The Importance of Weight Management for Osteoarthritis

Obesity is rapidly becoming an epidemic, and as most of us know, it is one of the leading causes of severe health problems such as diabetes, hypertension and heart disease. But it can also cause less life threatening health problems such as osteoarthritis, which can lead to a life of chronic pain. It can also exacerbate symptoms in those who already have the disease.
To understand how obesity affects osteoarthritis, we need to know what the disease is and how it works.
What is Osteoarthritis?
Osteoarthritis is a degenerative disease of the joints that develops as we age, or in response to an injury. It typically affects joints that are exposed to repetitive movements such as the wrist in carpel tunnel syndrome. It’s been nicknamed the “wear and tear” disease for this reason. When we walk, move our arms, bend our elbows, even shrug our shoulders, the joints in these areas do all the work. Let’s take the knees for example.
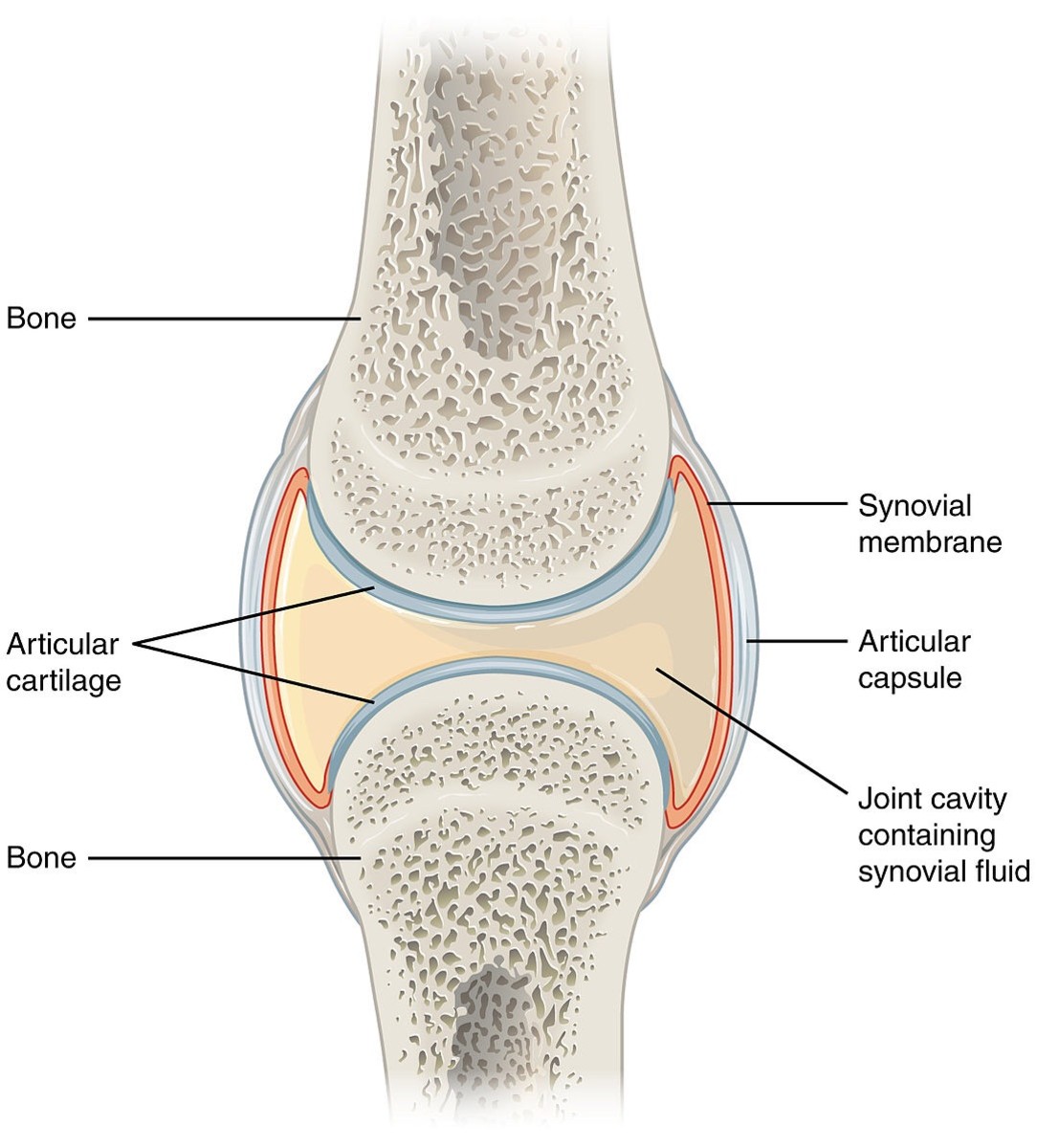
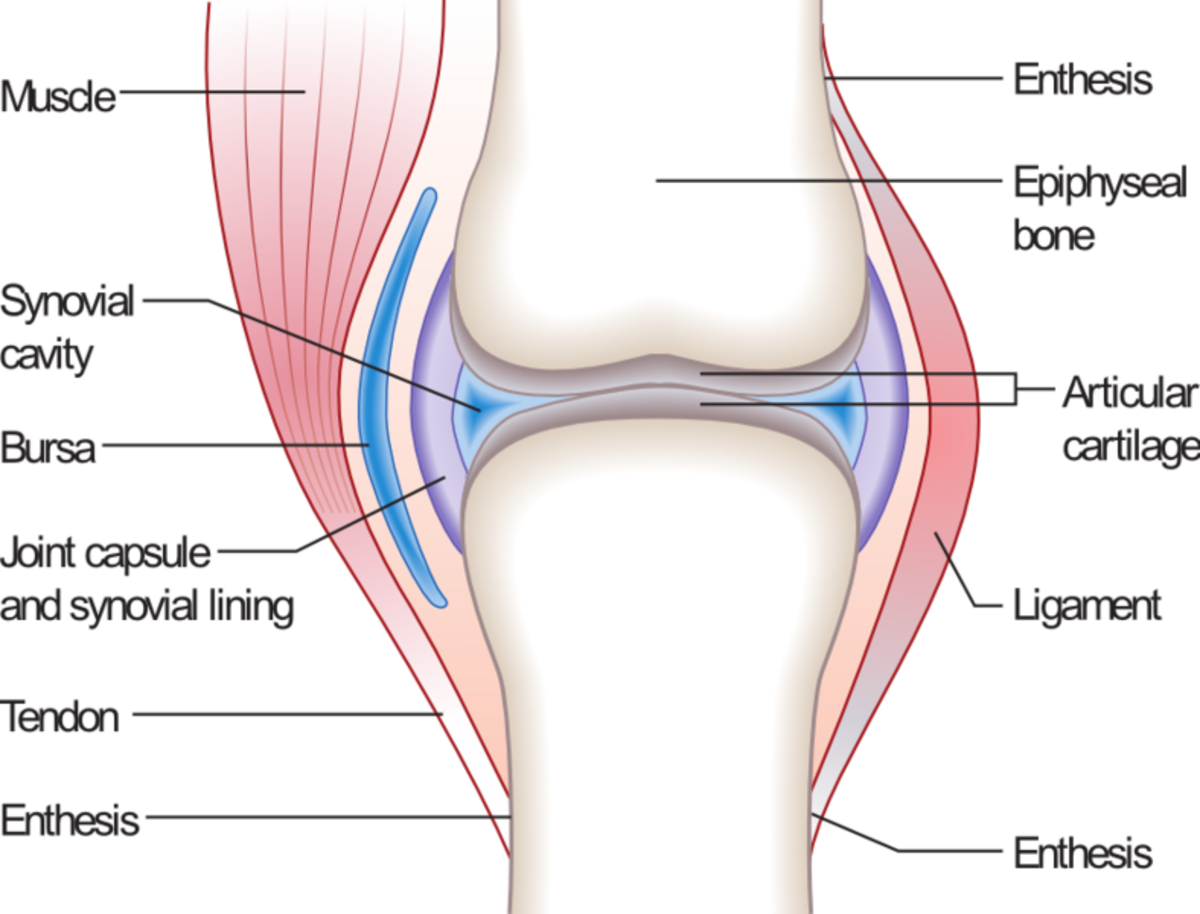
The femur (the long bone of the thigh) and the tibia and fibula (the two bones in the lower leg) form a joint we all know as the knee. On the ends of each bone that make up this joint is articular cartilage, which is essentially extra padding that helps to absorb the shock of each step we take. All of our joints have this extra padding.
In between the articular cartilage of each bone of the joint is a cavity called the synovial cavity, which is filled with synovial fluid. This fluid acts like the shocks on a car. It absorbs the majority of the shock, while preventing friction in an effort to protect the bone.
Anatomy of a Joint
Do you or someone you know have osteoarthritis?
Here’s where the “wear and tear” comes into play. As we get older, this articular cartilage begins to wear down and the synovial fluid begins to degrade.
Friction begins to exert its effects on the articular cartilage causing it to wear down like the tread on a tire. This eventually causes the bones to rub together causing more friction. Inflammation will typically develop as a result eventually leading to chronic pain.
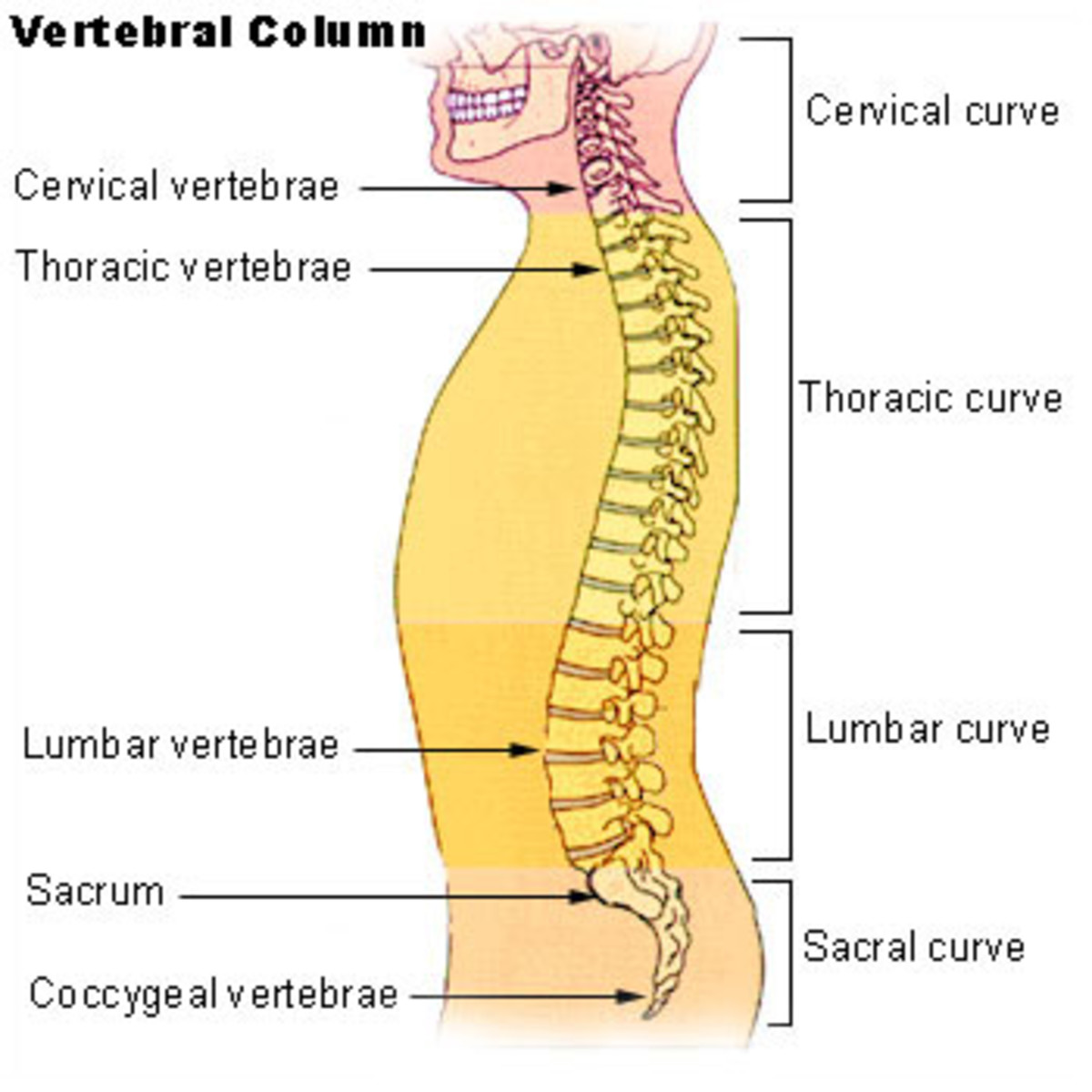
Osteoarthritis symptoms vary, but typically the pain it causes is described as a burning sensation in the tendons and ligaments, or a dull aching sensation. It can develop anywhere in the body including the neck, back, hips, hands, and feet. The neck, back, knees and hips are the most commonly affected joints.
As the disease progresses, the patient can experience a “cracking” noise known as crepitus, which occurs after sitting or lying down for long periods of time and then getting up. This is the result of a build up of nitrogen in the synovial fluid, which is released when the joint is moved causing a cracking or popping sound.
Locking can be another symptom of the disease and can be very uncomfortable. It is caused by small fragments of cartilage or bone that can cause the joint to become temporarily immobilized, or locked.
Locking typically affects the fingers, hands and feet, but can affect any joint. With a bit of manipulation, the patient can usually free the joint. Bone spurs, called osteophytes, can also cause locking. These are bony growths that develop on the ends of the bones in a joint, typically in response to excess wear and tear or injury.

How Does Obesity Affect Osteoarthritis?
Since osteoarthritis more commonly affects the weight bearing joints such as the hips and knees, being even a little bit overweight can put an extreme amount of pressure on these joints.
The weight bearing joints are subjected to a pressure equaling about three times our weight just when we’re walking, so even five or 10 extra pounds can cause damage to the joints. For example, if you are 20lbs overweight, you add an extra 60lbs of pressure to the knees and hips as you walk. Can you imagine someone who is 100, 200, or 300 lbs over weight?
This extra pressure exacerbates the “wear and tear” effect on the joints, which speeds up the degeneration process. People who are obese develop osteoarthritis much earlier in life than those who are not. They also typically go through joint replacement surgery at a much younger age and many times need a second joint replacement 10 to 15 years after the first.

Treatment of Osteoarthritis
The treatment for this disease is typically analgesics, or pain relievers such as Tylenol, Ibuprofen and Aleve.
For more severe cases, prescription analgesic and anti-inflammatory medications such as Voltaren (oral pill and gel form), tramadol (Ultram), and even narcotic painkillers such as Hydrocodone (Vicodin) are effective.
However, there comes a time when pain killers no longer work, and the patient needs the joint replaced. In fact, about one million people have joint replacement surgery every year. But replacing a joint isn’t an easy task, and it carries with it considerable risk.
Replacing a joint can also limit a person’s activities after the procedure, although many people undergo the surgery to continue living active lifestyles. Jogging and running can and will decrease the lifespan of the new joint, and can lead to the necessity of a second joint replacement later in life.
Do you exercise regularly?
The Benefit of Exercise
The best treatment of osteoarthritis caused by obesity is to lose the weight. In fact, exercise can go a long way in relieving the chronic pain and other symptoms of the disease.
When we exercise, we increase the strength of the muscles and ligaments around the joints, and this can help support the joints, and limit friction. Plus, there’s the added benefit of weight loss.
The problem with exercise for many patients with osteoarthritis is the pain. It’s very difficult to exercise when you’re in pain; I know this from personal experience. But there are ways around this problem.
For example, low impact exercises or swimming exercises can be very beneficial in improving cardiac as well as muscle strength without putting a lot of extra pressure on the joints. Low impact exercises that use body weight to build strength also strengthen the bone as well.
Diet and Osteoarthritis
Diet can also make a big difference in osteoarthritis, and not just because it aids in weight loss. Eating lots of fruits and veggies can help slow down osteoarthritis and may even help prevent it.
The antioxidants in these foods (especially Vitamin C and Vitamin E) help the body to “take out the cellular trash,” or the waste produced during our daily metabolic functions, which can exacerbate the effects of wear and tear if left in the joints. This process is called phagocytosis.
Refraining from animal products either completely or limiting them to one to two times a week can also make a big difference in the development of osteoarthritis. Animal products cause our body’s pH to become acidic. To neutralize this problem, the body uses calcium, which it strips from the bone. This causes the bone to become weak and brittle, speeding up the degeneration process and leading to osteoarthritis and eventually osteoporosis.
The bottom line? If you’re overweight, you need to lose the extra pounds, but do so safely. Check with your doctor before you start an exercise program. He or she can tell you if exercise will help your osteoarthritis or exacerbate it and which exercises will be most beneficial for your specific case.
© Copyright 2013 - 2015 by Melissa "Daughter of Maat" Flagg ALL RIGHTS RESERVED