- HubPages»
- Health»
- Women's Health»
- Pregnancy
What To Expect From A Caesarian Birth
WARNING: Read This First!
This article uses my story to inform others of a real-life caesarean birth & recovery. At times I go into graphic detail and talk about things that are gross. But that's the human body for you! You have been warned...
Why Do I Need A Caesarian?
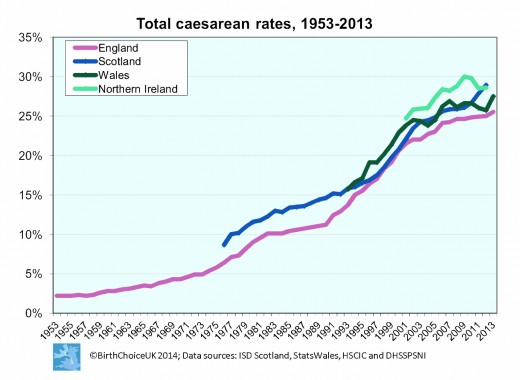
The number of Caesarian births has been steadily increasing, with approximately 25% of UK births being C-sections. Nowadays we have the technology and capacity to monitor the foetus's development to as much detail as if they were already born, and this means that any problems are usually picked up prior to the birth. Many of the things that doctors see as "red flags" would put the pregnancy into the "high-risk" category, but it's important to understand that it's a relative risk. Overall, childbirth of any type is incredibly safe in Europe & the US partly due to the medical assistance available. What we deem as "high-risk" is usually safe for both mother and baby as long as the appropriate medical care is given.
This does mean that more pregnancies are falling into the "high-risk" category, but it also means that many women & children are alive today who otherwise would not be. More pregnancies are able to continue to term, and have a successful outcome, than in previous years, and this means that there are inherently more "high-risk" pregnancies than say, 50 years ago. Those pregnancies would likely have ended in miscarriage or stillbirth, but now that we can pick up problems earlier, more of the at-risk pregnancies can be saved.
We should be careful when reminiscing about The Good Old Days, when caesarian births were rare or unheard-of; those same Good Old Days also had a higher maternal & infant mortality rate. If your doctor decides that a caesarian is necessary, it will be for a good reason. Generally, doctors prefer to avoid caesarian delivery, as it's more resource-intensive, carries a slightly higher risk than a natural birth (statistically speaking), and can have an increased chance of complications and a longer recovery period.
So that sounds rather daunting. It may have come as a shock or disappointment to hear that your birth is not going to go as planned. It might also be a relief - there is no shame in being afraid of childbirth, although it would be better for everyone if there were more honest and open discussions with and between women about what can happen on the day. You may also be worried about your child's health. If they have a condition that is survivable but could affect their development, that is another layer of anxiety to deal with. If you are fortunate, you will be offered appropriate counselling. Not everyone's experience is the same, unfortunately, and sometimes our cash-strapped health service isn't the best it could be. In those cases reaching out to community support groups, charities and internet forums might be the next step in making sense of the future for your child's health & development.
Sometimes there are issues identified prior to the due date that indicate well before time that a caesarian birth will be necessary. These include genetic conditions, growth problems, & multiple pregnancy. But there can be reasons that happen on the day of delivery. I was personally booked in for an elective C-section, but my child decided to come along two weeks early, elevating it to an emergency caesarian when I showed up at 4am in the hospital with my waters broken. Sometimes everything can be on course for a natural delivery, and then something happens that makes an emergency section necessary. Perhaps the baby is breech and cannot be turned, or labour isn't progressing quickly enough and mother and baby are in distress, or there may be an issue picked up with the baby at the last minute. Whatever the reason, if this decision is taken, shit gets real, really fast.
This Video Explains The Procedure - Not Sure About The Guided Imagery Bit, Though!
Not Enough Information
Unfortunately, the amount of information available to expectant parents varies hugely depending on which hospital you attend, whether you use the NHS or go private, and what supplementary services are available in the area that you live. All of the information you might need is out there - somewhere. But what is readily available is a different matter. It's a good idea to look for local parenting groups and charities (such as the NCT) well in advance so that at least you have a contact to go to if you're feeling completely lost. The trouble with relying on information from sources without medical training (and even some of those with it, unfortunately), is that not all of the advice you'll receive will be sound or useful. That's a topic for a whole new article, so I will just say that for now.
My own experience of the NHS was that specialists (I was under the care of three different consultants for various things during my pregnancy, and their support staff were also excellent and knowledgeable) were open, honest, and made sure that I knew exactly what the problems were, and exactly what I could expect. They spoke candidly with me about the less rosy possibilities, and I felt reassured that I was in capable hands.
However, I was also booked in for the same antenatal classes that are available to everyone, and the advice they provided seemed to be tailored for some mythical Earth Goddess who gives birth in a lake of butterfly tears and instantly bonds with her angelic infant. He cries no tears of his own, for Earth Goddess's intuition is such that her mind is one with her child. She nurtures, is natural, and is perfect in every way. What a load of old crap.
It was probably made worse by the idea pushed by the British media at the time, that celebrity mothers were having elective caesarians as they were "too posh to push". I'm not aware of any evidence for this affecting the overall caesarean rate, but there was a determined effort from midwives & health visitors to avoid discussions of such things. Gasp! I'm coming over all faint. Seriously, in my antenatal classes, they discussed all manner of birthing techniques, from doing it on the ward, to water births, to standing on your head probably. They covered in great detail any interventions, like ventouse suction, being induced, and all the different types of pain relief (with some weird anecdote about what hallucinations one of the midwives had experienced from gas & air). But caesarean birth was left right to the end, and there wasn't time to talk about it. In an earlier session, they announced what the percentage of births by caesarean was nationally, and then compared it to the proportion at that hospital. There was a bit of umm-ing and ahh-ing because this hospital had a sky-high C-section rate (over 30%), and they assumed it must be a mistake. It almost certainly was not, because it is a major hospital in a large city, with a specialist centre in reproductive and women's healthcare. The difficult cases (i.e. the ones more likely to need a caesarean) would be more likely to attend this hospital.
I knew, from discussions with doctors, that I would not be giving birth the good, old-fashioned way. There had been numerous interventions throughout my pregnancy, and all the indications were that a natural birth would endanger my life and that of my child. And yet I had no idea what would really happen on the day. Even though I'd been told by doctors that my baby wasn't going to be coming out of the expected place, midwives and nurses were still providing me with information on being induced and "natural" birth ("well, things might change"). The idea that women can't be trusted with information about their own bodies is a regressive and poisonous one. Most women in the UK do give birth naturally. If C-sections really were such an easy option, we'd all be having them. For those who can do it, it's recognised that natural birth is the easiest and safest option. In those cases where it's not possible, caesarians are necessary. It's a medical issue, not a fashion statement, and combatting media nonsense by withholding information, or assuming women are silly, is more harmful than the falsehood put out there in the first place.
Does My Bump Look Big In This?

Elective Caesarian
Elective caesarians are ones that are planned in advance between you and your healthcare team. If all has gone to plan and your baby hasn't turned up of their own accord by the big day, you'll attend the hospital at your allotted date and time, and prepare for surgery. Most elective caesarians are performed with the mother awake, using an epidural (spinal) anaesthetic, although if serious issues are anticipated, or if things suddenly change during the birth, a general anaesthetic may be needed. Although most major surgery is safe and high-quality, if there are more interventions in a birth, the risk starts creeping up. So a general anaesthetic won't be used unless it is absolutely necessary - it would only be a consideration if it would be safer for mother and baby due to whatever medical issue has arisen.
Because the surgery is planned, you will have been told not to eat or drink for at least 8 hours prior to the time of surgery. There are two reasons for this: anaesthesia, and the industrial-strength painkillers that you will receive after surgery, can make you feel queasy. It is going to be a major inconvenience if you start blowing chunks in theatre. And if things take a turn for the worse and you need a general anaesthetic - which means that you would be intubated (it's unlikely, but it could happen), there is a risk of you aspirating food into your lungs (in an emergency, the risk of this happening will be lower than the risk of you dying in the event that surgery doesn't happen, so it's safest for the doctors to take their chances on this not happening and deal with it if it does).
Once everyone is signed in and all the staff are ready to perform the operation (the operating theatre gets busy, more on this below!), you will be shown to a room where you will change into the sexy plastic hat and gown combo. You will then either walk, or be wheeled in a chair, into the anaesthesia room, and you will meet your friendly anaesthetist! One of my biggest fears was that I might be able to feel something during surgery, but my anaesthetist was very reassuring and they also did a test when I was on the operating table just to check the anaesthetic was doing what it needed to (more on this below).
The anaesthetic is then given, via an epidural injection. I was asked to sit on a trolley and lean over a high table. I was then given a local anaesthetic just to numb the skin over my spine, and then they delivered the good stuff through a tube. I then needed to lie down on the trolley, and they wheeled me in to theatre. I was lifted on to the operating table, my gown was raised (a piece of thick tissue was laid over my privates to preserve my modesty, which is very thoughtful, but at this point I was feeling rather woozy from the anaesthetic so probably wouldn't have cared if I was completely naked!), and a screen was put up so that I wouldn't be able to see the surgery happening. I had a friend who asked for no screen, and she told me a delightful tale about intestines, so unless you are completely unsqueamish, I recommend that you keep the screen!
On the operating table I was asked to lie with my arms outstretched, and they were supported on the cruciform operating table. At this point, things started to get a little weird. The top half of my body was shivering uncontrollably, and it was such a strange feeling. I can't remember if I felt cold or not, but I was advised by the obstetrician that this happens because the brain is trying to figure out where the legs have gone (under anaesthesia, the nerves stop sending signals back to the brain, which seems to cause it some distress - funny, that. I think that a similar thing happens in patients with phantom limb syndrome, but in reverse).
Before they start cutting, the surgeon needs to be sure that you really are numb from the waist down! They sprayed some cold stuff on my leg to check if I could feel it or not. At least, that's what she said she did, because I couldn't feel a thing! And the anaesthetist was there on standby, making sure that I was safe and pain-free. Once they know the anaesthetic has worked, they will insert a catheter into your urethra (you'll be seeing more of this later).
And then magic happens behind the screen. You might feel come tugging and wriggling, and hear some slurping noises, all of which is actually completely normal! Then you will hear a tiny cry and you may get to meet your baby straight away or they could be taken into the next room for some tests and/or treatment. It depends on their condition immediately after birth. Some babies require more attention than others, but whatever the healthcare team are doing, it will be in you and your baby's best interests.
The surgeon will be sewing up your wounds while this is going on, so you may not be able to hold your baby immediately. But unless they need to go straight to intensive care, they will be brought over so that you can at least see them, and if you have a partner in the room with you, they will get to hold them. I should also note here that your partner will be donning the obligatory funny hat and gown, and also some attractive blue foot covers. Once you have been sewn up and bandaged, you will be taken to recovery, where the anaesthetic will start to wear off, and you will be given additional painkillers. I was given morphine, and may I just say that that stuff is a-ma-zing! It makes you sort-of forget, and not really care about the pain. If you take this drug, you might find that you can't remember the names of everyday things, or struggle to string a sentence together. It is a very confusing experience, but a pleasant one. Morphine also makes you feel sick and thirsty, so you'll probably cycle between sipping water and throwing it back up again. Lovely.
In recovery, you'll be propped up so that you're leaning against the backrest and pillows at about a 45-degree angle, and you're probably in a better state to hold your baby now. You may be able to breastfeed - it's encouraged, but it doesn't always work out that way. You'll probably be really tired, and you may fall asleep in recovery, or when you get taken on to the ward. Having someone with you in the hospital can be very reassuring and they can help to keep your baby with you if you're not physically stable enough to hold them.
Hello, Mum!

Emergency Caesarian
Things are less certain with an emergency caesarean. No-one has planned for this, so it just has to be made up on the day. You will arrive at the hospital (you might or might not have had time to phone ahead and let them know that you need to come in), and be taken to the maternity ward so that you can be assessed by triage nurses and the obstetrician on the ward. Because things are uncertain, you might have any number of tests ranging from ultrasound scans to a physical examination. It probably won't be the greatest experience ever, but it's necessary, and at this point dignity and squeamishness have to be put to one side. Your body has decided that this is happening, and you are going to have to deal with that.
Whether you were anticipating a natural delivery, or planned caesarean, you will now have been assessed by the nurses, midwives and doctors, and the decision is that you need an emergency section. Similar to the above, you will gown-up and go through to the anaesthetic room. In many cases, an epidural anaesthetic can be used, and you will be awake for the birth. If you are already in labour, and it is safe to allow it to continue, you may not go to surgery until your contractions are very close together. This is because doing so helps to prepare the baby's lungs better for life on the outside.
In some cases, it's necessary to go under for the procedure. The surgeon and anaesthetist will explain to you the reasons for this, and talk you through what will happen as you lose consciousness and wake up in recovery. Your recovery will be different, due to the different type of anaesthetic, and any reasons that made an emergency section necessary. You might be aware of your breathing tube being removed, but you also might not be aware enough to remember that. It can be unpleasant for some people, but it has to stay in until the anaesthetist is happy that your airway is no longer affected by the anaesthetic. When you are brought round, you will be very confused and forgetful, but you will notice that you are in pain. You'll be given something suitably strong (usually morphine via an injection), and you will be monitored in recovery the same as for those who had an elective caesarean. You might not get to meet your child for a few hours more, as they may have been taken to intensive care or a different ward.
Rates of Caesarian Birth in the UK, 1953 - 2013
The Who's-Who Of The Operating Room
There will be at least 10 people, and more if you're having a multiple birth, in the operating theatre with you. It's a busy place! These are (Source: babycentre.co.uk):
- a midwife, to do basic checks on your baby once he’s born
- a consultant obstetrician or registrar, who does the surgery
- the obstetrician's assistant
- an anaesthetist, who gives you the drugs to numb you
- a paediatrician, if you are under general anaesthetic, or if your baby will need special care once he’s born
- a paediatric resuscitation team, in case your baby needs help straight away
- an anaesthetic nurse or operating department assistant
- a scrub nurse, to help the obstetrician with the instruments
- one or two theatre nurses
- medical students or student midwives (with your permission)
I Hope They Have A Theatre Big Enough For All Those People!

Post-Recovery
After the anaesthetist and surgeon are happy that you're out of danger, you will be transferred to the ward. If you've had a caesarean birth, you're more likely to get a single room, but it's not guaranteed. You're going to feel pretty crappy now, and getting some well-earned rest is necessary. Your birth partner needs to step in here and look after baby, as you won't be able to get up and move around immediately after the surgery. If you don't have anyone to assist, nurses will generally be able to help out, but in a busy NHS hospital, I found that they weren't all sympathetic and I did feel a bit over-stretched and frequently exhausted.
Depending on what time you arrive on the ward, you'll probably be given a light meal when you're able to eat again. I have fond memories of lying down, feeling a bit sorry for myself and eating toast because that was literally all I was capable of doing. If you're in an NHS hospital, they probably won't help you out too much from this point, partly as they want you to be moving about and getting used to looking after a baby while recovering from the birth, and partly because resources are limited and they have to divert attention to the most needy. Even though you feel terrible, are in pain and nervous about your stitches, you might not be a priority. It sucks, but if they are waiting on you hand and foot it probably means you've got bigger worries. Again, having someone with you in hospital is a huge help. In the first few days after the birth, the ward sister is likely to be more relaxed about visiting hours. Having a new baby is doubly tough if you're recovering from surgery. But after that, if you do need to stay longer, they tend to be strict about visiting hours, and this will mean you taking on more responsibilities. It's also a good reason to hope that you will be discharged as quickly as possible.
Remember that catheter I mentioned earlier? For the first day after surgery, this will stay in place, and you'll be carrying a bag of wee around with you wherever you go (nice). I needed to use a wheelchair for the first 24 hours, so I had this fixed to the side of the chair and I wore a blanket to cover the plumbing.

Dr. Jen Gunter's Blog
There's a lot of questionable info and advice out there. If you want the bare facts, read Dr. Jen Gunter's blog for evidence-based info on birth, and other women's healthcare issues.
Paper Pants
After childbirth, by whatever means, you get to wear the World's Ugliest Disposable Knickers! They come in broad Small / Medium / Large sizes, and you have to wear a pad in them that is about half the thickness of a house brick. This truly is a moment of glamour and style. The nurses don't want you to use sanitary towels for this purpose - this is because the giant brick pads, while a throwback to less advanced days, make it easier to check on what's coming out (nice). When you dispose of the pads, they are checked for anything unusual. All sorts of gunk is going to be coming out of there for the next 4 to 6 weeks, but if anything unexpected appears, it will usually be noticed soon after delivery. The hospital say to continue using these giant monstrosities once you go home, in case you get readmitted, but I was sick to death of feeling like I was wearing a nappy, so I reverted to my trusty Always Ultra.
The Caesarian Shuffle
On a maternity ward, it's easy to spot those who have had a caesarean birth. They're the ones taking tiny shuffling steps like elderly people! You are encouraged to start moving about as soon as you can, to assist in your healing and rehabilitation. But you're not going to be running marathons in the early days. Standing up and walking so soon after surgery is safe, but it doesn't feel like it. I was terrified; I thought my insides might drop out if I stood up, and it certainly felt like it. Taking a step was extremely tender, and felt like I was tearing my stomach muscles with every step. That's why those women do the caesarean shuffle! It doesn't last forever, you should be able to walk quite normally after a week, and back to your former stride after a fortnight. You'll still get the odd twinge when you move in certain ways, or stretch a bit too far - this could happen any time up to a few months after surgery. As long as you don't do anything too ridiculous (skydiving is off the cards for now), you're unlikely to cause yourself serious harm. You should avoid driving, heavy lifting (except for baby, unfortunately), or strenuous exercise for at least 6 weeks after the birth as a minimum.
Your First Poo
No, not baby's first poo, your first poo! You may think that you have escaped the indignity of soiling yourself that can happen with a natural delivery. Well, do I have a surprise for you! The anaesthetic slows down the body parts that it affects. And your gut & bladder are in the same region as your womb, so there are going to be some unpleasant effects.
Your body's waste disposal system is going to have something of a backlog. Your urine will have been dealt with via the catheter discussed above, and then once that's removed, you'll be expected to use the toilet by yourself. Everything will feel quite fragile and not-quite-right, and you may struggle to go, or you might be slightly incontinent (see, you get the same problems as an ordinary birth, but a lot of other stuff on top!). But when you need to do number-twos, it's worse...
In my case, I actually managed a poo before I urinated independently. No, I'm not superwoman - it's just that my guts did some work behind the scenes and my body wasn't properly recovered or ready for it... The day after my surgery the nurses got me to take a shower. Not all of the sensation had returned, but I could stand, just about. So I had as brief a wash as I could (I just wanted to sit back down, mostly), and got myself dry. With a white towel. That had sticky black poo on it. I felt so dirty - I'd pooed in the shower without realising. It was a worry for me - I didn't want to be doubly incontinent (it can happen to anyone who gives birth, but is thankfully not that common). After getting cleaned up, properly this time, I went back to bed for a rest. I felt quite embarrassed, but given all the prodding and examining I'd been through, it was just one more thing to add to the pile. My next bowel movement was more typical of those who've just had major abdominal surgery: painful and scary.
I felt a bit constipated (that's the anaesthetic hanging around in your system), and it took a lot of effort to do my business. Needing to strain made my stitches hurt, and so I was caught in a game of trying, but not too hard. It was horrible, and the fear of disembowelment was greater than for when I took my first steps (again, this is very unlikely to actually happen!). But when it's done, it's done, and apparently the fact that you have had a successful poo post-surgery is a good sign.
Finally, You Get To Go Home!

Going Home
You'll have to stay in the hospital for at least three days, usually. But before you leave, there are some things that need to happen:
- Your internal stitches will dissolve, but your external ones need to be removed. The wound will be checked to ensure that it's healing properly. If it needs more time, the stitches can be removed at home by a midwife.
- Your womb will be examined to ensure it's in the right place and is returning to its normal shape & size. This involves a doctor prodding and squeezing your lower abdomen.
- You will speak with the midwife about feeding. They like to encourage breastfeeding, and if you choose to, they should make sure that the baby is able to latch on and feed. If you're bottle-feeding, they will teach you and your partner how to make up a formula feed.
- Very important this one: contraception. It's not great for your physical or mental health to become pregnant immediately after giving birth. So the midwife will discuss contraception with you, and help you to arrange an appointment with your GP to discuss this.
- Your baby will be weighed and given a final healthcare screen, and then...
You're On Your Own!
You need to take baby home and figure it out together. It's a unnerving experience, but you will be ok.
Try To Take It Easy
That's easy for me to say, not having to care for a screaming baby while recovering from surgery. But you are still recovering, and any help you can get is going to make a huge difference. If you have a partner, make sure they know that you need extra help (they should be sharing the care anyway!). If not, find excuses to invite friends and relatives over, and cajole them into helping out - try not to feel guilty, this is a stressful and busy time and they should notice that! After 6 weeks out of hospital, you will need to go for a postnatal check-up at your GP's surgery. After that, life begins to return to normal (except for the screaming baby bit). You will be able to begin gentle exercise again, you can have sex again (if you have the energy), and you should feel less fragile. But you will still feel the after-effects for months and years afterwards. I still get twinges in my stomach if I do certain ab-based exercises, and I had my child 11 years ago!
Preparing To Take Baby Home
© 2017 Katy Preen