The General Clinical Significance Of Protozoal Infections And The Health Focus On Malaria
Protozoa Infected Patients

Protozoal Infections
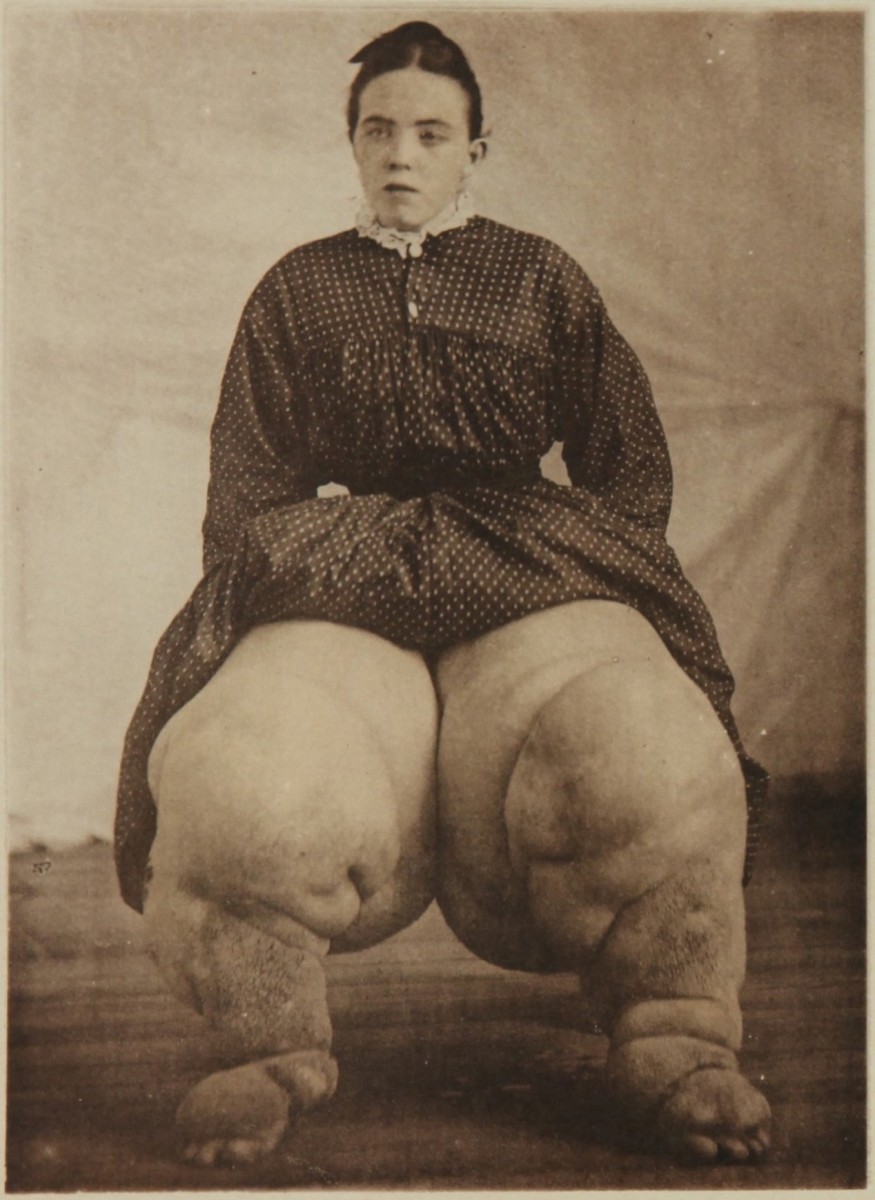
Several protozoa are found in humans. Some as pathogens, eg, Plasmodia and leishmania, and the others are commensals, eg, Entamoeba Coli. Though protozoa diseases are seen all over the world, they are much more common in the tropics. The major protozoa diseases include malaria, leishmaniasis, trypanosomiasis and amoebiasis.
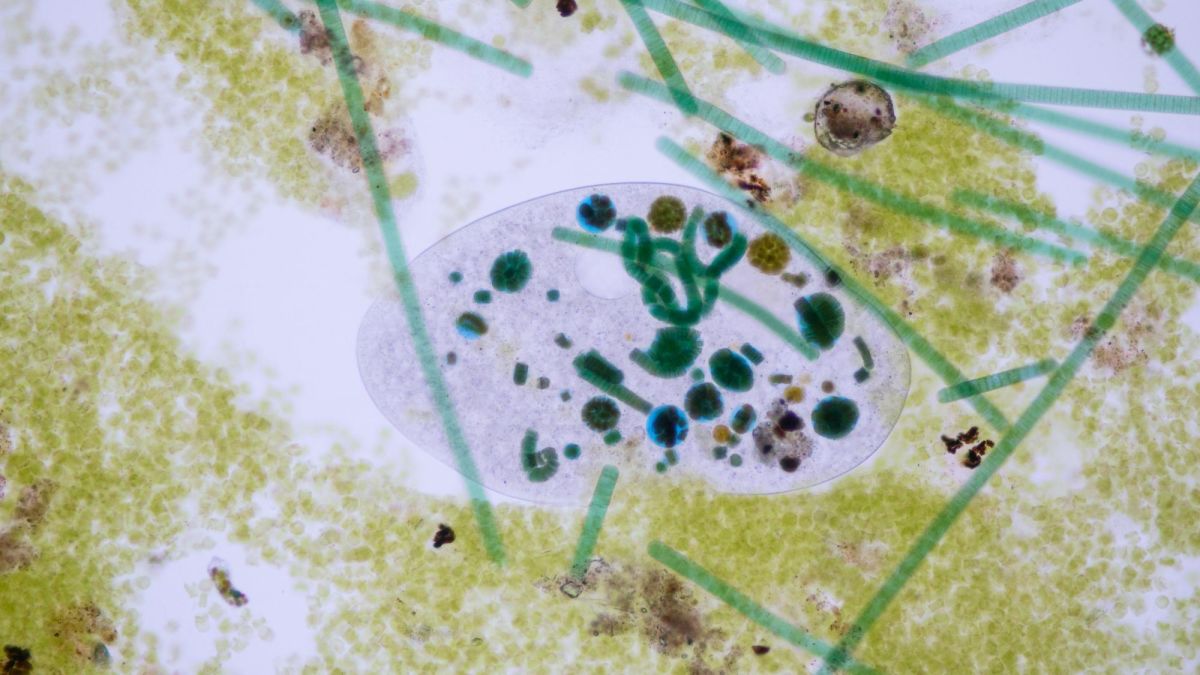
The protozoa are unicellular organisms containing cytoplasms, nuclei and other organelles. Based on the mode of locomotion, protozoa have been classified into flagellates, ciliates, amoebae and sporozoa. Even though differences exist between the different classes, divided into an outer ectoplasm and inner endoplasm. Both layers contain several organelles, the ectoplasms performs the functions of protection, locomotion, respiration, nutrition and excretion.
The nuclei is made up of fine delicate filaments studded with masses of chromatin granules and is enclosed by the nuclear membrane. The karyosome lies in the center of the nucleaus. It may be minute of large and conspicuous. Under adverse conditions, some protozoa like Amoeba change from the vegetative to the cystic form by encasing themselves in a tough membranous wall. The cysts are resistant to unfavourable environment. They are responsible for transmission from one host to another.
The Female Anopheles Mosquito

Infectious Diseases
Health Implications Of Malaria To Man
This is a febrile illness caused by the hemo-protozoa of the genus Plasmodium. It is characterized by periodic fever, splenomegaly, hemolytic anemia and a recurrent and chronic course. The plasmodia affecting man are P. vivax, P. falciparum, P. Ovale and P. malariae and they produce benign tertian, malignant tertian, ovale tertian and quartan malaria respectively.
Epidemiology: Malaria used to be the single largest killer of mankind before the middle of this century. Malaria is endemic in all tropical countries like India, Bangladesh, Sri Lanka, Burma, Middle East, Far East, several parts of Africa and tropical America. Present facilities for quick travel and migration of population have helped to introduce this disease in all countries. The disease is rare in stations above all altitude of 1500 meters or where the ambient temperature is low. Presence of sysceptible population, vector mosquitoes and availability of reservoir hosts determine the endemicity. Vivax malaria is more widespread, but in some parts, falciparum is more common. In the fifties, with aid from the WHO, national malaria eradication programs (NMEP) were initiated and many countries including India achieved considerable reduction in prevalence and incidence. The main strategy of this program was to detect and treat cases with drugs and destroy the vector by the use of DDT and other insecticides. In the seventies, the NMEP measures were slackened and the vector had also developed resistance to DDT and similar insecticides. Resistance of the parasite to drugs was also becoming more evident. Eradication of the disease from large areas also made the population more susceptible to fresh attack. All these factors contributed to the resurgence of malaria in the seventies and at present, malaria is still an important public health problem in most parts of the tropics.
In 1976, about fiften million cases of malaria occurred in Asia; ten million due to P.vivax and five million due to P. falciparum. Plasmodium ovale and P. malariae are only rarely seen. The vectors are female anopheles mosquitoes. They thrive in stagnant and running fresh water or brackish water.
The prevalence of malaria in a community is estimated by the spleen rate, parasite rate, infant parasite rate and other indices. Spleen rate represents the percentage of children aged 2 to 9 years showing palpable spleens. Parasite rate represents the percentage of positive cases of malaria detected by the positive cases of malaria detected by the examination of thick or thin blood films in a community. Infant parasite rate is the percentage of positives among children aged 0 to 11 months. This is closely related to the incidence of malaria.
In hyper and holoendemic areas, the local inhabitants develop immunity due to repeated encounter with the parasite. Such persons do not develop clinical disease even though parasites are demonstrable in blood. This phenomenon is called premunity. Children and new comers suffer heavily. In hypo- and mesoendemic areas, the local inhabitants do not acquire strong immunity and, therefore. Both local inhabitants and newcomers suffer.
© 2014 Funom Theophilus Makama