What is a Subarachnoid Haemorrhage and how does it affect the brain?

Coiling
What Causes a Subarachnoid Haemorrhage?
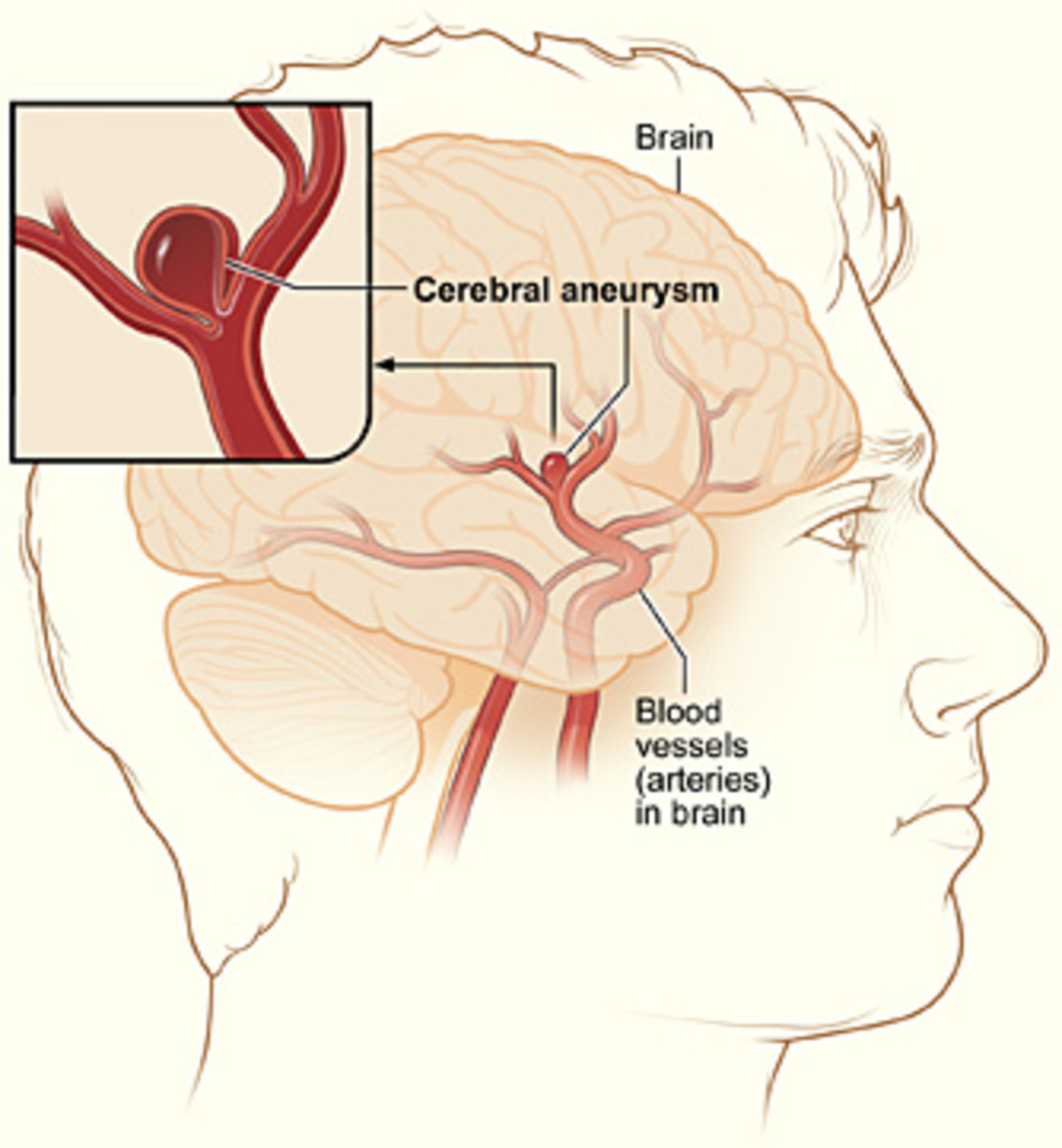
A subarachnoid haemorrhage (or SAH) is quite an uncommon condition of the brain which can lead to stroke. It is where blood vessels leak onto the brain, usually due to a burst aneurysm (known as berry aneurysms). These burst when there is a weakness in the blood vessel wall or from a head injury. Smokers or those with high blood pressure or hypertension are also at risk of SAH.
Signs and Symptoms of a Haemorrhage
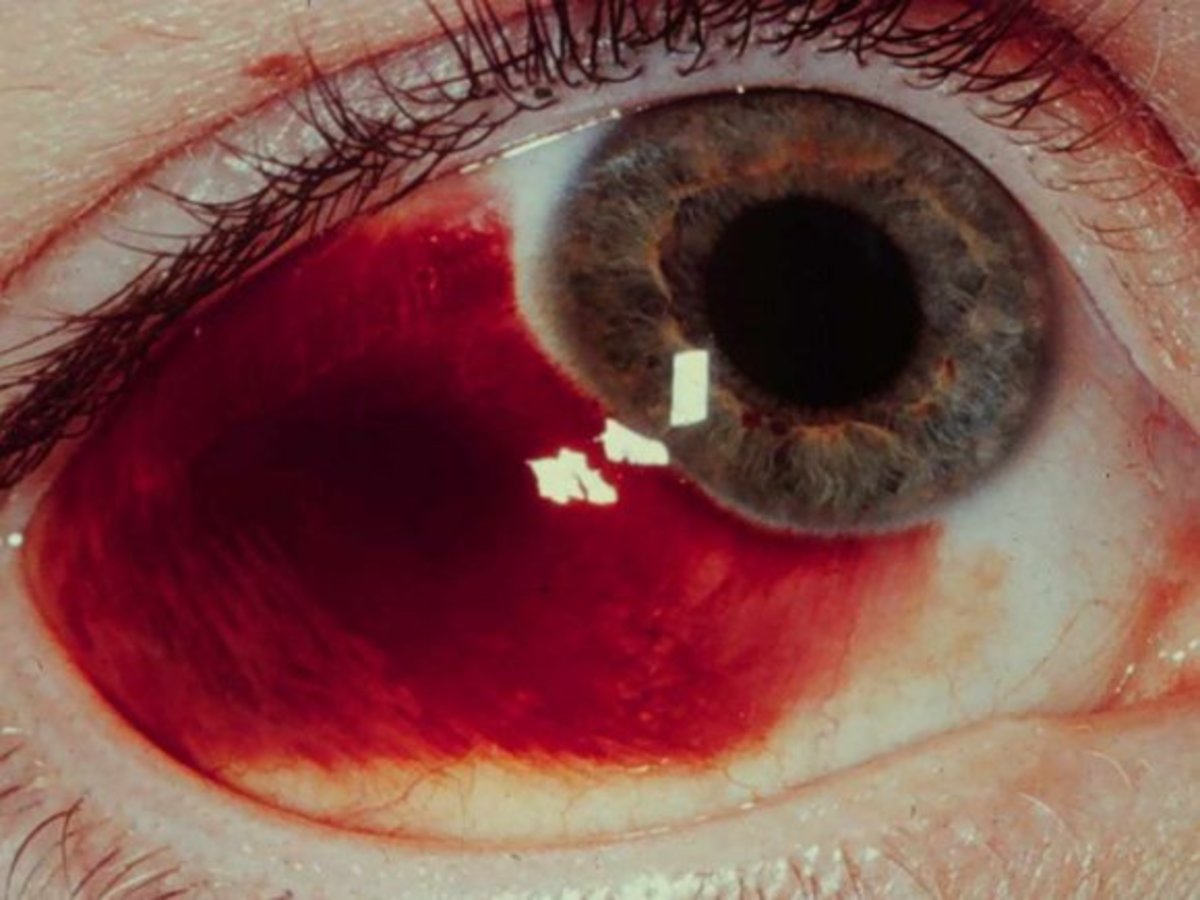
Symptoms tend to be a sudden headache which is severe and could cause collapse. Photo phobia (sensitivity to light) and symptoms similar to meningitis are also a sign that the patient has a haemorrhage in the subarachnoid space in the brain. The earlier the patient reaches hospital and is treated in a neuro-surgical unit, the better chance of recovery.
It is possible that a SAH could be fatal. This could be within hours or weeks of development, but the chances of survival are also good if the patient survives the bleeding and is admitted to hospital. Women are generally more likely to suffer from a SAH than men, with a ratio of 3:2. Women have a greater risk over the age of 40, but men are more likely to have a SAH before the age of 40.
Other signs and symptoms to watch out for include: Mild sudden headache, severe sudden headache, loss of consciousness, seizures, nausea and vomiting and focal damage.
A CT head scan will be carried out to detect the haemorrhage before going to theatre for surgery. However, a lumber puncture may be performed if the bleed was more than six hours previous, the CT scan is negative or a patient is confused or less responsive. If the spinal fluid is bloodstained it is cerebal, and the patient is referred to a neurosurgical team.
The surgeon will treat the aneurysm either by using 'coiling' or 'clipping' procedures when the patient has been assessed. The clinical assessment will be carried out to obtain the severity of the SAH. Neurological observations are done on the patient to indicate their GCS (Glasgow Coma Scale). If the GCS is 15/15, the patient has no confusion, is fully aware, and has good power in all limbs.
If the patient goes for clipping, it is usually because the aneurysm is very large or cannot be coiled due to the location of the site. Part of the skull is removed (craniotomy) and a small metal clip is fixed at the neck to stop blood flow to the aneurysm. Although it is effective, it is a complicated procedure.
Coiling however is a less invasive method, as it does not require open surgery. It was introduced in the early 1990s without the need of craniotomy. Small metal coils are inserted into the aneurysm through the vascular system to block blood flow to minimise risk of further bleeding. Blood then clots around the coils to seal the area.
After treatment, the patient stays on the ward for flat bed rest and observations before rehabilitation for full recovery. 50% of patients who survive SAH can continue with their former life and employment. A significant number however will suffer from a minor personality change or intellectual deficit and epilepsy.