The Health Implications Of The Drug Resistance Of P. Falciparium In Malaria Attack
Persistence Of Malaria Infection Due To Drug Resistance

A General Overview
Plasmodium falciparum has developed resistance to the common suppressant drugs during the past two decades. In many areas, this has reached alarming proportions so as to render the standard antimalarial drugs virtually ineffective. When a parasite strain is able to survive, multiply, or both, even after the administration and absorption of adequate recommended therapeutic dose or a higher dose of an active schizontidical drug, it is considered resistant (WHO, 1967)
Classification Of Anti-Malarial Drugs
Name
| Route
| Remarks
|
|---|---|---|
Schizonticidal drugs
| ||
Chloroquine (4 amino quinolone group) diphosphate & Sulphate
| 150 mg base (1 tab); oral
| Most effective schizonticidal drug, except in resistant P. falciparum. It shows cross-resistance (CR) with mepacrine
|
Chloroquine hydrochloride
| 200 mg; intramuscular or intravenous
| Used for pernicious malaria
|
Amodiaquin (4 aminoquinolone group) (Camoquin)
| 200 mg tab; oral
| Same as above
|
Mepacrine (4 acridine dye)
| 100 mg tab; oral
| Powerful schizonticidal drug, rarely used now due to side effects; shows cross-resistance with chloriquine
|
Quinine (alkaloid)
| 260/325 mg tablets; oral
| Schizonticide
|
Quinine sulphate
| 325 mg tablets; oral
| Schizonticide
|
Quinine ethyl carbonate
| Same as Sulphates; oral
| For pernicious and resistant forms, less bitter, used for children.
|
Quinine dihydrochloride
| 500 to 650 mg; intravenous solution
| For pernicious and resistant forms (quinine is not freely available at present)
|
Proguanil (Synthetic biguanide)
| 100 mg tablet; oral
| It is a weak schizonticide effective in semi-immunes it is a good causal prophylactic and it inhibits sexual cycle in mosquito
|
Pyrimethamine
| 25 mg tablet; oral
| Causal prophylaxis, inhibits sexual cycle in mosquito and shows cross resistance with proguanil
|
Sulfodoxine (long acting sulphonamide)
| 0.5 mg tablet; oral
| Schizonticide used for resistant P. falciparum in combination with pyrimethamine (Fansidar, Croydoxin, Malocide). Pyrimethamine 25 mg + Sulfodoxine 0.5g
|
Mefloquine (a quinoline methanol)
| 0.5 mg tablet; oral
| Schizonticide used for resistant P.falciparum in a single dose of 1500 mg.
|
Cotrimoxazole
| Trimethoprim 80 mg + Sulphamethoxazole 400 mg tablets; oral
| Schizonticide used for resistant P.falciparum
|
Tetracycline
| 250 mg capsules
| Slowly acting schizonticide
|
Dapsone
| 100 mg tablets; oral
| Weak schizonticide. If combined with 25 mg pyrimethamine, it is used for resistant P. falciparum pyrimethamine 25 mg + Dapsone 100 mg- Maloprim
|
Metakalfin
| Sulphalene 500 mg + pyrimethamine 25 mg; oral
| Effective in resistant P. falciparum
|
Drug used for eradication
| ||
Primaquine (8-aminoquinoline group)
| 2.5/7.5 mg tablets; oral
| Effectively eradicates the exo-erythrocytic cycle, kills gametocytes, and weakly schizonticidal
|
Malaria Attack Treatment

Treatment Of An Overt Attack
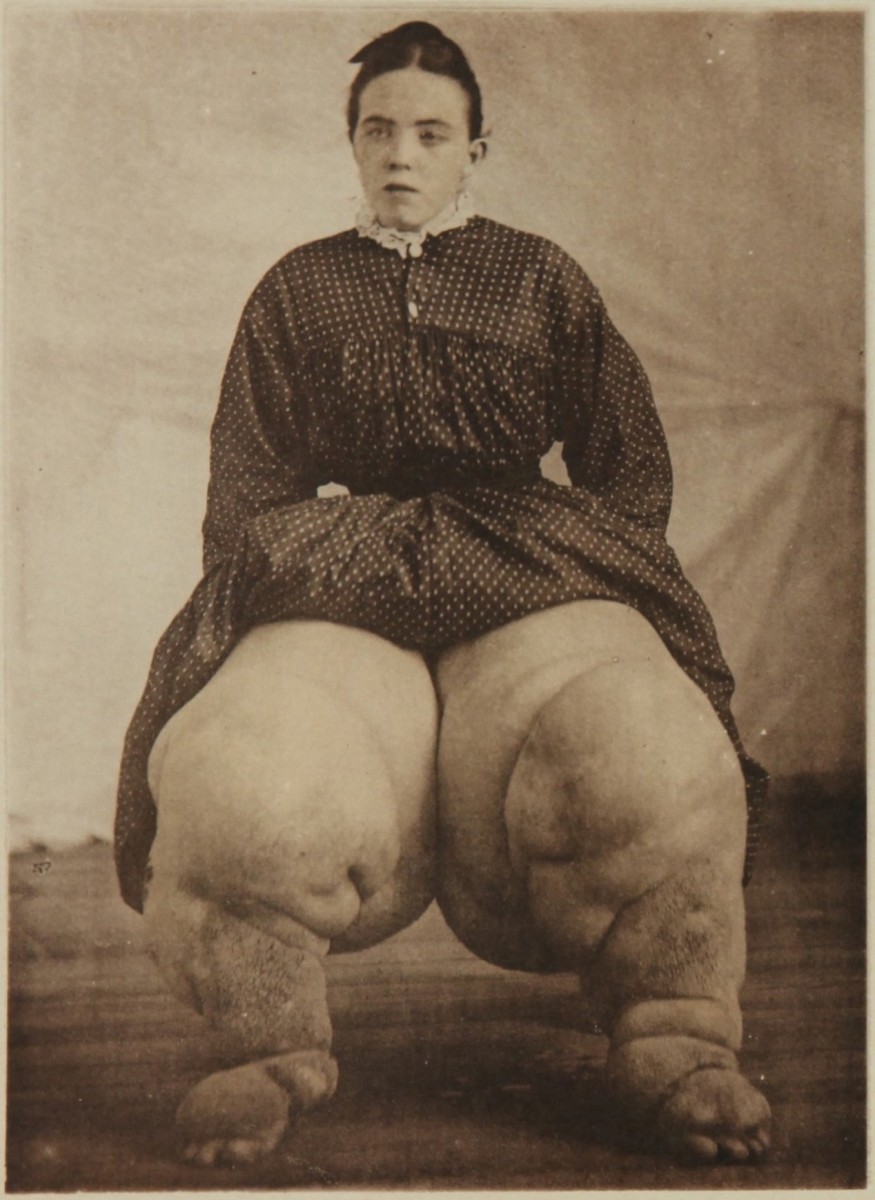
The drug of choice is chloroquine or amodiaquine, if the parasites are sensitive. The initial dose of 600 mg of the base (4 tablets) is given orally. It is followed six hours later by 300 mg (2 tabs) and then 150 mg (1 tab) twice a day for 3 to 7 days. For children, the initial dose is 5 to 10 mg/Kg body weight. Semi-immunes may respond to a single dose of 600 mg. Troublesome side effects include allergy, gastritis, dermatitis, psychosis, convulsions, photosensitization and deposition of the drug in the cornea and retina. When the drug is withdrawn, the corneal deposits clear up, but the retinal deposites set up adverse reactions which lead to visual loss. Therefore, ocular toxicity is an absolute contraindication to further chloroquine therapy. Alternative drugs are:
- Amodiaquine in a dose of 600 mg on the first day and then 400 mg daily for two more days;
- Quinine sulphate, 650 mg twice a day for 10 days; or
- Mepacrine 300 mg thrice on the first day, 200 mg thrice on the second day and 100 mg thrice a day for five days.
Adverse effects of quinine are gastrointestinal irritation, allergy, amblyopia, optic neuritis, myocarditis (especially, if given intravenously), deafness due to VIII cranial nerve damage and precipitation of black water fever. Mepacrine is seldom used at present due to toxicity. Toxicity includes psychosis, yellow staining of the skin, hair and nails, lichen planus, allergy and granulocytopenia.
© 2014 Funom Theophilus Makama