The Role of Gonorrhea and Chlamydia in Pelvic inflammatory disease (PID)

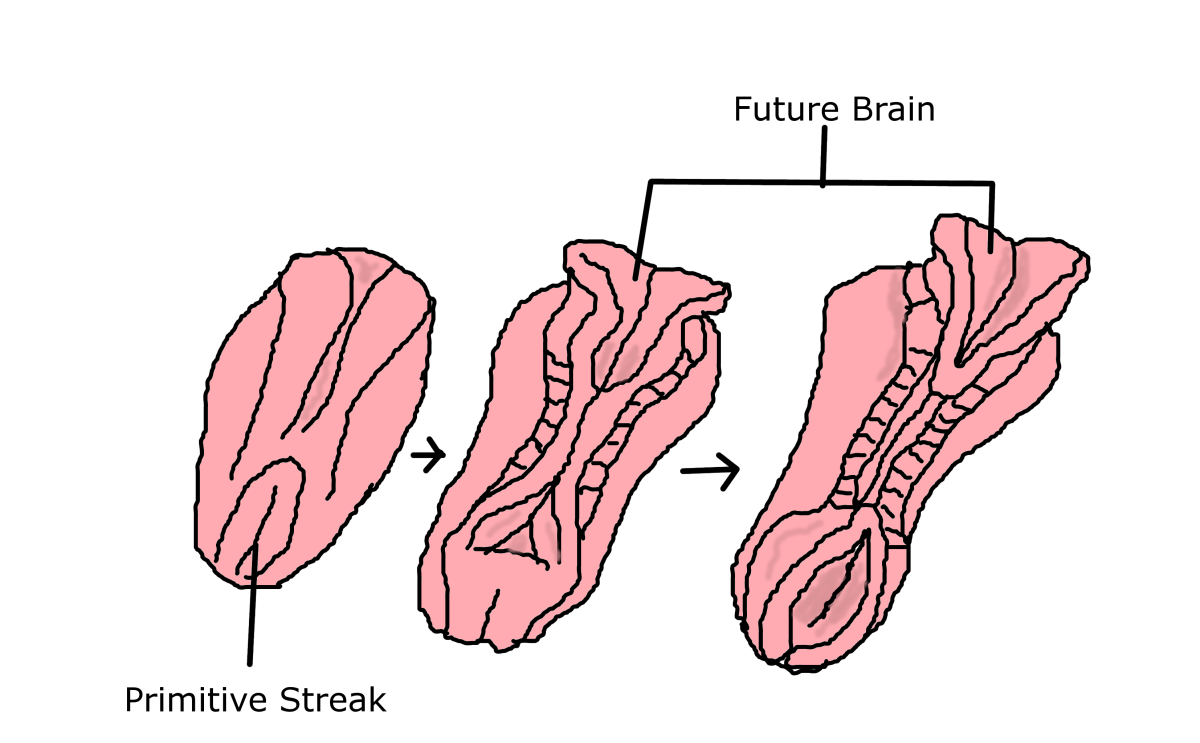
Although it can vary a good deal, the actual progress of gonorrhea or Chlamydia to Pelvic Inflammatory Disease (PID) is the same. These infections spread from your cervix up into your uterus and along your fallopian tubes, causing inflammation.
As this inflammation develops, the lining of your fallopian tubes becomes swollen and scarred, and the walls become distorted and stuck together. Over time, the passage down which a fertilized egg should pass becomes blocked.
Symptoms of Pelvic Inflammatory Disease
At first you feel vague pain in your pelvis. You may notice deep pain on intercourse, which may be bad enough to stop you having sex. Depending on the severity of the infection, you may become generally unwell. The most severe pain requires admission to hospital and antibiotics given through a drip.
Less severe, grumbling pain may last for weeks or months and is often diagnosed incorrectly at first because it is hard to place the actual origin of the symptoms. The mildest form of Pelvic Inflammatory Disease produces so little in the way of symptoms that you may be unaware that you ever had it, until, that is, you are told that your fallopian tubes are blocked as a result.
Risks of Pelvic Inflammatory Disease
Infertility is a serious consequence of Pelvic Inflammatory Disease, as is the increased risk of having an ectopic pregnancy. Ectopic pregnancy occurs when an already fertilized egg is halted in its tracks, and prevented from passing into the uterus by the scarring from Pelvic Inflammatory Disease. The fertilized egg grows in the tube at the point where it lodges. At about six weeks of pregnancy, it can rupture out of the tube, causing sudden, severe, internal bleeding that is life threatening.