The Effect of Opioids on Managing Dyspnea in Patients with Cystic Fibrosis

Cystic Fibrosis and Palliative Care
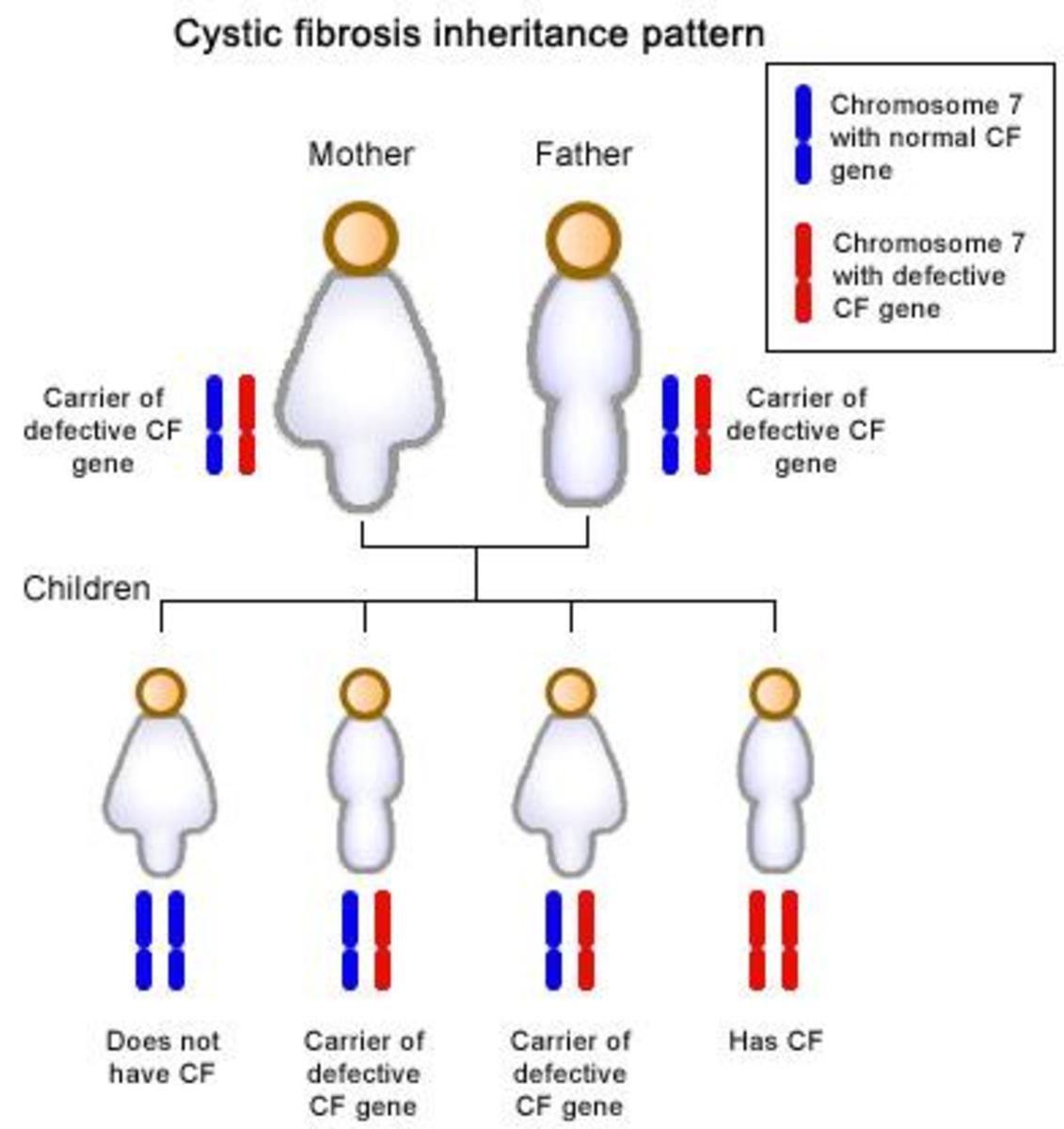
Cystic fibrosis is an incurable life threatening genetic disease that causes damage to the lungs due to persistent lung infections. It is the most common lethal genetic illness in the caucasian population of North America and is diagnosed in one out of every 3,000 live births. Cystic fibrosis remains universally fatal, with advanced lung disease as the primary cause of death (Robinson, 2000). A common symptom in the end stages is refractory dyspnea, in which the patients feel breathless and distressed that they are not receiving enough oxygen. Due to the fact that there is no cure for the disease and the dyspnea can be very upsetting to the patient, palliative measures are often taken which include opioid medications (Mahler, 2013).
End of life care has received little attention in the literature, despite the large cystic fibrosis patient population in North America and Europe (Robinson, 2000). Therefore, it is important and necessary as healthcare providers in palliative care to conduct studies and publish work in order to be able to carry out more evidence based practice in the care of individuals with cystic fibrosis. The pharmacological treatment choice used by physicians to address refractory dyspnea in patients with cystic fibrosis is opioids. Opioids are effective in relieving dyspnea by one or more different mechanisms: decreasing respiratory drive (associated corollary discharge), altering central perception, altering activity of peripheral opioid receptors located in the lung, and decreasing anxiety (Mahler, 2013).
PICO Question
In patients with cystic fibrosis receiving palliative care, what is the effect of oral opioids in comparison to nebulized opioids in managing refractory dyspnea?
Research Evidence
The five articles used for this paper were selected from peer reviewed journals accessed through the online databases, CINAHL and PubMed. The articles focus on either the use of opioids in treating dyspnea in terminal cystic fibrosis patients or specifically the use of nebulized opioids.
Evidence for Oral Opioids
1. (Mahler, 2013). This article addresses the uncertainties in figuring out the lowest effective dose of opioids necessary to help a given patient with refractory dyspnea. The article expresses in detail the mechanism of action that causes dyspnea on a neurological and psychological level and offers reasons for why opioids are effective at treating the condition as well as other methods used in treatment. The article is very indepth and provides a large body of factual information for anyone attempting to understand the underlying process of dyspnea. The article clearly states that nebulized opioids are not effective for treatment of refractory dyspnea, citing previous research, but does not expand on this at all. Furthermore, the article describes the presence of opioid receptors situated in the bronchioles and alveolar walls which seems to contradict its conclusion
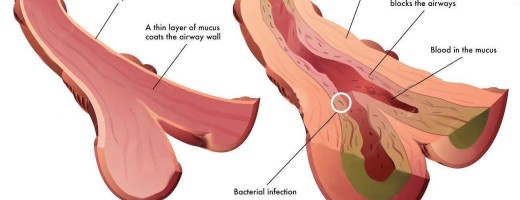
The effects of opioids and their mechanism of action are described by Mahler (2013): Opioids are produced in the body and relieve pain by binding to µ receptors in the peripheral and central nervous systems. The afferent signals of pain sent to the brain are inhibited thus decreasing the overall perception of discomfort. This inhibitory function is the scientific basis for the use of opioid treatment for refractory dyspnea as the lungs contain similar nociceptive pathways which cause feelings of discomfort and breathlessness and are believed to be inhibited by opioids.
There is support for the notion that some form of opioid is effective in managing refractory dyspnea is the conditions physiological mechanism. According to Mahler (2013) “Dyspnea is a warning signal that the usual unconscious awareness of breathing has been altered.” The article goes on to explain that normal stimulation of the lungs, such as oxygenated breathing, send signals to the brain that are mostly unconscious. Breathing only becomes conscious when these signals are disrupted and ones of discomfort are sent instead. The lungs contain afferent nerves in the bronchioles and alveolar wall which are capable of detecting discomfort. “The perception of dyspnea has been attributed to a mismatch, or imbalance, of afferent impulses from one or more sensory receptors and the outgoing central respiratory motor activity (demand to breathe) to the muscles of respiration (ability to breathe).” Opioids block signals of discomfort, which cause their analgesic effects, but can also potentially aid in the management of other forms of discomfort besides pain, such as respiratory distress.
While this article contains important information about the underlying mechanisms of action by which opioids suppress dyspnea, the conclusions of the author seem not to follow the evidence. As the article points out, there are nociceptors in the lung itself which are affected by opioids. The article does not make a strong case for why oral opioids should be used over nebulized opioids; rather it merely states that they should while providing evidence to the contrary.
2. (Gomutbutra, O'Riordan, & Pantilat, 2013). This article discusses the management of moderate-to-severe dyspnea in hospitalized patients receiving palliative care. A 2013 retroactive study was conducted on patient records from October 2005- October 2010, which consisted of 115 cases that met the eligibility criteria. The initial assessment consisted of 73% of patients with moderate dyspnea and 27% with severe dyspnea. At the follow up 74% reported an improvement of their dyspnea. Those patients that reported an improvement consisted of 42% that received only an orally administered opioid treatment, 37% that received an opioid treatment with benzodiazepines (BZDs), 2% that received only BZDs, and 19% that received neither treatment. The article concludes that most improvement in dyspnea was seen in those patients that had the treatment of opioids in conjunction with BZDs. However, further research should be conducted on the role of BZDs alone and in conjunction with opioid treatment for managing dyspnea.
This paper offers strong evidence that orally administered opioids are effective at managing dyspnea, even when administered on their own. There is nothing in this study that indicates oral opioids are more effective than nebulized opioids, rather only that orally administered opioids are in fact effective.
Evidence for Nebulized Opioids
3. (Cohen & Dawson, 2002). In this case study, a 10-year-old boy with end-stage cystic fibrosis that was admitted to the Walter Reed Army Medical Center exhibiting symptoms of fever, increasing home oxygen requirements, pleuritic chest pain, and severe dyspnea. Initially his treatment plan consisted of additional antibiotics, chest physical therapy, adjustment of his inspired oxygen concentration on the basis of repeated venous blood gases drawn through a central catheter. The patient’s dyspnea was not responsive to nebulized lidocaine treatment. Once palliative care was deemed appropriate he was placed on nebulized morphine in incremental doses ranging from 2.5 mg, 7.5 mg and 12.5 mg. After each treatment, the parameters documented to assess the patient's response were: change in dyspnea symptoms 1 hour after the treatment utilizing a visual analog scale, venous blood gases 30 minutes before and after treatment, serum morphine levels drawn 30 minutes after treatment, and blood pressure, heart rate, and respiratory rate before and 30 minutes after each nebulized treatment dose. The nebulized morphine treatment resulted in a mild effect on the patient's dyspnea.
Due to the anecdotal nature of this study, further research would need to be conducted to determine optimal dosing regimens and their efficacy. Furthermore, this study only demonstrates a single instance of nebulized opioids having benefit and more research is needed to make a stronger case for their use. This is something the authors themselves agree with in their conclusion.
4. (Hayes, Anstead, Warner, Kuhn, & Ballard, 2010). This article discusses a clinical case of a 48 year old man with cystic fibrosis whose medical condition included secondary infections, chest pain, and development of a narcotic dependency. His doctors treated him with heavy doses of both antibiotics and orally administered opioids. Despite this, he was transferred to palliative care where he was switched to an IV opioid, yet his pain and dyspnea continued. The patient's opioid dosages were raised and his pain became controlled but his dyspnea persisted. Eventually, he was administered a nebulized opioid which managed his dyspnea for the following two days until his death.
This is a case study with limited scope, though it does cite other incidences both supporting and opposing the idea that nebulized opioids are more effective that other administration routes for controlling refractory symptoms of cystic fibrosis. The results of the study are very clear in presenting nebulized opioids as an improvement over oral and even intravenous opioids in treating dyspnea. The article seems to interpret its data correctly and strengthens the work by Cohen and Dawson (2002) by offering further support for nebulized opioids.
5. (Sands et al., 2011). This article addresses the notion of advanced planning in end stage care for people with cystic fibrosis. Due to medical advances such as lung transplant, there is a critical period in which an individual and their family may need to decide whether to begin invasive life-prolonging procedures such as mechanical respiration while awaiting a lung transplant or to begin palliative care to reduce suffering. The article mentions the effectiveness of opioids in managing dyspnea and refers to nebulized opioids as having a varied level of effectiveness from patient to patient. It is mentioned that the majority of studies on this matter are retrospective. The article goes on to detail the process of preparing for life-prolonging procedures as well as palliative care and concludes that even with new breakthroughs in medical science, well planned end of life care is still needed.
The article seems to lean more towards palliative care than survival at all costs. At points, it could do a better job citing its sources or reasons for the ideas it expresses such as the fact that it does not actually cite any specific studies when it mentions the retrospective studies on nebulized opioids. The article demonstrates the framework in which palliative care is understood and the various obstacles to learning the most effective forms.
Unfortunately, little statistically significant research is available in the efficacy of nebulized opioids for treating dyspnea in cystic fibrosis. The majority of studies available on the topic that are not case studies are done retroactively, and instead look back through medical records to find instances where nebulized opioids were used. Furthermore, the nature of palliative care for patients with cystic fibrosis complicates the issue and means that many of them are either not placed on opioids, or are not on them long enough for doctors to try nebulized opioids as an alternative.
6. (Robinson, 2000). This article discusses the fact that little focus has been given to finding effective palliative care for end stage cystic fibrosis, with more research being given to treating the condition despite it being a terminal one. The article mentions that dyspnea is the primary symptom causing distress in people with end stage cystic fibrosis. The article details the difficulties in planning palliative care for people with cystic fibrosis such as the fact that it is difficult to identify short term mortality for the illness and therefore it is often hard for families to make the decision to put someone in palliative care since they may live longer. Patients with dyspnea are often treated with opioids, though some physicians are reluctant to do so given that opioids are respiratory depressants.
The article is more focused on the culture surrounding palliative care than on the science behind it, as is its purpose. It offers valuable insight into this culture, and it lends support to Sands et al, (2011) who point out that doctors will at times move to have their patient given a lung transplant rather than putting them on palliative care. Robinson (2000) expands on the barriers in palliative care and in reason that research into the subject is lacking.

Conclusion
Palliative care is a controversial topic at times in medicine, which is part of the reason little research exists on this topic. There are a great number of barriers standing in the way of research on the topic of nebulized opioids used to treat dyspnea in patients with end stage cystic fibrosis, and as such, evidence for its efficacy is mostly found in case studies done on individual patients such as those already cited in this paper.
This paper was meant to determine efficacy of nebulized opioids when compared with oral opioids. The five articles discussed range in their findings, with one opposed to nebulized opioids, some not having enough data to make a conclusion, and some in favor of nebulized opioids. There is evidence in the literature of the effectiveness for oral opioids, but there is not enough evidence to draw a conclusion on the effectiveness of nebulized opioids. There is also no evidence that indicates specifically that nebulized opioids are not effective. Further academic research would be required to understand this issue better. Additionally, it is worth noting that there is physiological evidence that supports the notion that opioids would be able to modulate the mechanism of action underlying dyspnea.
The uncertainty in drawing conclusions is due to a lack of research on the use of nebulized opioids as well as their lack of documented use at all in medical practice. The use of opioids for someone with severe lung function impairment, almost makes it certain the patient will not recover, and this fact makes the decision for their use difficult for families and medical professionals. This controversy is not the aim of this paper, but is worth mentioning as an explanation for the lack of any hard evidence that is itself not anecdotal in nature. In a similar vein, ethical standards greatly restrict what could be accomplished through experimentation. When enough instances of nebulized opioids being used are collected together, the data can be analysed in a statistically meaningful way from which to draw conclusions. Until such time, all that can be said is that oral opioids appear to be effective and the effectiveness of nebulized opioids is uncertain.
References
Cohen, S. P., & Dawson, T. C. (2002). Nebulized morphine as a treatment for dyspnea in a child with cystic fibrosis. Pediatrics, 38, 110-113.
Gomutbutra, P., O'Riordan, D. L., & Pantilat, S. Z. (2013). Management of moderate-to-severe dyspnea in hospitalized patients receiving palliative care. Journal of Pain and Symptom Managment, 45, 885-891.
Hayes Jr., D., Anstead, M. I., Warner, R. T., Kuhn, R. J., & Ballard, H. O. (2010). Inhaled morphine for palliation of dyspnea in end-stage cystic fibrosis. American Journal of Health-Systems Pharmacy, 67, 737-740.
Mahler, D. A. (2013). Opioids for refractory dyspnea. Expert Review of Respiratory Medicine, 7, 123-125.
Robinson, W. (2000). Palliative care in cystic fibrosis. Journal of Palliative Medicine, 3, 187-192.
Sands, D., Repetto, T., Dupont, L. J., Korzeniewska-Eksterowicz, A., Catastini, P., & Madge, S. (2011). End of life care for patients with cystic fibrosis. Journal of Cystic Fibrosis, 10, S37-S44.
© 2018 Vince