Staphylococcal Infections: Epidemiology, Pathogenesis, Treatment, Prevention And The Toxic Shock Syndrome
Physical Presentations Of Staphylococcal Infections

Epidemiology And Pathogenesis
Staphylococci are the most ubiquitous organisms affecting man. Staphylococcus aureus is the most common pathogen.
Epidemiology: Healthy people carry staphylococci in the nose and to a lesser extent in the perineum. The organism is spread by direct contact, through formites, dusts or by airborne droplets. Large number of organisms are shed from superficial lesions and from the respiratory tract. Though initially, staphylococci were sensitive to sulphonamides and penicillins, many strains have developed resistance to several antibiotics in common use. Penicillin is inactivated by penicillinase (betalactamase) and this is the basis of penicillin resistance. Resistance can be transferred from one strain to another by transduction through the mechanism of plasmids. At present, most hospital strains of staphylococci are resistant.
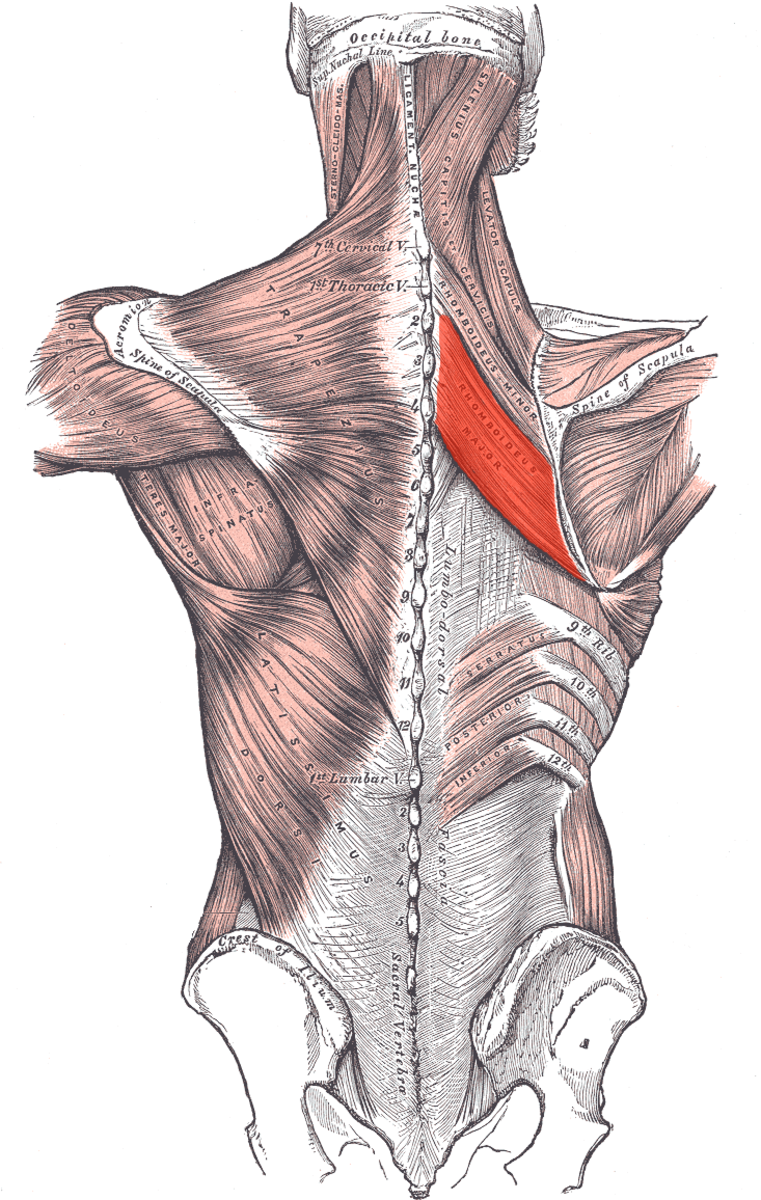
Pathogenesis: Staphylococci invade hair follicles and sebaceous glands. Incidence of infection is higher in diabetics and obese subjects. Subjects recovering from influenza and measles are more susceptible to staphylococcal infection. The organism multiples in the lesions and leads to suppurative inflammation.
Toxins of staphylococci: Staphylococcus aureus elaborates toxins like hemolysis, leucocidins enterotoxin, hyaluronidase, fibrinolysin, nuclease, lipase and protease. In addition, nontoxic substances like coagulase which facilitate invasion are also produced.
Toxic Shock Syndrome

Treatment And Prevention
Treatment
Superficial skin infections respond to proper cleaning and application of topical ointments containing chlorhexidine or cetrimide. In systemic infections or when the lesions are deep, systemic antibiotics are required. Benzyl penicillin is the most effective antibiotic if the organisms are sensitive, Methicillin and cloxacillin are effective against penicillinase- producing strains.
For staphylococcal pneumonia caused by penicillin- resistant organisms, methicillin, oxacillin, nafcillin, cephalothin and cephalozolin in doses of 1g every 4 to 6 hours is preferred. Subjects allergic to penicillin may be treated with vancomycin 0.5g intravenously every 6 to 8 hours or clindamycin 600 mg four times a day. A full course of treatment extends for 10 to 14 days. If empyema develops, antimicrobial drugs are introduced directly into pleural cavity along with proteolytic enzymes. If needed, surgical drainage may be under-taken. Oxygen inhalation, intravenous fluids, bronchodilators and supportive therapy should be instituted.
Prevention
Patients with open staphylococcal lesions should be isolated. Surgeons and hospital staff should be periodically checked by local application of neomycin and chlorhexidine. Topical application of antiseptics such as hexachlorophene are found useful in preventing staphylococcal infection in selected cases.
Toxic Shock syndrome
This syndrome described first in 1978 consists of sudden development of shock associated with high fever, headache, sore throat, diarrhea and erythroderma. It was noted in young girls using certain brands of vaginal tampons during menstruation. This syndrome is caused by a diffusible toxin produced by staphylococci (phage type I) which grows in such tampons. Blood cultures are negative. Mortality is high in untreated cases.
Treatment: Emergency measures to combat septic shock should be instituted. Betalactamase- resistant antibiotics should be used in full dosage from the onset. Corticosteroids have helped to reduce toxemia in some cases. Further use of such tampons should be avoided.
© 2014 Funom Theophilus Makama