Surviving With Bladder Cancer
Surviving With Bladder Cancer
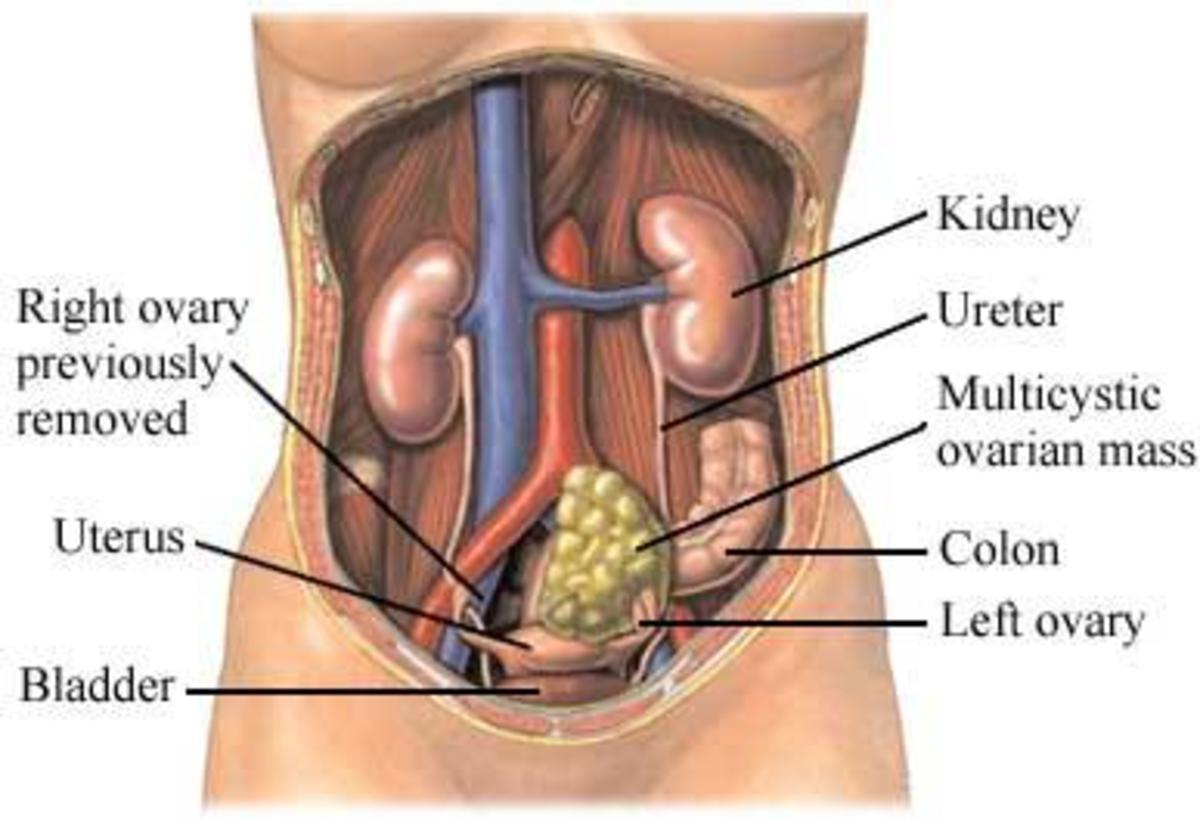
The urinary system is composed of the kidneys, one on the right, and one on the left. The kidney drains the urine through the ureter, which is a long tube that drains down into the bladder. The kidney is composed of two main parts. We have got meat of the kidney, which we call the parenchyma and the types of cancer that occur in the meat of the kidney are called renal cell carcinoma and then we have got the sink where the urine actually gets excreted into, which is called the collecting system of the kidney. Each ureter then drains down into the bladder. The bladder has various layers, there is an internal layer of the bladder and then there is the lamina propria of the bladder, the muscular layer of the bladder and then the fatty layer of the bladder. The main subject we are talking here is about the types of kidney cancer, and the type of urothelial carcinoma. So, the meat of the kidney would be called renal cell carcinoma, the collecting system of the kidney, the ureter, and the bladder would be urothelial carcinoma. This is just the basic nomenclature.
The bladder cancer is the fourth most common malignancy in the United States. There are nearly 75,000 patients, individuals, Americans who are diagnosed with bladder cancer every year, and over 15,000 of those patients die from bladder cancer on a yearly basis. The incidence of bladder cancer is steadily climbing and by 2027 that bladder cancer would be the third most common cancer in men.
Individuals who have a family member with bladder cancer are two times as likely to develop bladder cancer. Race, white Americans are more likely to get bladder cancer than African Americans. Men are three times more likely to develop bladder cancer than compared to women. In age bladder cancer is the diagnosis of the elderly, not that of the young. There are also some infections that can actually promote bladder cancer growth. Some of these infections can be a worm, which is found in Africa, and Middle East, and some of them can be just chronic urinary tract infections. People have suggested that low fluid consumption may also increase the risk of getting bladder cancer.
There are certain types of chemo-therapies, and any radiation therapy to the area where the bladder is located would also increase your chance of getting bladder cancer. Tobacco is the leading cause of bladder cancer incidence in the United States. There are other agents that can also cause bladder cancer, such as dyes, and solvents, so people who work with rubber, and leather and textile and printing products, painters, machinists, mechanics, printers, hairdressers, and truck drivers are all more likely to get it because of the solvents that are being evaporated and fumes are inhaled.
Patients in their 20 are much less likely to get bladder cancer, but as individuals get older and older they are more likely to get bladder cancer. Half of the people who get diagnosed with bladder cancer are 73 years of age. So, it is more of a diagnosis of elderly Americans. Additionally, bladder cancer seems to be harshest on those that are in the elderly, in other words it is disproportionately more aggressive in those that are elderly. Part of it may be due to the immune system; part of it may be just due to the face that the bladder has been exposed to toxins for that much longer.
Whenever we see small, little tiny tumors in the bladder we call those Ta bladder tumors. Sometimes there are flat lesions, those are called Tis, or CIS, or carcinoma in situ. Sometimes the cancer can invade this lamina propria layer, it would be a T1, if it invades the muscle, it would be a T2, if it invades the surrounding fat, it is T3, and if it invades surrounding organs it is T4. Bladder cancer or urothelial carcinoma is not just in the bladder, it could actually be in the ureter, or actually up in the collecting system of the kidney.
As far as the stage of the bladder cancer now we have got varying stages and people may be diagnosed with one stage and they cannot really compare their outcomes unless you really have to compare them with someone with the similar stage. Most bladder cancers are actually localized to that inner layer in 51% of those patients, 35% of the patients are actually diagnosed with cancer that is still localized to the bladder. In people whereby the cancer is still on that inner layer of the bladder, their 5-year survival rate is 96%, so when one gets diagnosed with this type of bladder cancer there is a very good chance that we can beat it. If the cancer is localized to the bladder, there is about 70% change of that the patient will live 5 years from this. So, there is a 30% of dying of bladder cancer. Once that cancer spreads to the lymph nodes; however, is where the mortality rates significantly increases. So about one-third of the patients are alive after 5 years of the cancer has spread to the lymph nodes, meaning two-thirds of the patients have died, and if it spread to distant organs a chance of them surviving 5 years is 5%. So to summarize this briefly, 75% of patients who are diagnosed with cancer that is still localized to the inner linings of the bladder, or the lamina propria layer, their chance of dying of bladder cancer are only 15%. Majority of the deaths of bladder cancer are attributed to those that have invaded the muscle or have invaded to the lymph nodes.
Progression
About 15 to 25% of the patients who have this non-invasive cancer can actually invade into the bladder muscle wall and start spreading to the lymph nodes and about 20 to 45% of the patients who are diagnosed with an invasive cancer will actually have metastatic cancer when the doctors remove the bladder at a later time point.
The standard of care for treating this low-grade bladder cancer is cutting out the tumor in its entirety and injecting a little bit of chemotherapy in the bladder to prevent the free-floating cancer cells from re-implanting anywhere else. These patients do not need too frequent cystoscopy. A cystoscopy is where we place a small little scope into the urethra and into the bladder and look around to see if there are any recurrences. These low-grade Ta tumors tend to be less aggressive and can be surveyed less frequently.
As coming to high-grade tumor, it has a velvety pattern. It is sessile, meaning it is flat; it does not have that cauliflower appearance. The standard of care for this is removing the tumor and if you find out that it is high-grade, or if it is T1 you make sure that the doctor takes you back to the operating room to cut out some more tissue to make sure there is no residual disease. After all that was done after four weeks after that we advise that the doctor put BCG into the bladder. A doctor slips a small little catheter into the bladder and they squirt a small amount of BCG and what it does is it ramps up the immune system in the bladder to kill all the cancer cells. Most people gets six weeks of BCG, so they come in once a week for six weeks and they get this treatment, but what is important is you do not stop there. Patients should get three installations once a week for three weeks every six months for up to three years. So, in total it adds up to about 27 installations in a three-year period of time. These patients since they have an aggressive tumor even though it has not invaded yet, we advise that they undergo frequent cystoscopy in cytology. Cytology means just sending the urine off for urine test, and there are specialists in pathology who look under the microscope to see if there are any cancer cells there. It is also recommended that they get a CT scan every one to two years. For patients who may have invasive disease it is recommended to get it every year.
The thing with high-grade non-muscle invasive bladder cancer is that they have a high propensity of recurring. If they do recur the doctor may try to put another round of BCG in the bladder, another six installations, or they may want to put in interferon, which also ramps up the immune system. They might want to try these other chemo-therapeutics, which is gemcitabine or valrubicin. Most doctors should advise their patients that radical cystectomy is still something they should strongly consider if their cancer keeps coming back despite BCG therapy.
However, the treatment type depends on the grade, is it recurrent high-grade Ta, or is it recurrent high-grade T1. T1 would be more aggressive than Ta. If the cancer tends to come back much sooner, it tends to pretend a worse prognosis whereas one that goes cancer-free for a year, or two years and if it comes back those patients tend to do well. How about if the cancer is invasive what is being done for that? Currently, the doctors recommend the patients have their bladder excised, so the entire bladder and surroundings organs are removed. Sometimes it is recommended that they get chemotherapy before or after surgery and once the bladder is taken out the patient loses the storage capacity, so another way should be made to divert the urine and this can be done either by building a new bladder made out of intestines, or building a new bladder that patient can catheterize off to the side, or an ileal conduit where urine just drains into a bag constantly.
It is also recommended that patients may benefit from radiation therapy along with chemotherapy. They get radiation to the bladder five days a week for about six to eight weeks and they also get some chemotherapy associated with it. Chemotherapy in combination with either surgery, radiation can be before, or after and it can last anywhere from six weeks to eight months, it depends on the type of protocol that the patient is on.
If the cancer has also already spread to other places there really is no benefit in surgery or radiation unless it is reserved for those where we are trying to treat pain or local symptoms from a tumor that is invading into surrounding structures. For those patients where the cancer has spread to the liver or to the lungs or to the bone, systemic chemotherapy is the primary treatment, and the types of chemotherapy one may get is MVAC, or one of these other agents, sometimes they are in combination, sometimes they are single agents.
The upper tract cancers are the ones where we actually find tumors in the collecting system of either the kidney, or in the ureter. The treatment for those non-invasive upper tract tumors is, the doctor slips a small scope and using a laser fiber that has the width of a hair follicle we can actually oblate these small tumors, or we can grasp these small tumors with a small basket that is a little bit larger than the size of a hair follicle. We can grab these tumors and pluck them out and we can prevent the kidney from being removed. The doctor also recommends that chemotherapy be instilled up here to prevent these free-floating cancer cells from re-implanting, or from recurring. The way we follow these patients is we recommend that we look up the kidneys frequently and actually get CT scans more frequently.
What if the upper tract cancer is invasive? For that it is recommended that the patient have the entire kidney and the ureter down to the level of the bladder be entirely removed. Chemotherapy should be considered in treating patients with an invasive upper tract cancer. It is usually recommended to give it before the kidney is removed because they have two kidneys and chemotherapy is better tolerated when it is given to patients with two kidneys than with one kidney.
Compliance with some of these measures have not been up to the par. When patients have low-grade bladder cancer the doctor instills a little bit of chemotherapy at the time of resecting the tumor to prevent those cancer cells from implanting. We know that it can cut down the risk of recurrence by about 35%; however, only 5% of patients ever get it.
What are some of the common risk factors for bladder cancer? Risk factors for bladder cancer include tobacco use, exposure to dyes, or solvents. It can also be the type of workplace the patient is in, so being exposed to some of the organic solvents, hairdressers, mechanics, machinists, truck drivers; those also increase the risk of getting bladder cancer. Three or four percent of men will develop bladder cancer sometime in their lifetime and about one percent of women will develop bladder cancer sometime in their lifetime, men more likely, women less likely, the older you are the more likely. In genetics, if you have a father, mother, brother, sister, with bladder cancer you are more likely to get bladder cancer.
This content is accurate and true to the best of the author’s knowledge and is not meant to substitute for formal and individualized advice from a qualified professional.
© 2020 Putcha Venu Madhav