When the Battle Between the Baby and HIV Begins

Our body has the dynamic functions of protecting ourselves against diseases. It is “knitted” and delicately designed to guard us against the attack and assault of the unseen opponent. What if one day this wonderful defense mechanism deteriorates? What if it happens to your precious newborn baby? What if a newly-born child gets infected with HIV? What a mother should know?
Main Agenda
Human Immunodeficiency Virus (HIV) is an intelligent viral agent that causes Acquired Immunodeficiency Syndrome (AIDS)—a disease characterized by a depleted immune response towards infection and unguarded to the attack of the opportunistic infections. HIV is a kind of very shrewd virus that deceptively ravages our very own natural immune defender and turning them into an HIV factory.

The Mother-to-Child-Passage of HIV
- During childbirth.
The virus can be transmitted to baby through breaks and ruptures in the membrane, which commonly happens in the moment of giving birth. Infected mother’s birth canal is filled with fluids and secretions rich in HIV and passing on this canal would yield a tremendous risk of stress, breakages and tears in the baby’s mucus membrane. HIV infected pregnant women are advised to have caesarean section than preferring normal delivery.

- When the baby is still in the womb or during pregnancy
Usually placenta gives a total protection of fetus from any invading pathogens. In some instances, when the mother contracts other in-uterine infections, or malnutrition giving lowered immune defenses, the capability of the placenta to shield the fetus from pathogens like HIV can be broken down.
- Through breastfeeding milk
Virus transmission can occur in breastfeeding because of the presence of HIV in breast milk of infected mothers. Many studies have shown that there is a higher chance of perinatal transmission (which is previously called Mother to Child Transmission or MTCT) of the virus during acute HIV infection rather than during chronic HIV infection. This is because of the rapid viral load increase and subsequent decrease in CD4 count during acute HIV infection. The higher the viral load in blood will result to higher viral load in breast milk and the higher the chance of transmitting HIV.

Infants Develop Faster Progression to AIDS than in Adults
According to Encarta Encyclopedia, HIV infection aggressively develops into AIDS in babies than in recently infected adults; this is because the immune system of the baby is on the stage of development. In an adult—with a well-developed immune system—the body can still respond to virus stimulation; reduce and delay the progression; but it cannot eliminate the virus.
The still-structuring and only just-developing immune system of the baby is gradually shut down by this devious virus in their early days. More studies have shown that HIV infected newborn dies before they reach the age of 2.Most of the opportunistic infections commonly acquired by the adults are also acquired by the babies, except that they are more susceptible and prone to more repeated viral, bacterial, and fungal infections.
One of the devastating facts about HIV is that there is a symptom or disease common in HIV- infected baby but not in adult. Because of the aggressiveness of the virus in babies, the virus massively and without enough restriction attack the brain impeding their intellectual and reasoning capability—affecting their growth and overall body functions—leading to general disability and death.
Most Common Primary Opportunistic Infections Occur in Babies
Pneumocystis pneumonia
| It is a kind of pneumonia characterized by having lower oxygen consumption and delivery, caused by the blockage of the fungus—resulting to dry cough and fever.
|
|---|---|
Meningitis
| A bacterial infection in the brain that provides opportunity to invade the general body system functions, and produces devastating infections.
|
Tuberculosis
| It is a bacterial infection which attributes to the thin and “skeleton-like” physique of an infected person in addition to the symptoms of cough, fever, and anemia.
|
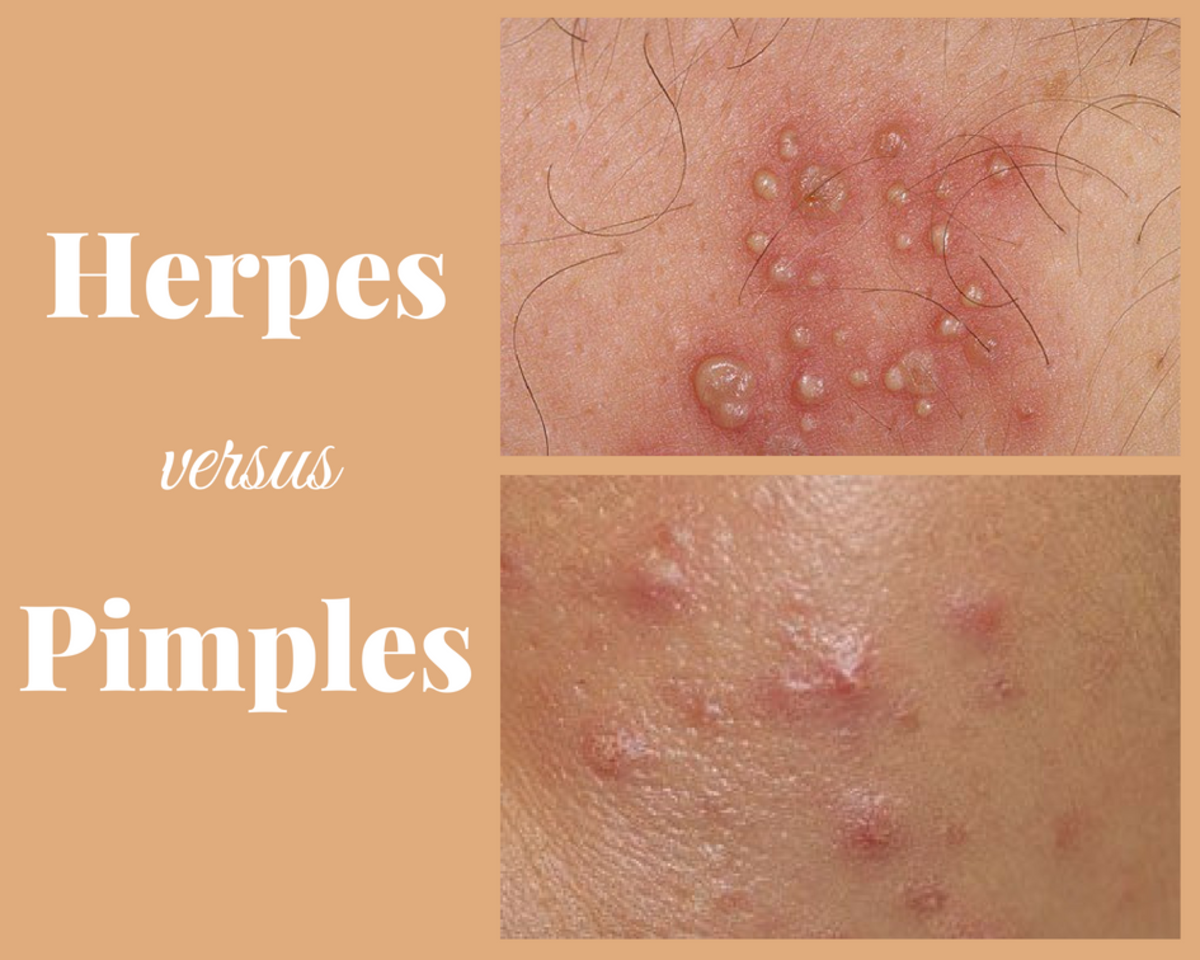
Herpes
| Formation of itching and inflamed skin blisters, and in severe cases, can cause blindness and cancer like Kaposi’s sarcoma
|
People living with HIV (PLWH) managed to beat the effects of the virus through Highly Active Antiretroviral Therapy (HAART) by strengthening their immune system, and reducing the amount of virus.
Zidovudine is one kind of reverse transcriptase inhibitors. The general effect of this type of ARV drugs is to inhibit the replication and reproduction process of HIV by inhibiting the reverse transcription of HIV RNA to HIV DNA.
Most ARV drugs taken by pregnant women cross the placenta to give the baby a pre-exposure prophylaxis
Chance of Transmission
The possible risk of HIV transmission from mother to baby is not always 100%. Most researches revealed that many babies are still negative or did not develop into HIV infection after birth.
According to aids.gov, there is 25% chance of passing the virus to newborn (or 1 possible HIV mother-to-child-transmission out of 4 childbirths) for those HIV naive-mothers who do not receive HIV treatment during pregnancy, labor and delivery.
In contrast, MTCT falls down to 2% (or 2 chances of MTCT out of 100 childbirths) for those:
- Mothers who receive special antepartum, intrapartum, and postpartum care by having standard combination of antiretroviral (ARV) regimen.
- Mothers who undergo scheduled and pre-labor, caesarian section delivery
- Mothers who do not breastfeed
- Infants who receive 6 weeks of zidovudine prophylaxis (this is generally recommended for those infants borne by HIV-infected mothers to reduce MTCT)
What a Mother Should Know and Decide
Here are some of the general information regarding the recommendation for prevention of perinatal transmission. Detailed and updated information is available on this site.
1. Mothers who receive standard combination of Antiretroviral Therapy (ART) before, during and after childbirth with suppressed viral load and high adherence to antiretroviral (ARV) drugs.
- Infant should receive the standard 6 weeks of zidovudine chemoprophylaxis regimen within 6-12 hours of delivery.
- A recent recommendation that a 4 weeks of zidovudine chemoprophylaxis regimen is being considered to minimize the toxic effect of the drug—which is anemia.
The Importance of Antiretroviral (ARV) Drugs
2. Mothers who receive standard Antiretroviral Therapy (ART) before, during and after childbirth, but have detectable HIV load near delivery
- Infant should receive the standard 6-week-zidovudine chemoprophylaxis regimen.
- Mother is recommended to undergo scheduled and pre-labor, caesarean section delivery (at 38 weeks of gestation period) rather than vaginal delivery to reduce perinatal virus transmission due to higher viral load.
- Mother is recommended to undergo ARV drug resistance testing
- Mother must be counseled about the significance of adherence to ARV drug regimen.
- Caesarean section delivery is recommended if the viral load of the expecting mother exceeds 1000copies/mL
The combination of two ARV drugs is said to be more efficacious than using Zidovudine monotherapy in accordance to the condition stated.
3. Mothers who receive antiretroviral drugs during childbirth or HIV intrapartum care only.
- Soon after delivery, infant should receive 6-week-zidovudine chemoprophylaxis regimen and 3 doses of nevirapine in: first dose (0-48 hours after birth); second dose (48 hours after first dose); third dose (96 hours after second dose).
- Mothers are recommended to be treated during labor with intravenous zidovudine regimen if the viral load exceeds 1000 copies/ml or with unknown HIV RNA; but it is not required if viral load is equal or below 1000 copies/ml with consistent and strict compliance to standard combination ARV drugs.
- Prophylaxis should be given immediately after birth. If the treatment is given at 2 days old, prophylaxis is said to be not effective anymore in prohibiting virus transmission. At 14-day-old, HIV is already established in the infant's body.
- A surgical technique of a "bloodless caesarean section" is very helpful to reduce from minimum to zero exposure of baby to maternal blood and body fluids— thereby depleting the chance of perinatal transmission.
Remember, it's Avoidance!


4. Untreated Mother before and during birth
- Soon after delivery, infant should receive 6-week-zidovudine chemoprophylaxis regimen and 3 doses of nevirapine in: first dose (0-48 hours after birth); second dose (48 hours after first dose); third dose (96 hours after second dose).
- Mothers are recommended to deliver baby through caesarian section if plasma HIV RNA exceeds 1000copies/mL
As part of the intrapartum care, the general recommendation for the avoidance of:
- artificial breaking of the fluid-filled bag called the amniotic sac to speed up labor
- use of fetal scalp electrode (Fetal scalp electrode is used to monitor fetal heart rate and rhythm. An electrode and spiral or wire are inserted inside the vagina and is attached to the fetal scalp. It is recommended not to use fetal scalp electrode during childbirth of HIV infected mother due to the possibility of bruising the fetal scalp and can produce infection.)
- use of forcep;
- episiotomy or the surgical incision from the vulva towards anus.
Caution: A positive HIV antibody test done on an infant can indicate maternal HIV antibodies that passed thru placenta and cannot be used to confirm infant's HIV infection. A special test like Nucleic Amplification Test (NAT) is used to diagnose HIV infection in infants below 18 months old. If infant's NAT is positive, ARV prophylaxis should be stopped and the infant should receive the necessary standard antiretroviral therapy based on Pediatric Antiretroviral Guidelines
5. Mothers who don't have HIV screening or confirmatory test
- Rapid HIV testing is recommended for the mother during labor and for infant soon after birth.
- If rapid HIV testing is reactive (positive), infant's ARV prophylaxis should be initiated as soon as possible even without waiting for the confirmatory or supplemental result. If the supplemental test is negative, the ARV prophylaxis should be stopped.
The Significance of Adherence to ARV Drugs
6. Mothers who are ARV drug resistant
- The actual and defined drug formulation and the necessary optimal prophylaxis given to infant delivered by an ARV drug resistant mother are still unknown and not yet established. It is recommended for the mother to consult with an HIV specialist in pediatric care before childbirth.
- Infants are recommended to undergo ARV drug resistance testing before the start of standard cART (combination antiretroviral therapy).
- Multiple (ARV) drug resistance can be passed to infants through perinatal transmission, though there are some studies suggested that multiple resistant virus has lesser viral replication and transmission capacity.
- Screening for Hepatitis B and C is recommended for all HIV-positive pregnant women due to the possibility of co-infection with HIV. The determination of co-infection is necessary before the start of treatment; mode and type of treatment to be used; or the risk of treatment cessation. Consultation must be made with the infectious disease specialist.

White ribbon is a universal symbol for awareness of: (1) elimination of violence against women; (2) and safe motherhood. In the picture above, white ribbon represents baby's protection from HIV infection.
For HIV-Infected Mother
Making the preliminary decision to stand up for the betterment of your baby resides in you. The battle of your baby against HIV primarily commences with your own battle against the virus. The HIV infection needs not to be feared of, but instead, to gain strength to fight back. Fighting back requires acquiring knowledge and information about your enemy—HIV—that can help you protect yourself from the consequences of the action and mechanism of HIV; indulging in a communities and organizations that are willing to help and support; knowing the “in-depth” significance of total adherence to antiretroviral regimens; and intentionally researching how the anti-retroviral drugs work and how drugs resistance occurs. You may be infected now with the devious virus, but there is a greater chance for your baby to be excluded from it. If in some circumstances that HIV infection takes its course in both of you, nothing and no one can stop your will power to live for God and for your baby. A better and healthy life for your babies is waiting ahead, because you decide to stand up for him/her now.