Why Am I so Fat? a Biological Perspective
The mainstream belief in America is that people become fat by simply overeating compared to their physical activity. This is an oversimplification. Many overweight people eat far less than their thin friends. In this article, we will examine the biological factors that contribute to weight gain:
- Heredity
- Body Chemistry

Heredity
Twin and adoption studies conclude that our genes contribute 50% to the likelihood that we will be overweight or obese. Our heredity affects a variety of factors that contribute to our weight, including our basal metabolic rate (BMR). See: Why am I so Fat? Examining the Set-point Hypothesis.
In addition, researchers find that genetics account for 2/3 of our Body Mass Index (BMI).
However, when we inherit the obesity gene from both mother and father, our chance of becoming morbidly obese increases greatly. People with two obesity genes, when eating extra calories, deposit those calories as fat, versus the average person whose body uses more of those calories to develop muscle. But, heredity alone does not destine whether or not we’ll be fat.
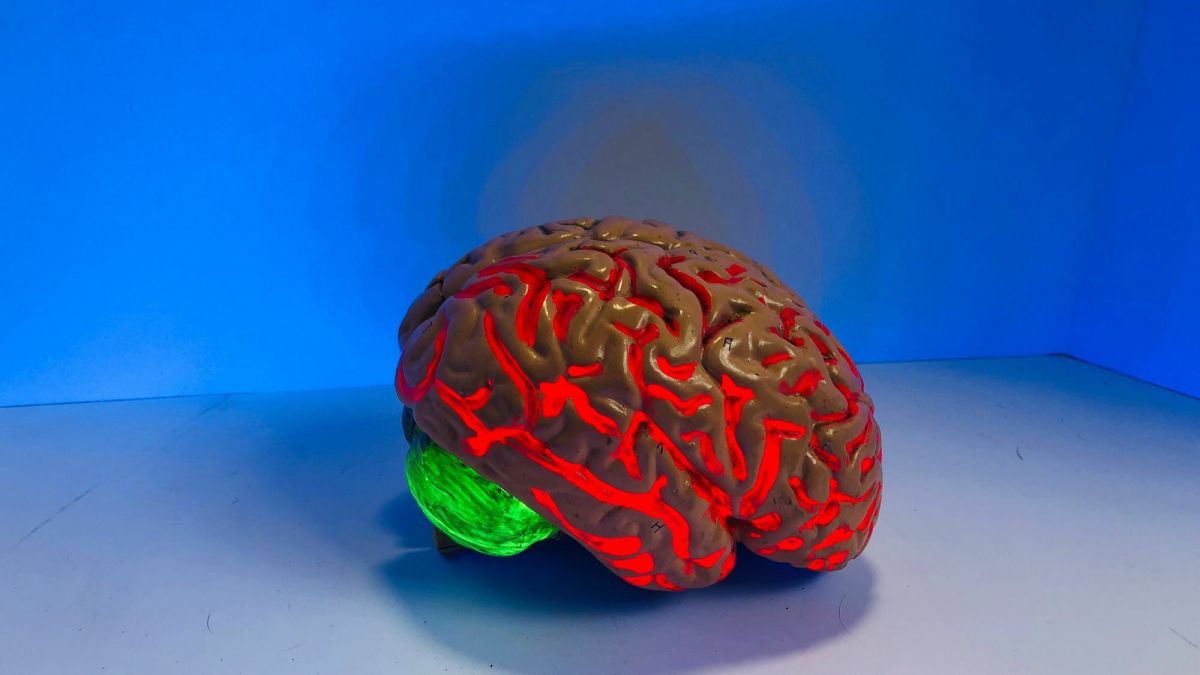
Body Chemistry
At a cellular level, nearly all of the energy our body derives from food is eventually converted to heat. Energy output is:
- immediately lost as heat (60%)
- used to do cellular work
- stored as fat or glycogen
When our energy intake and output are balanced, we maintain our body weight. So simple, right? Then why is it that 2 out of 3 U.S. adults are overweight, with 1 out of 3 being obese?
One reason is that obese people are more fuel efficient and better fat storers. While anyone ingesting 100 extra calories of fat, will, at rest, burn only 3 calories and store the rest, fat cells of overweight people:
- Sprout more alpha receptors, which favor fat accumulation.
- Send different molecular messages than fat cells of thin people. They spew out inflammatory cytokines that can promote insulin resistance, and they release less adiponectin, a hormone that improves the action of insulin in glucose uptake and storage.
- Have super efficient lipoprotein lipases, which unload fat from the blood (usually to fat cells).
Although our satiety chemicals should prevent massive fat deposits, this doesn’t prove to be the case in obese people. Scientists think that it may be that excess weight promotes insulin and leptin resistance.
In addition, our body chemistry can ‘tip the scales’ against us because our body’s weight controlling system appears to be more adept at protecting us against weight loss than weight gain (due probably to early ancestral influences). Our body chemistry, including especially the operation of several hormones, may make the difference in whether we’re able to pass by McDonald’s or not.
Current theories of how eating and hunger are regulated focus primarily on the following factors:
- Neural signals from the digestive tract
- Bloodborne signals related to energy stores
- Hormones

Neural Signals from the Digestive Tract
Vagal nerve signals are those that carry on a two-way conversation between our gut and our brain. For instance, research shows that eating protein produces 30-40% greater and longer appetite–decreasing signals than when we eat sugars.
Bloodbourne Signals Related to Energy Stores
Levels of glucose, amino acids, and fatty acids send signals to the brain that influence appetite and energy production.
Glucose
When we eat, rising blood glucose levels eventually depress our appetite. When we eat sugary foods, our brain signals the body to release dopamine as part of our pleasure system. This could account for the times we instinctively reach for ‘comfort food’ when we feel stressed or depressed.
Amino Acids
Elevated blood levels of amino acids (found in proteins) decrease our desire to eat, although scientists are not currently sure how this works.
Fatty Acids
The larger the amount of fatty acids found in our blood, the more our desire to eat is inhibited. Could this be a factor in the very low level of success in fat-free diets?
Hormones
Insulin, and especially Cholecystokinin, are released when we eat, and they block the appetite-inducing affect of NPY (neuropeptide Y). NPY is the most potent appetite stimulant known. By blocking its release, leptin blocks appetite-enhancing orexins disbursed from our hypothalamus.
On the other hand, people who fast or greatly reduce their caloric intake will experience a rise in levels of glucagon and epinephrine, producing Ghrelin, which is the stomach’s most powerful appetite stimulant.
Other Biological Factors that Contribute to Weight Gain
Where you live may contribute to your weight. Rising temperatures reduce our desire to eat, whereas a cold environment activates our hunger center.
Chronic stress, combined with a junk-food diet, drastically increases release of NPY.
Other factors like certain infections, sleep deprivation, and the composition of gut bacteria also affect our body mass.
Why am I so Fat?
So, overeating is only a surface explanation for being overweight. A large array of biological factors, some still unknown, contribute to our desire or feelings of needing to eat and how our body stores fat.
Other factors also contribute to being overweight: See: Why am I so Fat? A Psychosocial Perspective