Spinal And Bulbar Forms Of Poliomyelitis And The Clinical Presentations In Polioencephalitis
Spinal And Bulbar Forms Of Poliomyelitis

Forms Of Poliomyelitis
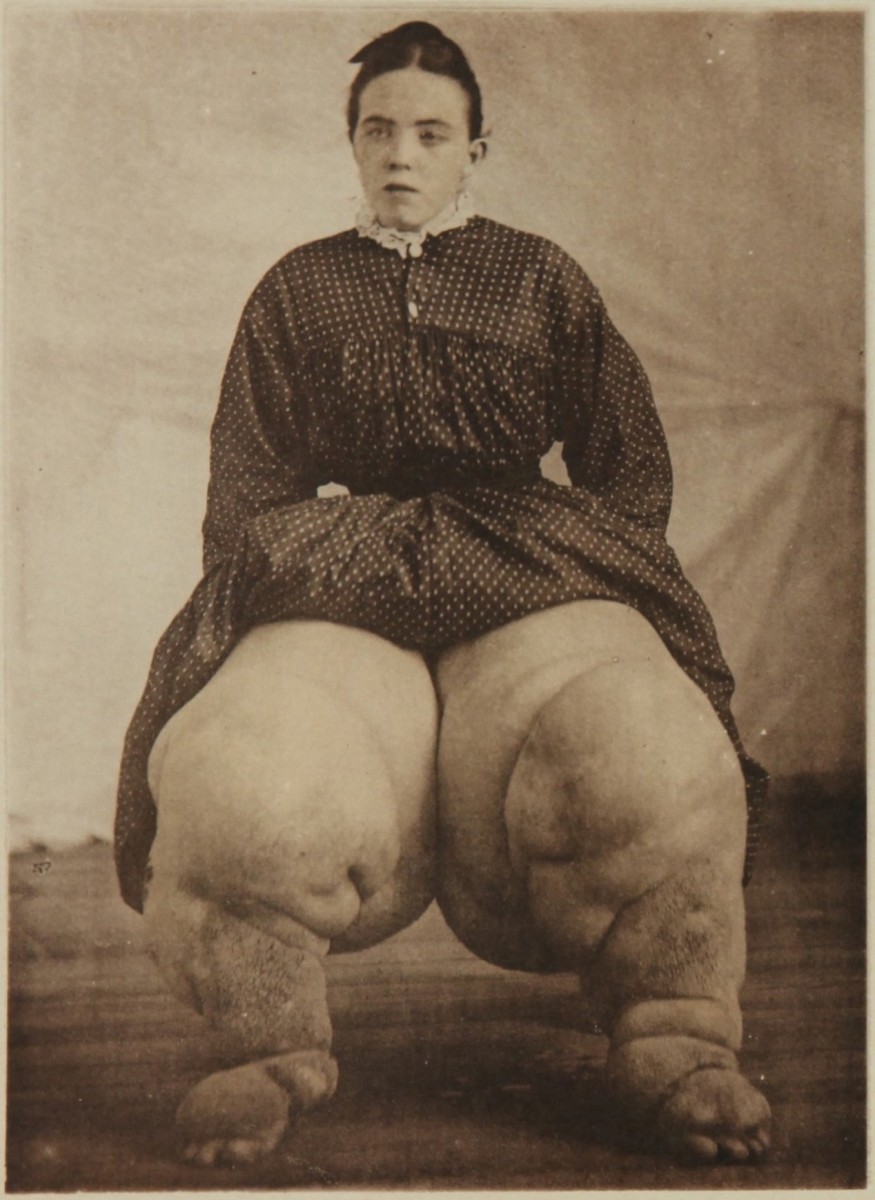
Spinal Form: The initial manifestations in this form are followed by diffuse muscle twitching and cramps. The muscles may be tender. Transient fasciculations may be noted. Paralysis of muscles sets in rapidly by the third or fourth day of illness. The spectrum ranges from mild weakness of a limb or a part there of, to extensive flaccid quadriplegia. Paralysis usually takes place within hours in the majority of cases, rarely it may take four to five days or more. There seems to be a predilection for the cervical and lumbar segments of the spinal cord. The tendon jerks are abolished. Objective sensory changes do not occur. The paralysis is asymmetrical, maximal in the beginning and tends to recover with time. Total destruction of neurons leaves behind complete paralysis, partially affected groups recover to varying combinations of muscle paralysis. Often, part of a muscle is affected, leaving the remaining part unaffected. Ventilatory insufficiency may develop, if the diaphragm and intercostals are paralyzed. Respiratory failure manifests as restlessness and tachypnea, with shallow irregular respiration.
Bulbar form: Affection of the lower cranial nerves occurs early in this form. It may precede or follow the spinal involvement. Dysphagia, dysarthria and dysphonia occur commonly, facial palsy may develop less commonly.
Involvement of the nuclei of the medullar reticular formation results in dysfunction of the vital areas such as the respiratory and vasomotor centers. These manifest as irregularity of respiration with apnoeic spells, vasomotor collapse, transient hypertension and cute pulmonary edema.
Convulsions In Polioencephalitis

Polioencephalitis
This form is unusual and is characterized by alteration in the level of consciousness, convulsions, signs of brainstem involvement and varying combinations of spastic or flaccid paralysis. This condition may mimic other forms of encephalitis.
Diagnosis: Poliomyelitis should be diagnosed clinically in any unimmunized child who develops an initial febrile illness and proceeds to acute paralysis within a few days. Rarely, Coxsackie and ECHO viruses are also capable of producing paralytic diseases.
Non-paralytic poliomyelitis has to be differentiated from other conditions causing aseptic meningitis. Acute motor polyneuropathy occurring in nutritional and toxic neuropathies, viral encephalitis and Guillain-Barrer syndrome may cause difficulty in diagnosis. In Guillain-Barre syndrome, there is considerable rise in CSF proteins without rise in cells (albuminocytological dissociation), whereas in polio, the cellular response occurring before the rise in proteins is characteristic. Nerve conduction studies also help in diagnosis. Slowing of the velocity of nerve condution in the peripheral nerves and nerve roots is suggestive of Guillian-Barre syndrome. Acute intermittent porphyria may present rarely with motor paralysis. Other features of the disease such as psychiatric disturbances, abdominal pain and hypertension may be evident. Demonstration of excess of porphobilinogen in the urine supports the diagnosis. Sometimes, painful conditions near the joints result in restriction of movement of the part. Such pseudo-paralysis may occur in osteomyelitis, periosteitis, arthritis, hemophilia, scurvy with subperiosteal bleeding, syphilitic epiphysitis, etc. These have to be carefully looked for and excluded by local examination. Rarely, hysterical paralysis may be mistaken for poliomyelitis. This has to be bourne in mind when other features and the CSF findings help to make a bedside diagnosis in almost all cases. The virus can be isolated from the CSF in some cases. Serological diagnosis is established by demonstrating rising titers of neutralizing and complement fixing antibodies in the serum.
© 2014 Funom Theophilus Makama