Mother Became a Child
It happens. Adults get older and behave like they are children. This is no surprise to many of us because we expect it. When it actually happens, however, that shift of power is a heavy burden to bear. There are relationship changes, financial adjustments, and social adjustments. In this article, I use the personal experiences of my parent who fell into the grasps of dementia. No names are used other than my own. The experience can be ongoing and emotionally painful, though my parent passed away within three weeks of her official diagnosis.
Vascular Dementia
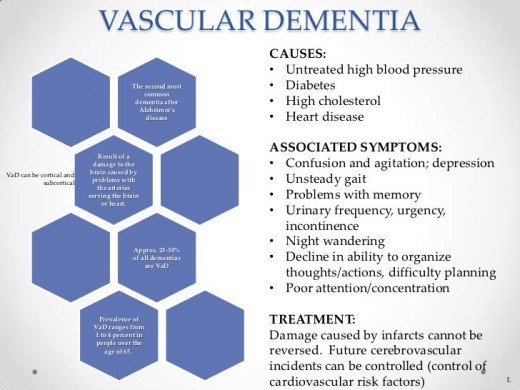
Dementia is a general term used to describe any condition that impairs memory, language, reasoning, attention, perception, or problem-solving. It affects older people, mostly over the age of 60 and is the result of head trauma.
Vascular Dementia is the disease of blood vessels in the brain, generally, resulting in confusion and eventually memory loss. It generally follows severe or multiple strokes. Its effects on the sufferer and family vary depending on the level of brain damage. Find out more at the National Aphasia Association.
Mother's attending physician in the hospital found evidence of oxygen-depleted brain tissue due to a severe stroke she suffered years ago while I was a youth. He suggested the diagnosis of Vascular Dementia as an explanation of Mother's odd behavior with advice to follow-up with the Primary Care Physician for a visit to the Alzheimer's Center in our local area. This was the beginning of the end of Mother's freedom.
To help mom now, we had to be a team. Now, more than ever, we had to put aside any personal bias and work together to support a family member who could not help herself.
Relationship Changes: Husband & Wife
Mother was always a vibrant and independent woman. She survived drug abuse, abusive marriages, and poverty. When my wife suspected that her new enemy was dementia four years prior to the diagnosis, I flatly dismissed the possibility. I assumed my wife and mother had a complicated "love-hate" relationship and this accusation from my wife's represented the latest attempt to explain the strain.
My wife and I strained communication about Mom to put it lightly. My mother's behavior changed to such a degree that my wife became alarmed. Mom's standard behavioral schema no longer existed. Having lived with us for seven years at the beginning of our marriage, I adamantly opposed my mother living with us because of past troubles. My wife encouraged me to step in and see if there were problems with Mom. Each time I asked her if she was fine, of course, Mom said she was fine.
If there existed some evidence to support investigating "fine behavior" I did not see it. When Mom obtained a new boyfriend, my wife balked. I told Mom to marry the man.
When Mother stopped visiting like she normally did, my wife pressed harder that something was amiss. I dismissed it. My wife and I had enough on our plate without her bringing up Mom having issues.
My wife was fearful of my dismissal of Mom's changes. I refused to see out of fear that there were emotional or mental changes. I feared she would need to live with us. My wife and mother's relationship suffered due to these emotional changes in Mom. I loved Mother, but my wife could not deal with her quirkiness. I had no intention of putting my marriage on the line.
I refused to express my feelings with my wife fearing she would express a thought that would involve abandoning my mother, a gross mischaracterization of my wife. Mischaracterizing my wife was something I did often. It was easier to invent flawed personality traits for my wife than speak to her and discover the truth.
Four years of denial changed when my wife's fears proved to be true about Mom. The fear shattered and I spoke to my wife. To help Mother, we had to be a team[ to put aside any personal bias and work together to support a family member who could not help herself.
Knowing dementia was the cause of the friction with Mom softened our hearts and changed our understanding of how to help her.
It helped us learn to trust each other.
Be prepared to lovingly, yet assertively say no when it is necessary.
Relationship Changes: Parent & Child
Independent people do not take kindly to others telling them what to do. Imagine a child telling the parent when it was time to eat, take medicine, or go to bed.
My wife accused me of being a momma's boy. After years of denying it, I must admit it. When adults suffer from any form of dementia, the severity of it determines if that person needs constant support. Mom needed constant support and help to the point that she could never be left alone.
When Mother spoke, I felt the need to obey, even as an adult. The things that came out of her mouth made no sense. As hard as it was, I had to ignore Mom's commands! When I spoke to her, I did so with the understanding that she might not remember what I said or understand it.
Because my wife and I were her caregivers, we had to create a routine and plan of action to help to accommodate Mother's illness that maintained her integrity in our eyes and the eyes of others.
Instead of her caring for me, I had to care for her.
The fallacy that the caregiver is the parent needs to be stressed. Never will a child be the parent of his or her parents. The relationship is the only thing that changes. The parent must receive the same level of respect and honor as before. A caregiver must make sure to provide only the level of care necessary to help his or her charge to help, in our case, herself. Doing too much, even too little, may cause a quicker mental decline.
We do not do everything for our children, or they will not learn. If we did everything for Mother, she would lose the little bit of freedom to act she had left. The hardest thing for me to do was tell Mother, "No." Being prepared to lovingly, yet assertively say "No" when necessary did not make us Mother's parents, but respectful guardians.
As caregivers, we must be open with those in our care to the extent they can understand about their finances and other things.
Financial Adjustments
Mother had bills. She had income. Our predicament was different because she was in a relationship with a man before we brought her home who used her declining mental capacity to get ahead financially. Once Mom lived with us, we could not speak to her about the bills she had because she did not understand the questions we asked. She had not paid her bills for months. The boyfriend had taken over that aspect of her life.
We worked to cancel her cards and get a Durable Power of Attorney so that we could manage her funds and pay off her debts. We also had to consider her health needs in that Durable Power of Attorney. We decided to get a separate Medical Power of Attorney so that we could make her doctor's appointments and make decisions on her behalf to keep her healthy and alive. The hardest thing about it was to wait until Mother had a moment of clarity so that she could sign the legal documents to give us that power. The following link is one way to find out information about a power of attorney. HERE
Caring for another dependent changed the way we did our budget because we had to include her income with ours. We also had to make sure that she had access to the things she wanted to purchase within reason so that she could keep a measure of control. This is a sacred trust. Many elderly people are taken advantage of by shameful people because the elderly tend to trust family and even complete strangers due to loneliness. Caregivers must be open with those in their care to the extent the recipient can understand their finances and other things.
Social Adjustments: Mom's Decline
Mother had a boyfriend. This was a shock to our little family. As an active church-going lady, Mother devoted her life to God. About four years prior to living with us, she found a man when she moved into her new apartment a few miles from my family. She spoke often of not wanting to be lonely. We had her over as often as we could after she stopped living with us. It was not enough for her. She wanted constant companionship.
She brought her new suitor and his grandson around. At first, we all liked the idea. The man was 20 years her junior, but Mom always dated younger men, including my dad. My oldest kid immediately disliked him. We thought it was due to the reality of seeing his grandmother dating. After a few more meetings with the man, my wife disliked him.
We wanted Mom to date and have a social life. Her choices in friends did not give us confidence that she made the right choices. They fought and profaned each other. This type of behavior was not Mom-behavior! She ended the relationship only to return to him again. He proposed to her many times, but she always refused marriage.
As her mind declined, she stopped visiting so often. When she refused to come to my home for her traditional Mother's Day dinner, I died inside. This was never the case. She was above 70 and never missed the dinner I made for her. We fought with the boyfriend over her for weeks before he was jailed over unrelated concerns. A neighbor of hers called us to get her.
Social Adjustments: Living with Mom
Never did we think it would be so hard to deal with a person until we brought Mom home. She did not want to come with us. Her boyfriend told her that he was the only person who cared about her. She believed him. After days of deprogramming her, we started the long process of integrating her into our daily lives.
At our home, we had to tag-team with each other about who would go away from the home. We were able to get her to go to church with us, but being in public was usually a big overwhelming deal for her. We did not go on dates because we couldn't leave our kids with her. There are resources out there that help caregivers. There are elderly daycares and homes. We, however, didn't want to put her in an old folks' home to live or even to visit.
I was in a nursing home for 1 month due to surgery. It was not a bad place, but emotionally, it was hell. The people there do not treat the patients with enough dignity (Notice I say enough dignity here). They were not mean. They treated me like a child. I was young and mentally stable and aware. Who would know if all the employees at a facility treated those who do not have the mental capacity appropriately?
Mother's doctor told us that being around younger kids made it more bearable for her. The kids loved their grandmother and gave her the love and acceptance that she needed from the youngest child to the adult child. It is a testament to their character and our rearing. Family support is a key ingredient in helping dementia patients.

Social Adjustments: Psychological Aspect
She sat in the living room looking at the door for an hour, or so, chatting out loud about needing to get her car. I tried reasoning with her that we have her vehicle already and there was no need for her to worry about leaving to do so.
It did not appease her. I could feel the anger dripping off of her as I tried to say no without actually saying it. The temperature outside was above 100 degrees when I heard her open the door and head out. I chased her down the driveway and stopped her from leaving. She fell to the ground and started screaming bloody murder!
Angry, shocked, and scared, I tried to pick her up off of the hot ground before she hurt herself. In my head, I could only think "Why is she acting this way? Doesn't she know that I am trying to help her?"
She refused to go back into the house and I could not touch her without her going into a panic and fighting. We had to call the non-emergency line for help. She went to the hospital.
Here was the first mistake I made when I noticed she was in that predicament. I did not redirect her attention. She is not a child; though, like children, redirection works best to avoid a temper tantrum. When providing care for parents, we have to lovingly guide their thoughts toward something more constructive.
The second mistake I made was to stop her by force once she started walking away. Avoid using force. I could have simply followed her and asked her where we were going. That was a viable solution in my case because of the neighborhood in which we lived. When I blocked her way it caused her to panic verifying her fear that I was trying to take away her freedom.
Mother cried all night because she remembered the entire experience along with the terrible things she said. Again, redirection is the best answer. It could have worked had I had the training to think of it. If there is no other option, explaining to her why she cannot do something rather than preventing her from doing it with no explanation is the key to avoid a traumatic breakdown. Instead of blocking her way, I could have stood in front of her with a smile agreeing to take her to her car. We could have driven around the block. The only time force is necessary is when there is a danger such as falling off a bridge or handling a sharp object.
The third mistake I made was to vent my feelings around her regarding her condition. Never vent about your charge in her presence! Mother revealed later that she heard us speaking about her in another room about her being senile. It hurt her feelings, which is what triggered her need to leave that day.
Training about how to deal with caring for loved ones with mental concerns and support groups provide a way to best provide the proper environment to support the mental health of all parties involved.
Having dementia does not mean the person inflicted will forget her episode, as we called it. It is not a time to vent frustration toward the parent or anyone else. It will happen, however. It can be avoided with training and practice. There is a proper time to express frustration, but it should always be directed toward the situation and NEVER the person.
Four Things to Remember with Your Charges:
-
Redirection works on Adults and Children.
-
Never use physical force over non-life-threatening things.
-
Never vent frustrations in front of the person.
-
Training is the key to success.
I love Mom, as I am sure many of you love those who are in your charges. The willingness to take care of our charges is only limited by our capacity to do so in a loving and respectful manner. The moment intimidation and unkind words become an option on our part is the moment we need to think of a different living arrangement.
Seek support from family and community organizations to help keep everyone sane and safe. We have our church and family to help us when times get hard. Reaching out can be hard and embarrassing. It is worth the trouble to admit we need help than to hurt a loved one.
Mom died on July 11, 2018, almost two weeks after this article was published.
Reaching out can be hard and embarrassing. It is worth the trouble to admit we need help than to hurt a loved one.
For Help With Love Ones With Dementia
- Caregiver Health | Alzheimer's Association
Caregiver health resources – caring for someone with Alzheimer's or another dementia can be overwhelming. Get help taking care of your own well-being. - Caregiver’s Guide to Understanding Dementia Behaviors | Family Caregiver Alliance
This content is accurate and true to the best of the author’s knowledge and is not meant to substitute for formal and individualized advice from a qualified professional.
© 2018 Rodric Anthony Johnson