move blood into the lower ventricles. The electrical current passes through the atrioventricular (AV) node (the electrical bridge between the upper and lower chambers of the heart), causing the ventricles to squeeze and release in a steady, rhythmic sequence. As the chambers squeeze and release, they draw blood into the heart and push it back out to the rest of the body and lungs. This is what causes the pulse we feel on our wrist or neck.
Atrial flutter is similar to atrial fibrillation, a common heart rhythm disorder. However, the rhythm in your atria is more organized and less chaotic in atrial flutter than are the abnormal patterns common with atrial fibrillation. Sometimes you may have periods of both atrial flutter and atrial fibrillation.
Although people with atrial flutter may not experience symptoms, the disorder can cause stroke, heart failure and other complications. There are effective treatments for atrial flutter, including scarring small areas of heart tissue (ablation) or medication.
Atrial Flutter itself is not life threatening. If left untreated, the side effects of Atrial Flutter can be potentially life threatening. Atrial flutter makes it harder for the heart to pump blood effectively. With the blood moving more slowly, it is more likely to form clots. If the clot is pumped out of the heart, it could travel to the brain and lead to a stroke or heart attack.
Without treatment, Atrial flutter can also cause a fast pulse rate for long periods of time. This means that the ventricles are beating too fast. When the ventricles beat too fast for long periods of time, the heart muscle can become weak and tired. This condition is called cardiomyopathy. This can lead to heart failure and long-term disability.
Without treatment,Atrial flutter can also cause another type of arrhythmia called atrial fibrillation. Atrial fibrillation is the most common type of abnormal heart rhythm.
Supraventricular tachycardia (SVT):
With this condition, the fast heartbeat starts in the top chambers of the heart, the atria. When electrical signals in the atria fire off early, the atria contract too soon. That interrupts the main electrical signal coming from the SA node. This results in the heart beating very quickly through an abnormal and separate pathway.
This condition is divided into three types:
Atrioventricular nodal reentrant tachycardia is the most common form. If you have it, there’s an extra pathway in your heart that causes an electrical signal to circle around and around instead of moving down to the ventricles. This can trigger the rapid heartbeat.
The AV node slows down the electrical signal before sending it to the ventricles. This slight delay allows the ventricles to fill with blood. When electrical impulses reach the muscles of the ventricles, they contract, causing them to pump blood either to the lungs or to the rest of the body.
In a healthy heart, this process usually goes smoothly, resulting in a normal resting heart rate of 60 to 100 beats a minute.
Supraventricular tachycardia occurs when faulty electrical connections in the heart or abnormal areas of electrical activity trigger and sustain an abnormal rhythm. When this happens, the heart rate accelerates too quickly and doesn't allow enough time for the heart to fill before it contracts again. These ineffective contractions of the heart may cause you to feel light-headed or dizzy because the brain isn't receiving enough blood and oxygen.
Short-term or urgent management of SVT can be separated into pharmacologic and nonpharmacologic strategies. Nonpharmacologic management typically uses maneuvers that increase vagal tone to decrease heart rate. Pharmacologic management typically includes intravenous adenosine (Adenocard) or verapamil, which are safe and effective treatment choices for terminating SVT, but verapamil is more effective for suppression of this rhythm over time. is an algorithm for the short-term management of SVT. Patients who are hemodynamically unstable need to be resuscitated with electrocardioversion to avoid further deterioration of cardiovascular status.
TYPES:
AVNRT(Atrioventricular nodal reentrant tachycardia)
The most common type of SVT is AVNRT. Most patients with AVNRT do not have structural heart disease; the group most often affected is young, healthy women. However, some patients do have underlying heart disease, such as pericarditis, previous myocardial infarction, or mitral valve prolapse. The coexistence of slow and fast pathways in atrioventricular nodal tissue is the basis of aberrant substrate for reentrant tachyarrhythmias.
AVRT(Atrioventricular reciprocating tachycardia)
The second most common type of SVT is AVRT. Patients with this arrhythmia typically present at a younger age than those with AVNRT. This SVT is caused by accessory pathways (or bypass tracts) that serve as aberrant conduits for impulses that pass from the sinoatrial node and travel in an antegrade or retrograde fashion through such tracts, establishing a reentry circuit. AVRT, occasionally comorbid with Wolff-Parkinson-White syndrome, is a diagnosis not to be missed because this rhythm may spontaneously develop into atrial fibrillation. Key electrocardiography (ECG) findings, such as a delta wave, are not always apparent because of the accessory pathway being concealed; therefore, special diagnostic testing may be needed
Ventricular tachycardia:
Your heart rate is controlled by electrical impulses that trigger each contraction and determine the rhythm of the heart. When this process is disrupted and the electrical signals are sent too quickly, ventricular tachycardia can occur. The rapid heartbeat doesn’t give the ventricles enough to time to fill with blood before the heart contracts. As a result, the heart may not be able to pump enough blood to the rest of the body.
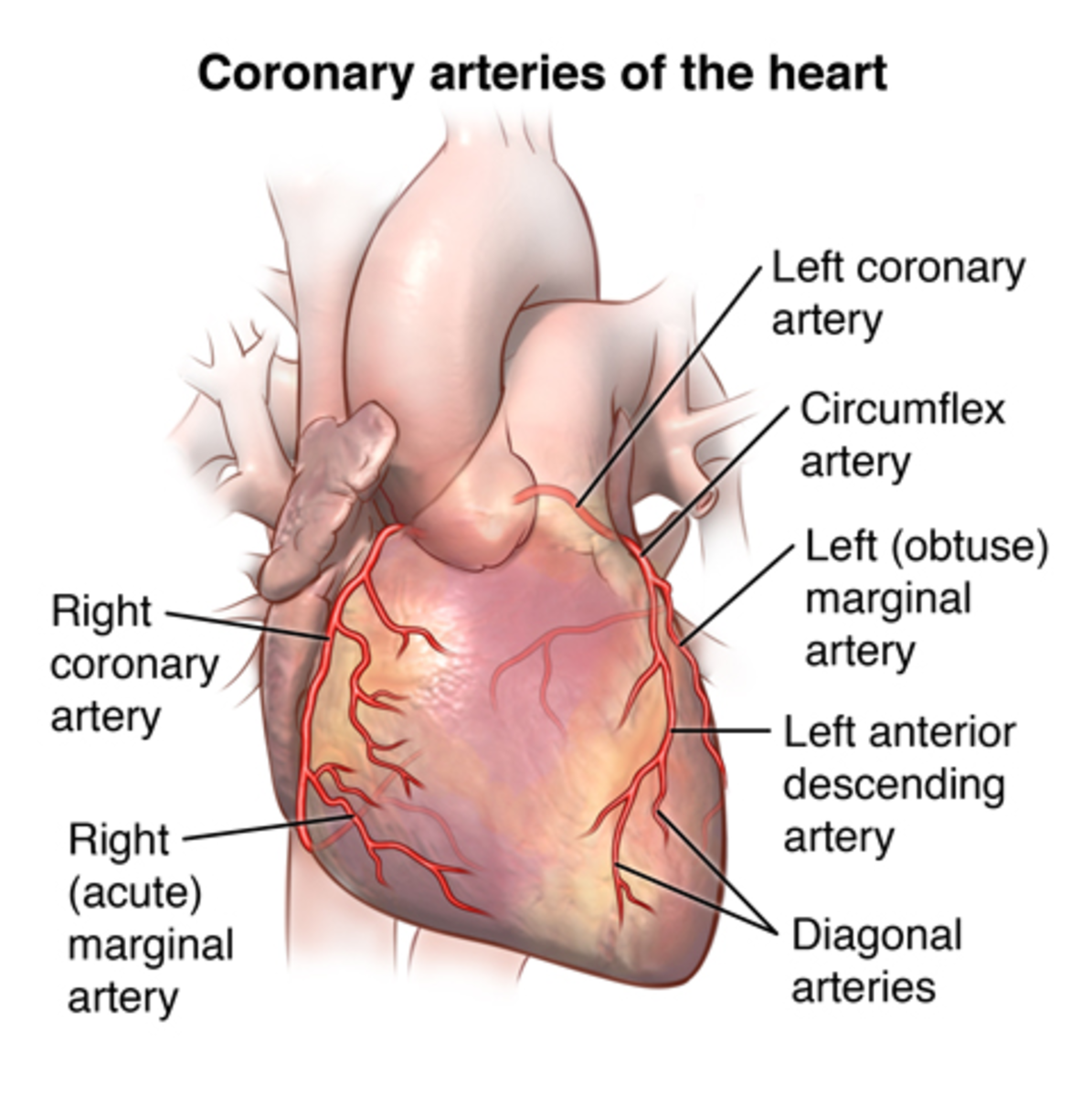
Ventricular tachycardia may only last for a few seconds or for much longer. It doesn’t always cause symptoms, but when symptoms do occur, they may include lightheadedness, dizziness, and fainting. The condition most commonly affects people who have heart disorders, such as coronary artery disease and cardiomyopathy.
Ventricular tachycardia may eventually lead to ventricular fibrillation, which is characterized by a rapid, inadequate heart rhythm. In this condition, the heartbeat is so fast and irregular that it causes the heart to stop working. To prevent this complication from occurring, it’s important to get immediate treatment for ventricular tachycardia.
Sustained ventricular tachycardia (VT) is a ventricular rhythm faster than 100 bpm lasting at least 30 seconds or requiring termination earlier due to hemodynamic instability. VT is defined as a wide complex tachycardia 120 milliseconds or greater) that originates from one of the ventricles, and is not due to aberrant conduction e.g., from bundle branch block), at a rate of 100 bpm or greater. "Idiopathic" occurs in the absence of apparent structural heart disease (e.g., prior MI, active ischemia, cardiomyopathy, valvular disease, arrhythmogenic right ventricular cardiomyopathy, left ventricular noncompaction, or other disorders of the myocardium), known channelopathy , Brugada syndrome, catecholaminergic polymorphic VT, , drug toxicity, or electrolyte imbalance. VT can be described as monomorphic or polymorphic.is a polymorphic VT with a characteristic twisting morphology occurring in the setting of interval prolongation. Sustained VT usually results in hypotension and symptoms of weakness, syncope, or palpitations; however, the arrhythmia may be present in patients who are asymptomatic and normotensive.
If an electrocardiogram (EKG, ECG) can be done while ventricular tachycardia is occurring, it often provides the most useful information. An electrocardiogram is a tracing of the electrical activity of your heart. It is usually done along with a history and physical examination, lab tests, and a chest X-ray.
Because ventricular tachycardia can occur intermittently and may not always be captured by an EKG at the doctor's office, you may be asked to use a portable EKG to record your heart rhythm on a continuous basis, usually over a 24-hour period. This is referred to by several names, including ambulatory electrocardiography, ambulatory EKG, Holter monitoring, 24-hour EKG, or cardiac event monitoring.
Your doctor may recommend further tests, including an echocardiogram, to evaluate your heart's function, a stress test or coronary angiogram to determine whether a part of the heart is not getting enough blood, and/or an electrophysiology. An EP study can locate specific areas of heart tissue that give rise to abnormal electrical impulses, which may be causing the ventricular tachycardia. This information is used to determine the best treatment.
Ventricular fibrillation:
When VF occurs, the two chambers in the lower portion of your heart aren’t able to pump hard enough to move blood through your body. These lower chambers are called ventricles. This makes your blood pressure drop quickly and keeps blood from traveling through your body. As a result, blood can’t get to your vital organs.
Fainting or losing consciousness are the most common symptoms of VF, earlier symptoms include:
- chest pain
- dizziness
- nausea
- rapid, fluttering heartbeat
- shortness of breath
These early symptoms can occur one hour or less before fainting or loss of consciousness occurs.
Ventricular fibrillation is a life-threatening cardiac arrhythmia in which the coordinated contraction of the ventricular myocardium is replaced by high-frequency, disorganized excitation, resulting in [the effective] failure of the heart to pump blood. Ventricular fibrillation is the most commonly identified arrhythmia in cardiac arrest patients. In the prehospital setting, 65%-85% of patients in cardiac arrest have Ventricular fibrillation identified as the initial rhythm by emergency services personnel.
Symptoms:
No matter which type of tachycardia you have, you may feel:
- Dizziness is the feeling of being lightheaded, woozy, or unbalanced. It affects the sensory organs, specifically the eyes and ears,
- Lightheadedness The sensation of lightheadedness can be short-lived, prolonged, or, rarely, recurring.
- Shortness of breath Your heart and lungs are involved in transporting oxygen to your tissues and removing carbon dioxide, and problems with either of these processes affect your breathing.
- Chest pain appears in many forms, ranging from a sharp stab to a dull ache. Sometimes chest pain feels crushing or burning
- Heart palpitations make you feel like your heart is beating too hard or too fast, skipping a beat, or fluttering. You may notice heart palpitations in your chest, throat, or neck.
In extreme cases, you could become unconscious or go into cardiac arrest.
But sometimes, a super-fast heart rate causes no symptoms at all.
TESTS:
Electrocardiogram (ECG):
(ECG or EKG) is a diagnostic tool that is routinely used to assess the electrical and muscular functions of the heart. While it is a relatively simple test to perform, the interpretation of the ECG tracing requires significant amounts of training. Numerous textbooks are devoted to the subject.
The heart is a two stage electrical pump and the heart's electrical activity can be measured by electrodes placed on the skin. The electrocardiogram can measure the rate and rhythm of the heartbeat, as well as provide indirect evidence of blood flow to the heart muscle.
Your doctor may also ask you to use portable ECG devices at home to provide more information about your heart rate. These devices include:
-
Holter monitor. This portable ECG device is carried in your pocket or worn on a belt or shoulder strap. It records your heart's activity for an entire 24-hour period, which provides your doctor with a prolonged look at your heart rhythms.
Your doctor will likely ask you to keep a diary during the same 24 hours. You'll describe any symptoms you experience and record the time they occur.
- Event monitor. This portable ECG device is intended to monitor your heart activity over a few weeks to a few months. You wear it all day, but it records only at certain times for a few minutes at a time.
Cardiac imaging:
Cardiac imaging is a subspecialty of diagnostic radiology. A cardiac radiologist supervises or performs and then interprets medical images to diagnose diseases of the heart such as heart disease, leaky heart valves and defects in the size and shape of the heart.
A cardiac radiologist uses imaging techniques such as X-rays, ultrasound (echocardiograms), CT (computed tomography) scans and MRI (magnetic resonance imaging) scans.
These tests are used to screen for heart disease, determine what is causing your symptoms and monitor your heart and find out if your treatment is working.
All imaging technologies have undergone continual improvements since their inception to a point that imaging has become essential in both clinical practice and research. This article provides a glimpse into the future of cardiovascular imaging and highlights areas of imaging that still need improvement, with a view towards improving the practice of health care, where efficiency and value are becoming ever more dominant criteria throughout the continuum of care
Stress Test:
A stress test, also called an exercise stress test, shows how your heart works during physical activity. Because exercise makes your heart pump harder and faster, an exercise stress test can reveal problems with blood flow within your heart.
A stress test usually involves walking on a treadmill or riding a stationary bike your heart rhythm, blood pressure and breathing are monitored. Or you'll receive a drug that mimics the effects of exercise.
Your doctor may recommend a stress test if you have signs or symptoms of coronary artery disease or an irregular heart rhythm (arrhythmia). The test may also guide treatment decisions, measure the effectiveness of treatment or determine the severity if you've already been diagnosed with a heart condition
During stress testing, you exercise (walk or run on a treadmill or pedal a stationary bike) to make your heart work hard and beat fast. Tests are done on your heart while you exercise
Causes
Causes of sinus tachycardia - A rapid heartbeat may be your body's response to common conditions such as: Fever Anxiety Some medicinal and street drugs Severe emotional distress Fright Strenuous exercise Other causes but less commonly, it may indicate: Anemia (low blood count) Increased thyroid activity Heart muscle damage from heart attack or heart failure Hemorrhage (severe bleeding) You may be having Palpitations, which are feelings or sensations that your heart is pounding or racing. They can be felt in your chest, throat, or neck. You may Have an unpleasant awareness of your own heartbeat or may Feel like your heart skipped or stopped beats The heart's rhythm may be normal or abnormal when you have palpitations. Palpitations are not serious most of the time. Sensations representing an abnormal heart rhythm (arrhythmia) may be more serious. Your doctor should consider and treat the cause of sinus tachycardia rather than the condition itself. If your rapid heartbeat is a symptom of a more serious or longer term problem, simply slowing the heart rate without checking for underlying reasons could cause more harm because you are leave the underlying condition untreated.
Your doctor will ask you to describe your symptoms. He or she will review your personal medical history and potential causes of tachycardia, including lung disease, thyroid disorders, and medications. Your doctor will want to know if you have a family history of heart disease and cardiac arrhythmias.
During the physical examination, your doctor will check your heart rate and rhythm. Your doctor also will check for an enlarged heart, for heart murmurs (one sign of a heart valve problem), for abnormal lung sounds and for physical signs of thyroid abnormalities (enlarged thyroid gland, hand tremor and an abnormal protrusion of the eyes).
To further evaluate your tachycardia, your doctor will order an electrocardiogram (EKG). However, because some forms of tachycardia come and go, a one-time office EKG may be normal. If this is the case, you may need a test called ambulatory electrocardiography. For this test, you will wear a portable EKG machine called a Holter monitor for a period, usually for 24 hours. If symptoms occur infrequently, you may have to wear a monitor for much longer. You will be taught to press a button to record EKG readings when symptoms occur.
Rhythm
| Regular
| |
|---|---|---|
Rate
| Fast (> 100 bpm
| |
P Wave
| Normal, may merge with T wave at very fast rates
| |
Notes
| QT interval shortens with increasing heart rate
|
Dear Heart stop going for everything.Your Job is to pump Blood thats it