The War on Drugs is A War on Mental Health: MDMA

MDMA, also sometimes incorrectly labeled as “molly” or “ecstasy”, has been modernly perceived as a party drug. It was synthesized in 1912 by German scientists to be used as a pharmaceutical. MDMA eventually had its psychoactive properties researched by the CIA as part of MK-ULTRA; highly classified mind-control research conducted by the U.S. Government in the 1950s. In the 1980s, the rave and recreational culture surrounding MDMA led to its banning by the DEA in 1985 (1).
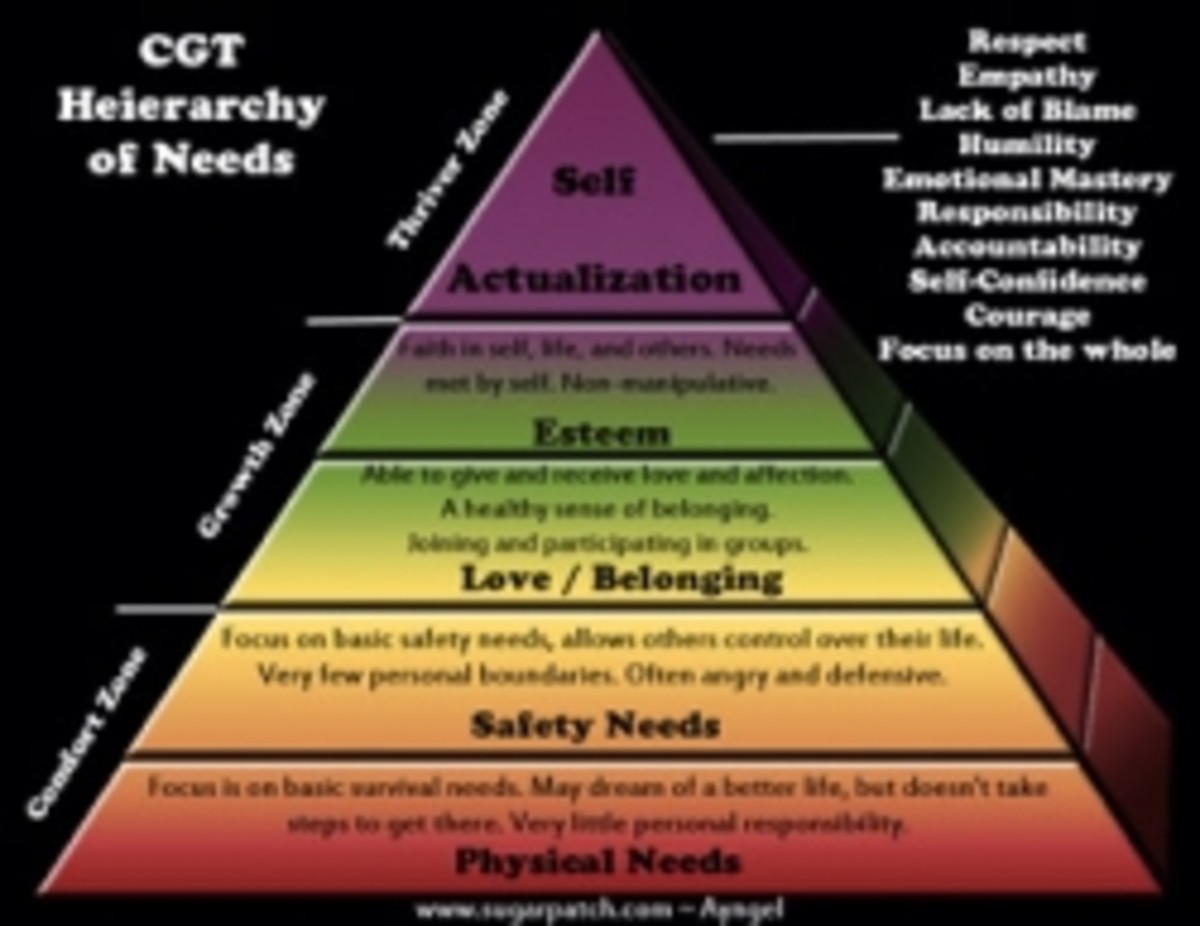
The effects of MDMA can be both positive and negative. On the plus side, the drug creates a feeling of euphoria and compassion, often leaving the user feeling emotionally healed. Contrarily, long-term use of the substance may cause difficulty with memory and depression, including damage to the serotonin system. “Ecstasy” and “Molly” are usually confused with MDMA, although the former can contain other mixed substances that may lead to a higher chance of unwanted health problems. Research has shown that short-term use is generally safe (2).
Would you believe me if I told you that in 2018, a double-blind study conducted by the British Association for Psychopharmacology resulted in 76 percent of PTSD patients being cured? That means 28 PTSD-diagnosed patients participated in the study, with only about 7 people needing further treatment after a 12-month checkup (3). According to the Multidisciplinary Association for Psychedelic Studies, “at least one in two PTSD patients cannot tolerate or do not respond adequately to existing treatments”. Alternative Medicine is in high demand, and there is substantial evidence pointing to MDMA as a breakthrough solution.
As of August 26th, 2017, MDMA is undergoing phase three of the FDA’s rigorous clinical trial. There are five phases, the third phase consisting of researchers studying the reaction of the drug on the human body. MDMA was granted a “Breakthrough Therapy Designation” by the FDA. The Food and Drug Administration classifies this designation as “a process designed to expedite the development and review of drugs that are intended to treat a serious condition and preliminary clinical evidence indicates that the drug may demonstrate substantial improvement over available therapy on a clinically significant endpoint(s).” (4). The expected completion date is estimated to be sometime in 2021 and could make the drug available as a prescription.
Last year it is estimated that 30.5 million U.S. citizens used benzodiazepines, the pharmaceutical name for mental relaxation drugs like xanax and valium (5). These drugs combat symptoms of anxiety and depression, and are also highly addictive. According to the National Institute on Drug Abuse, more than 30 percent of overdoses involving opioids also involve benzodiazepines (6). What if there were a safer prescription that could lower the public’s dependence on addictive prescription drugs? What if most patients could still feel cured of mental illness 12 months after their first treatment? The research has shown that even with minimal treatment, a large portion of patients can end up free from PTSD, anxiety, and depression. MDMA may be an important catalyst for the overhaul of U.S. drug policy, as other illegal substances slowly make their way through the FDA’s trial process. There is no easy answer to defeating mental illness, but the way is being paved to replace outdated methods that lead to addiction.
Do you support the legalization of medicinal MDMA?
Sources
(1) History.com Editors. “MDMA.” History.com, A&E Television Networks, 31 May 2017, www.history.com/topics/crime/history-of-mdma.
(2) Lawton, Graham. “Ecstasys Long-Term Effects Revealed.” MAPS, Feb. 2009, maps.org/news/media/596-ecstasy's-long-term-effects-revealed.
(3) Grigsby, Jim, et al. “3,4-Methylenedioxymethamphetamine-Assisted Psychotherapy for Treatment of Chronic Posttraumatic Stress Disorder: A Randomized Phase 2 Controlled Trial - Marcela Ot'alora G, Jim Grigsby, Bruce Poulter, Joseph W Van Derveer, Sara Gael Giron, Lisa Jerome, Allison A Feduccia, Scott Hamilton, Berra Yazar-Klosinski, Amy Emerson, Michael C Mithoefer, Rick Doblin, 2018.” SAGE Journals, Oct. 2018, journals.sagepub.com/doi/full/10.1177/0269881118806297.
(4) Unknown. “Breakthrough Therapy.” U.S. Food and Drug Administration, FDA, 2018, www.fda.gov/patients/fast-track-breakthrough-therapy-accelerated-approval-priority-review/breakthrough-therapy.
(5) National Institute on Drug Abuse, National Institute on Drug Abuse. “Research Suggests Benzodiazepine Use Is High While Use Disorder Rates Are Low.” NIDA, 18 Oct. 2018, www.drugabuse.gov/news-events/latest-science/research-suggests-benzodiazepine-use-high-while-use-disorder-rates-are-low.
(6) National Institute on Drug Abuse. “Research Suggests Benzodiazepine Use Is High While Use Disorder Rates Are Low.” NIDA, 18 Oct. 2018, www.drugabuse.gov/news-events/latest-science/research-suggests-benzodiazepine-use-high-while-use-disorder-rates-are-low.