Treatment And Prevention Of Rubella And Clinical Manifestations Of Herpes Simplex
The Best Way Of Preventing Rubella Is Through Vaccination

Rubella Treatment And Prevention
Treatment: As the disease is generally benign, it is desirable to acquire rubella before the child-bearing ages. No specific treatment is indicated. Rubella occurring in women in the first 16 weeks of pregnancy leads to fetal malformation in up to 50% cases. Risk of fetal affection reduces as the pregnancy advances. Medical termination of pregnancy has to be considered if there is proof of rubella infection in early pregnancy.
Prevention: Vaccination using live attenuated vaccines has been in vogue. Live attenuated rubella virus RA 27/d grown in human diploid fibroblast cells is effective, when given in a dose of 0.5ml as a single injection. Vaccination confers solid immunity for 7 to 9 years. If facilities are available, vaccination should be considered for girls in the age groups of 11 to 13 years and women in the child-bearing age who are antibody-negative and are desirous of child-bearing. The vaccine virus passes into the letus and so pregnancy should be avoided for eight weeks following vaccination. Gammaglobulin administered to the mother after exposure aborts an overt attack, but safety of the fetus cannot be guaranteed.
The Physical Presentation Of Herpes Simplex Viral Infection

Infectious Diseases
Herpes Simplex (Herpes Febrillis, Fever Blister, Cold Sore)
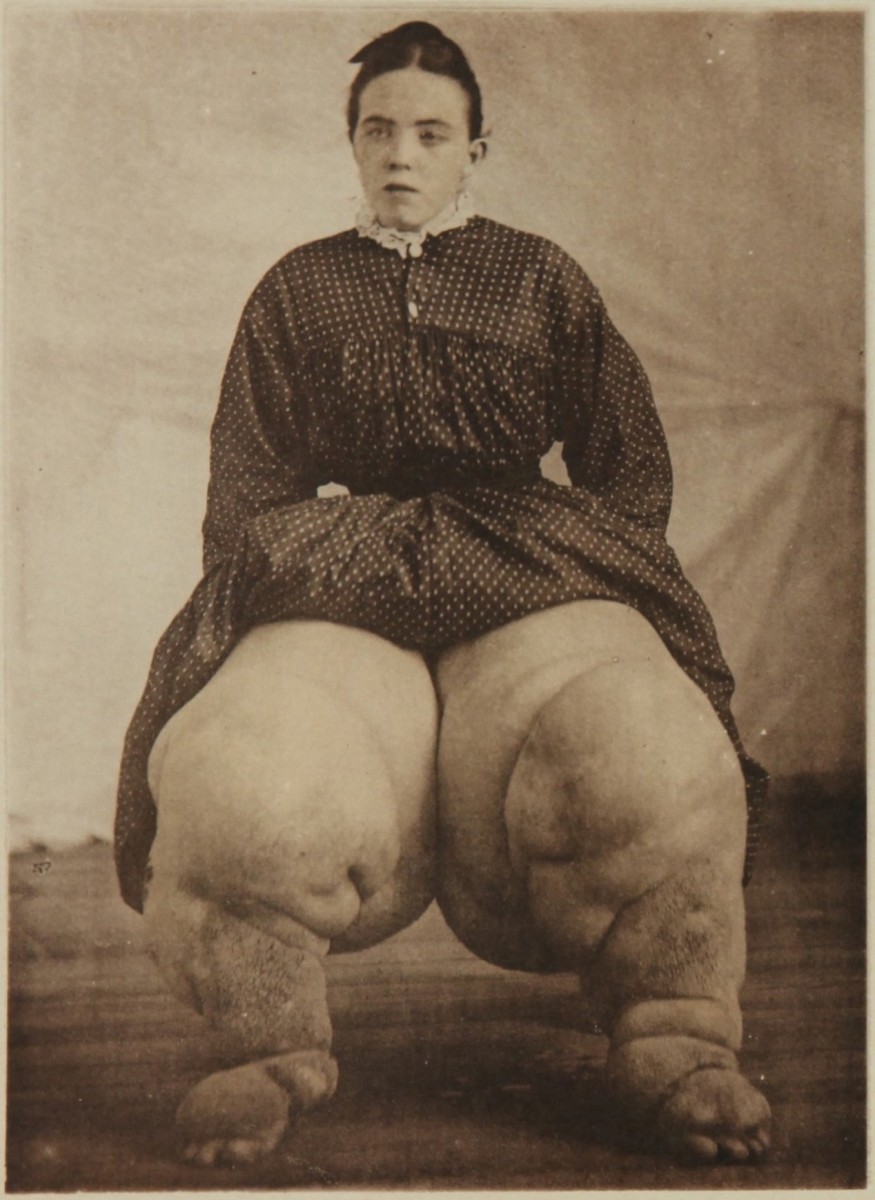
Infection by Herpes simplex virus (HSV) also known as Herpes virus hominis (HVH), produces recurrent crops of vesicles over the mucocutaneous regions. Two types are infective to man. Type I HSV causes herpes labialis and keratitis. It is transmitted non venerally. Type II causes genital lesions and is transmitted by sexual contact. The virus remains in the skin and nerve ganglia in the dormant form to be activated periodically to give rise to recurrent eruptions. Fever, exposure to sunlight physical or emotional stress, malignancy and immunosuppressant drugs lead to exacerbation. Fevers, especially pneumonia, malaria and meningitis are commonly associated with herpes labialis. Herpes simplex is rare in enteric fevers. A crop of vesicles develop following a short period of tingling pain and paraesthesia over the affected region. The vesicles remain for 7 to 10 days after which they start to heal with the formation of crusts. Healing is complete in 21 days. When the crusts fall off, thin scars persist for some time. Common sites of eruption are around the mouth and external nares. Less commonly herpes simplex keratitis, recurrent gingivostomatitis and vulvo vaginitis may occur. Herpes simplex virus can cause mild fever. Serious complications may occur in susceptible persons and in immune-suppressed subjects. These include herpes simplex encephalitis and Kaposi’s varicelliform eruptions (eczema herpeticum). The latter develops in infants and adults with eczema. In such subjects, the eruptions become generalized and this leads to excessive loss of fluid, electrolytes and proteins. Herpes tends to become generalized in subjects who have sustained burns. Generalised herpes simplex occurring in wrestlers is called herpes gladiatorum. Herpes simplex virus pneumonia occurs in immunnocompromised hosts.
Diagnosis: Herpes simplex has to be differentiated from pustular or vesicular rashes and herpes zoster; the latter is nonrecurrent. Herpes simplex virus can be isolated from the vesicle fluid. Serological diagnosis is by demonstrating complements fixing antibodies.
Treatment: Local lesions which are benign may be left alone with simple cleaning and application of gentian violet. Topical iodoxuridine (0.1% hourly as drops or 0.5% ointment) is effective in herpetic keratitis. Antiviral drugs like adenine arabinoside and vidarbine are effective in more serious and extensive infections. Adenine arabinoside is given intravenously in a daily dose of 15 mg/Kg for 10 days.
© 2014 Funom Theophilus Makama