Traumatic Brain Injury (TBI) Facts
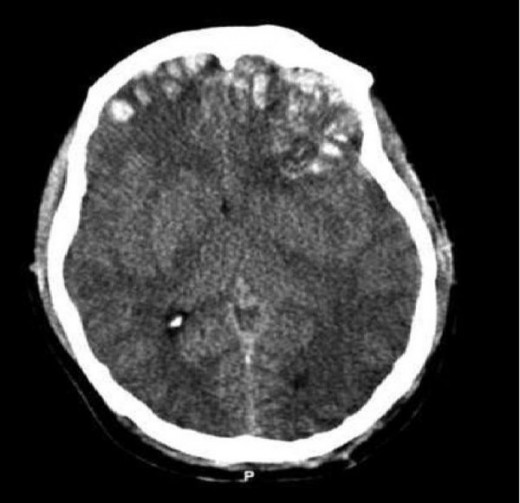
Brain Injury Scan
Traumatic Brain Injury Statistics
Traumatic brain injuries (TBI) were first described in the 16th century by recounting the symptoms. Currently, 2.8 million people suffer from TBIs each year in the U.S. and 50,000 die annually. Adults 75 years or older are at the highest risk for these injuries. Falls are the leading cause of death for people over 65 years old, and brain injuries are common for children from 0-4 years of age. Between 2006-2014, brain injuries increased in the U.S. by 53%.
The next most common patients are children between 0-4 years old, then from 15 to 19 years of age. Worldwide 69 million people suffer from TBIs annually. In the U.K. TBIs are the most common cause of death for men under 40 years of age. Motor vehicle accidents are the second leading cause of TBIs, particularly for 15 to 44 year olds.
Definition of Traumatic Brain Injury
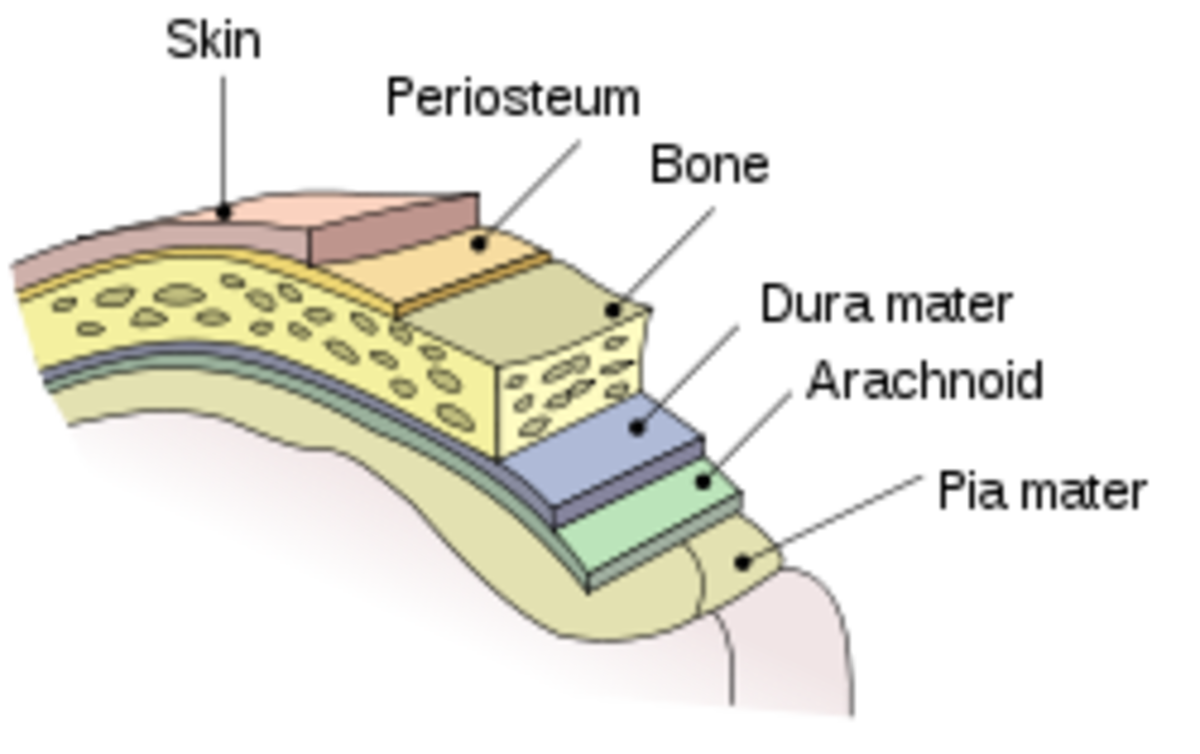
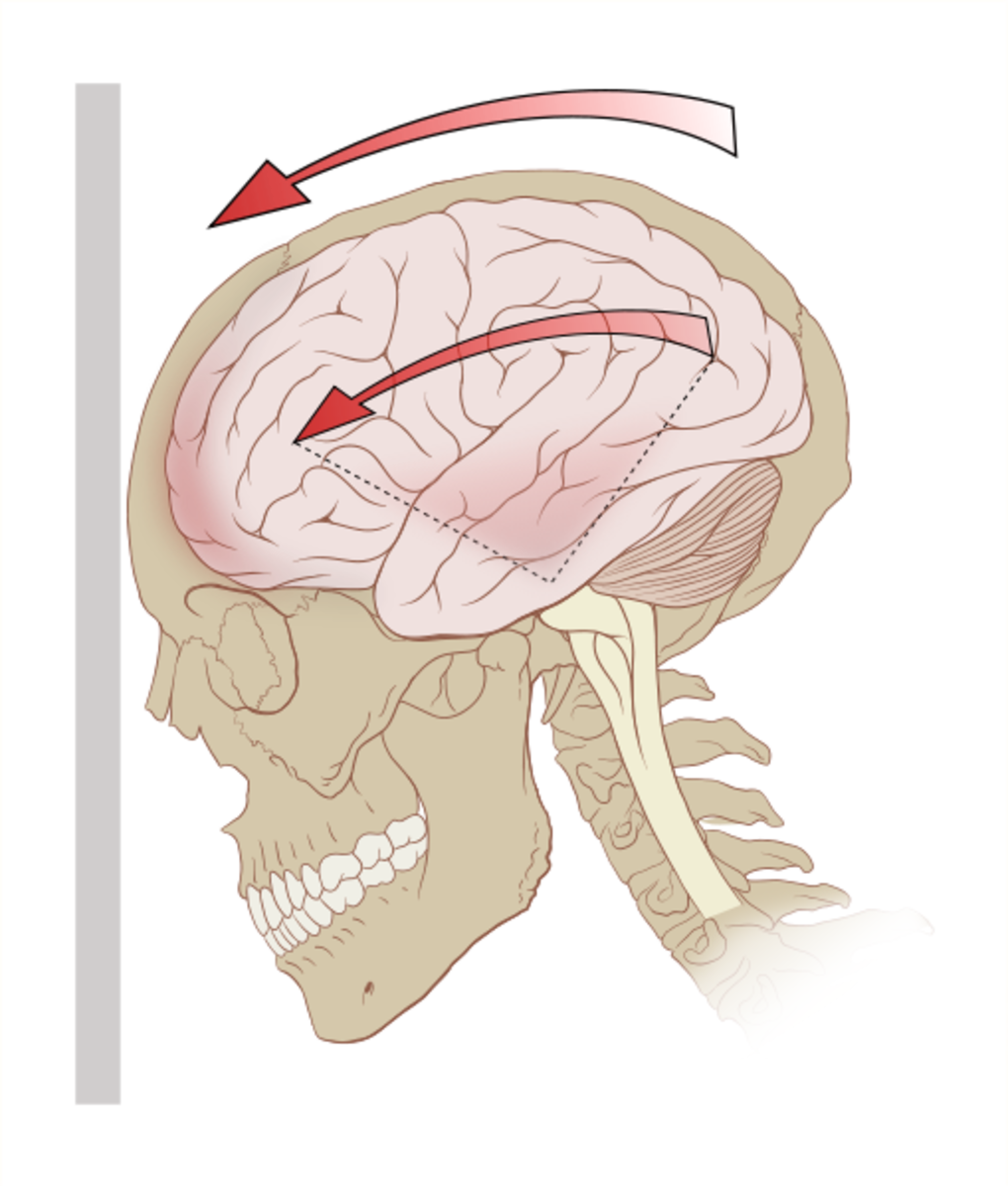
A traumatic injury is a noncongenital, nondegenerative insult to the brain, which occurs due to a strike to the head, a fall or a motor vehicle accident that affects brain function. In the U.S. it is a serious public health risk. TBIs can lead to temporary or permanent impairment of physical, cognitive or psychosocial function. TBIs must be treated quickly as the consequences can rapidly deteriorate without medical intervention.
Head Injuries 5, Primary Brain Injuries
Traumatic Brain Injury Symptoms
The symptoms of TBIs may appear immediately and other symptoms may not appear days, months or even after the patient returns to regular activities.
Four categories of TBIs with physical symptoms, emotional or mood changes and sleep patterns include the following:
- Difficulty in thinking clearly - headaches, fuzzy or blurry vision, irritability, sleeping more than usual
- Feeling slowed down - nausea or vomiting as an early symptoms, then dizziness, sadness, sleeping less than usual
- Difficulty concentrating - sensitivity to noise or light sensitivity and balance problems, more emotional and trouble falling to sleep
- Difficulty remembering new information - feeling tired or having no energy, nervousness or anxiety
In the United States in 2014, an average of 155 people daily died from TBI injuries. The survivors faced significant effects of their injury that lasted from days to the rest of their lives, which depended on the category of their injury.
TBI Danger Symptoms

Diagnosing Traumatic Brain Injuries
Physicians use the Glasgow Coma Scale, which is a 15 point scale to evaluate a patient. They evaluate the patient's ability to follow directions and move their limbs and their eyelids.
Altered consciousness is certainly the first symptom to recognize. Seizures and fluid that is built up in the brain are serious symptoms. If there is a penetrating head wound then infection is a possibility. A bleed in the brain is very significant and it may be diagnosed by an MRI. The MRI can also show a small area of bruising (contusion) or scarring (gliosis). Complaints of vertigo and headaches are also important.
Other symptoms include:
- Dizziness
- Ringing in the ears
- Paralysis of facial muscles and losing the sensation in the face
- Loss or altered sense of smell
- Loss or altered sense of taste
- Problems with swallowing
- Loss of hearing
The cognitive functions of memory, learning, judgment, reasoning and concentration or paying attention may be a factor. Difficulty in understanding speech, writing, speaking or having trouble following a conversation are also symptoms.
Moderate to Severe Brain Injury Symptoms
Mayo Clinic lists the symptoms of moderate to severe as follows:
“Physical symptoms
-
Loss of consciousness from several minutes to hours
-
Persistent headache or headache that worsens
-
Repeated vomiting or nausea
-
Convulsions or seizures
-
Dilation of one or both pupils of the eyes
-
Clear fluids draining from the nose or ears
-
Inability to awaken from sleep
-
Weakness or numbness in fingers and toes
-
Loss of coordination
Cognitive or mental symptoms
-
Profound confusion
-
Agitation, combativeness or other unusual behavior
-
Slurred speech
-
Coma and other disorders of consciousness”
Soldier

Military Personal Traumatic Brain Injuries
Mild TBIs are the most common diagnosis for our military, and they are the most difficult to diagnose. They are also the least well understood. They usually occur due to explosive blast from improvised explosive devices. Injuries may occur from blast exposures due to IEDs, land mines, suicide bombers, rocket-propelled grenades and mortar rouneds.
Current combat operations are directly impacted by these injuries, so they affect the level of unit readiness and troop retention in each branch of the service.
The bigger concern is the number of veterans coming home with traumatic brain injuries and post traumatic stress syndrome who have suicidal idealations. One third of these veterans that do commit suicide. The veterans from Iraq/Afghanistan have a higher rate of TBis compared to previous military conflicts due to changes in warfare tactics. There are more frequent improvised explosive device attacks now.
Football Players

Professional Football Players Risk of TBI’s
A study of 111 deceased football players who had TBI’s showed 110 players had chronic traumatic encephalopathy (CTS). This is a degenerative brain disorder that is associated with TBIs. In 2017, a study of 202 deceased players researchers found that 177 had been diagnosed with CTE.
Fewer boys are participating in high school football due to the fear of head injuries. The NFL has changed several rules to try and prevent TBIs. The kickoffs have been moved from 30 to the 35 yard line and touchbacks have been changed from 20 to 25 yard line. Football helmets have been upgraded over the years. If a player has a possible concussion they are benched for the rest of the game and they may not play until they are cleared by a doctor. Penalties for unnecessary roughness have also increased.
Finding Hope After Traumatic Brain Injury: Corey Davis’s Story
Treatments for TBIs
Diuretics are often given to treat extra fluid that may cause swelling in the brain. Antiseizure medications are administered as there is a risk of seizures during the first week after a serious brain injury. Patients are sometimes put into a coma following a serious head injury as the brain needs less oxygen to function and they are placed in intensive care.
I have cared for head trauma patients as an RN in ICU. There are rare times when the injuries are so serious we drained cerebral spinal fluid from the brain and kept the patient’s blood pressure at a lower but stable rate.
Surgery may be necessary for repairing skull fractures, for a brain bleed or removing clotted blood.
Recovery
A physiatrist often oversees the rehabilitation process as they are doctors trained in physical medicine. They manage the medical rehabilitation, prescribe medicine as needed and work with other care providers. They may include an occupational therapist, physical therapist, speech therapist, rehabilitation nurse, vocation counselor or a neuropsychologist.
Patients are encouraged to follow a routine, write things down, attend a support group and to stay focused.
Numerous clinical studies are in progress at top hospitals with promising results, but there is still a long way to go before serious TBIs do not have lifelong disabilities.
In Conclusion
A moderate or serious traumatic brain injury may lead to long term may cause permanent physical or mental disabilities. About 60% of moderate TBI patients will recover very well over time, but about 25% will have a moderate amount of disability. While TBIs are being diagnosed more rapidly, there are still many long term disabilities associated with these injuries.
References
- https://emedicine.medscape.com/article/326510-overview
- https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/diagnosis-treatment/drc-20378561
- https://en.wikipedia.org/wiki/Traumatic_brain_injury
- http://www.center4research.org/football-brain-injuries-need-know/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5501743/
This content is accurate and true to the best of the author’s knowledge and does not substitute for diagnosis, prognosis, treatment, prescription, and/or dietary advice from a licensed health professional. Drugs, supplements, and natural remedies may have dangerous side effects. If pregnant or nursing, consult with a qualified provider on an individual basis. Seek immediate help if you are experiencing a medical emergency.
© 2019 Pamela Oglesby