Why do people end up on so many medications?
"Why do I have to take so many medications?"
I feel this is a question that is often asked of every health care provider. It is a question that stems from multiple feelings. It can be disbelief at the amount of pills swallowed in a day, the annoyance of remembering to take their medications, buying all of the drugs, and more. And in all honesty, I think it is a valid question. I enjoy the question. When I hear this question, it quickly tells me, that the patient may not be aware of what their medications do. This alone invites a moment for the patient to be educated.
"Why do you think you take these medications?" "Do you know what they are used for?" "How do you take your medications at home?"
If I hear, for instance, that the patient has not been taking their Lasix/furosemide (a diuretic or water pill) at home because they do not like the way it makes them urinate all the time, I may suddenly understand why they had an exacerbation of their congestive heart failure (CHF). Its poor work on our part not to educate patients and help them understand why they are on their medications and the purpose. In this patient, for instance, were they taking their pill in the evening and that is why they felt they had to pee all the time and could not sleep? Did they not know to take it in the morning instead? Where they ever told? Who knows, but its an opportunity to take and help the patient and prevent further issues through education down the road.
I am going to give a few sample patients to demonstrate how a person can be on multiple medications.
Example 1: Patient that has recently had a heart attack
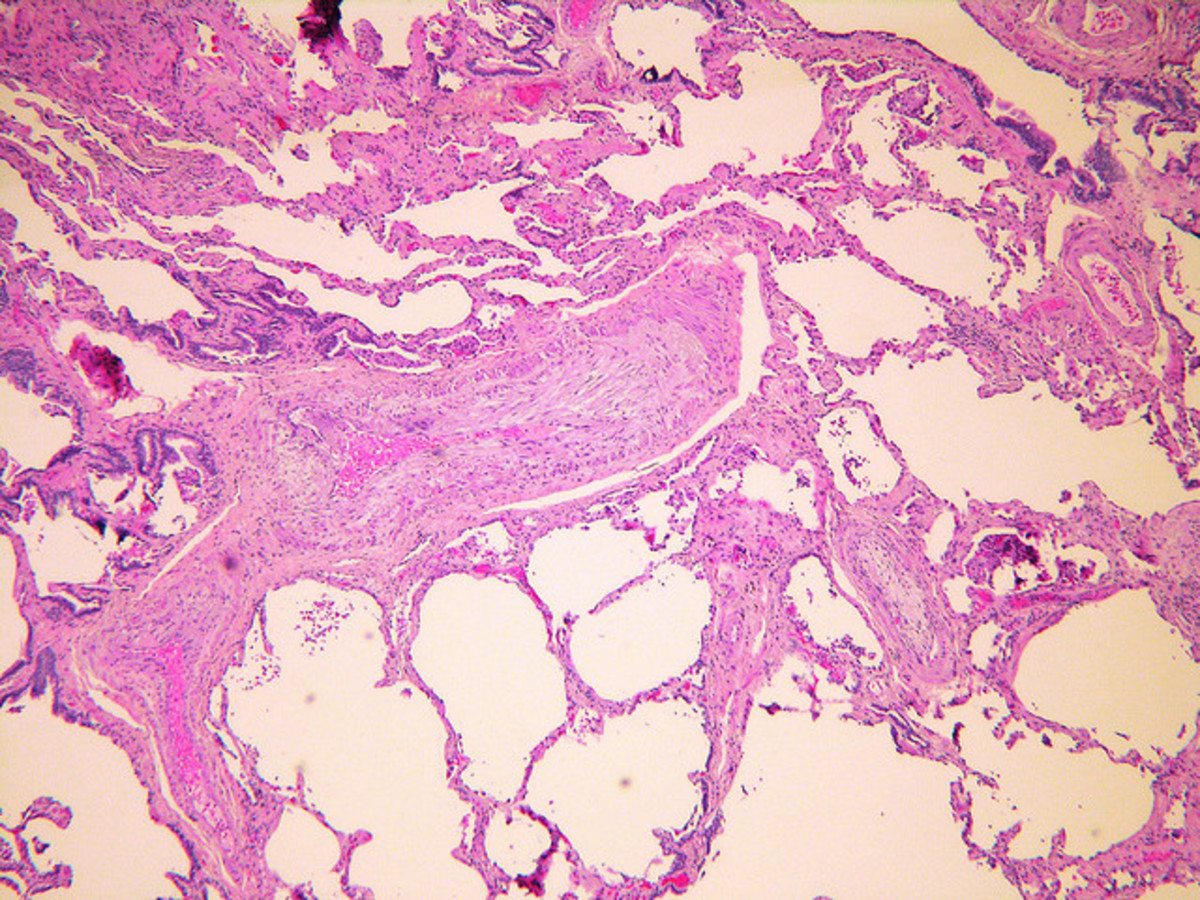
This I see frequently. A patient comes into the hospital with new onset chest pain, and trouble breathing. They were on a aspirin at home because they thought it was good for them, and maybe a proton pump inhibitor (PPI) for their acid reflux. Other than that, they take nothing. Now what? Lets say that they are taken to the Cath Lab and tests show that they have an occlusion, and they recieve a stent to open up the vessel that was blocked. Their labs demonstrate elevated markers for a myocardial infarct (heart attack), elevated Low-density lipoprotein (LDL or bad cholesterol), elevated heart rate and blood pressure, and maybe a elevated A1C or glucose levels (markers for risk of diabetes). What is this patient going to be discharged home on, and why?
- Beta-blocker - Drugs like Lopressor/metoprolol or Toprol may sound familar, and they are common drugs given to patients with a heart attack to reduce the patients heart rate. This helps the heart recover and reduces blood pressure.
- ACE Inhibitor - Drugs like lisinopril are given to help the heart recover and prevent the heart from remodeling and potentially developing heart failure in the future. They also help reduce blood pressure.
- Statin - Drugs like pravastain, simvastain, Lipitor/atorvastatin, Crestor are fairly common. These are to help reduce the cholesterol of the patient as evidence by the plaque build-up which led to the heart attack.
- Anti-platelet Therapy - Drugs like Plavix, Effient, Brilinta may be given. This is to help the stent placement from closing up and prevents further blockages from occurring. A patient may take this in addition to aspirin.
Right off the bat the patient walked in with two medications and walks out now having to possibly take 6 a day. And that is if those are enough to get him to a therapeutic goal that lowers his risk for developing another event (this is called secondary prevention - to prevent the heart attack from happening again). It must be kept in mind that this is all precautionary, these therapies help reduce the risk of an event or progression of a disease state from continuing, but it will not necessarily cure it.
These new drugs may be bothersome for a new patient. They are going to require labs to be drawn up yearly, close monitoring, and of course side effects. However, it is important for them to know why they are taking it. How about something that can be more burdensome?
Example 2: Patient develops diabetes
Let us say the previous patient, while taking their medications, did not make some lifestyle modifications and steadily gained weight (which may have been an issue before due to their elevated glucose). They were advised to watch their diet and to monitor themselves more, but they did not. Now a few years later their physician notices on their labs that they are now a diabetic, with accompanying signs and symptoms (urinating more, headaches, thirsty, etc.). What may be added?
- Metformin - This drug is taken multiple times a day, and helps reduce mortality in patients with diabetes. It is also helps reduce glucose levels overall and control diabetes progression.
- Oral Anti-diabetic medications - There are many drugs to help reduce blood sugars. I will not go into detail, but think of glipizide, glyburide, Actos, Junuvia, etc (These are all part of different drug classes). It may take more than one of these agents to control sugars.
- Insulin - A patient may end up on a insulin regimen if they fail oral therapy or their diabetes is incredibly uncontrolled. This may require multiple injections throughout the day.
Now, our patient went from being on 6 medications to possibly 8-12 different medications that they will have to take throughout the day. And all of these medications require close monitoring and will have side effects the patient will need to be aware of.
What if the patient develops complications from their diabetes?
- Diabetic Neuropathy - The patient may add on additional medications to modulate their pain that will have to be taken multiple times throughout the day. This could be anywhere from 1-3 more drugs.
- Chronic Kidney Disease to Possible Kidney Failure - This may require a whole slew of different medications to manage a patient with renal failure, which could add on another 3+ drugs depending on the severity and progression.
So now a patient may be 15+ in medications as their disease progresses.
Summary
- Patients may be on multiple medications to help reduce symptoms of their disease and delay progression
- These medications may be taken multiple times a day, adding on pill burden
- Medications come with possible side effects and drug interactions the patient must be aware of
- Medications alone will not solve everything. A patient must be willing to take measures to help control factors that place them at risk for chronic diseases and delay progression
- Live a healthy lifestyle
- Talk to your caregivers