Findings and Treatment of Women Chronic Pelvic Pain

Chronic pelvic pain is defined as noncyclic pain lasting at least 6 months that localizes to the pelvic girdle region; it must be of sufficient severity to cause functional disability or necessitate medical care.
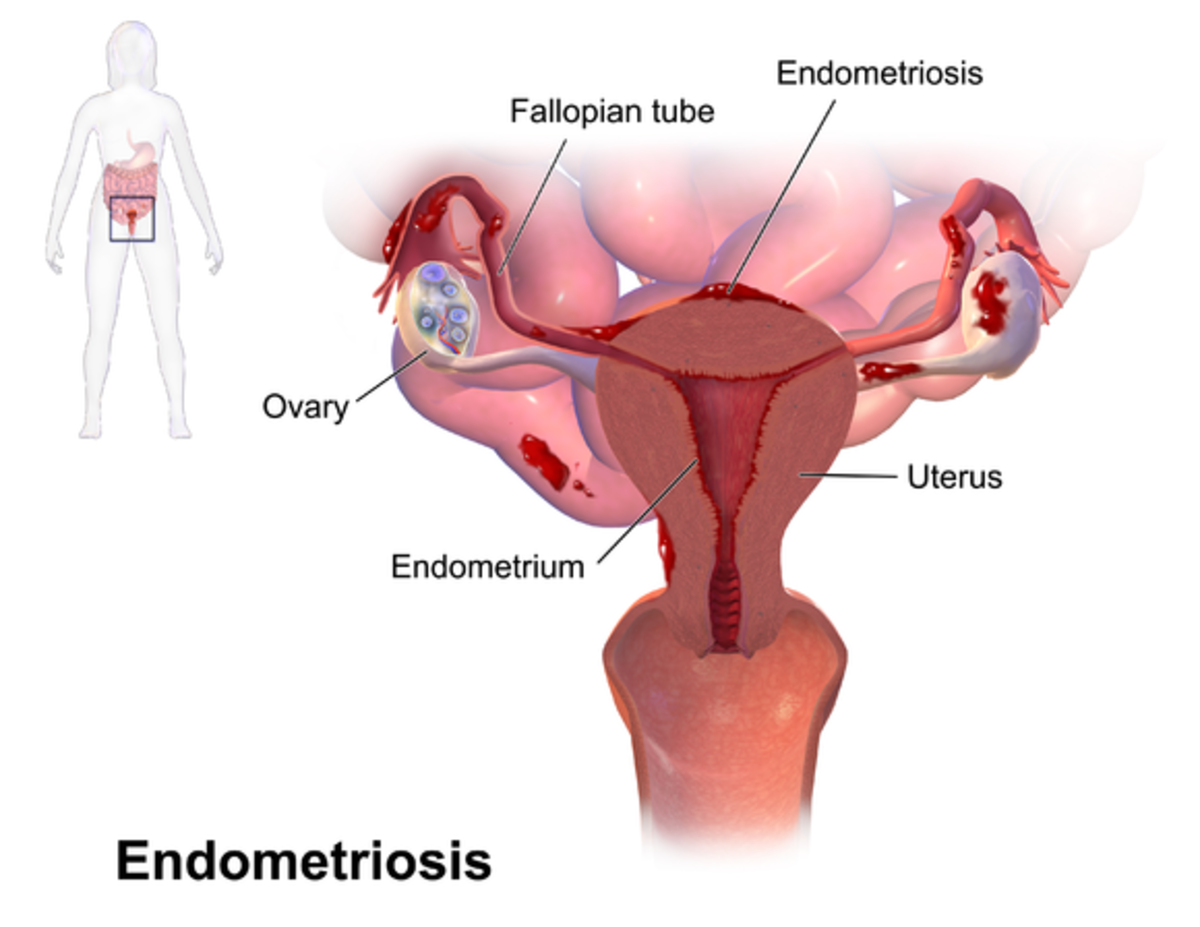
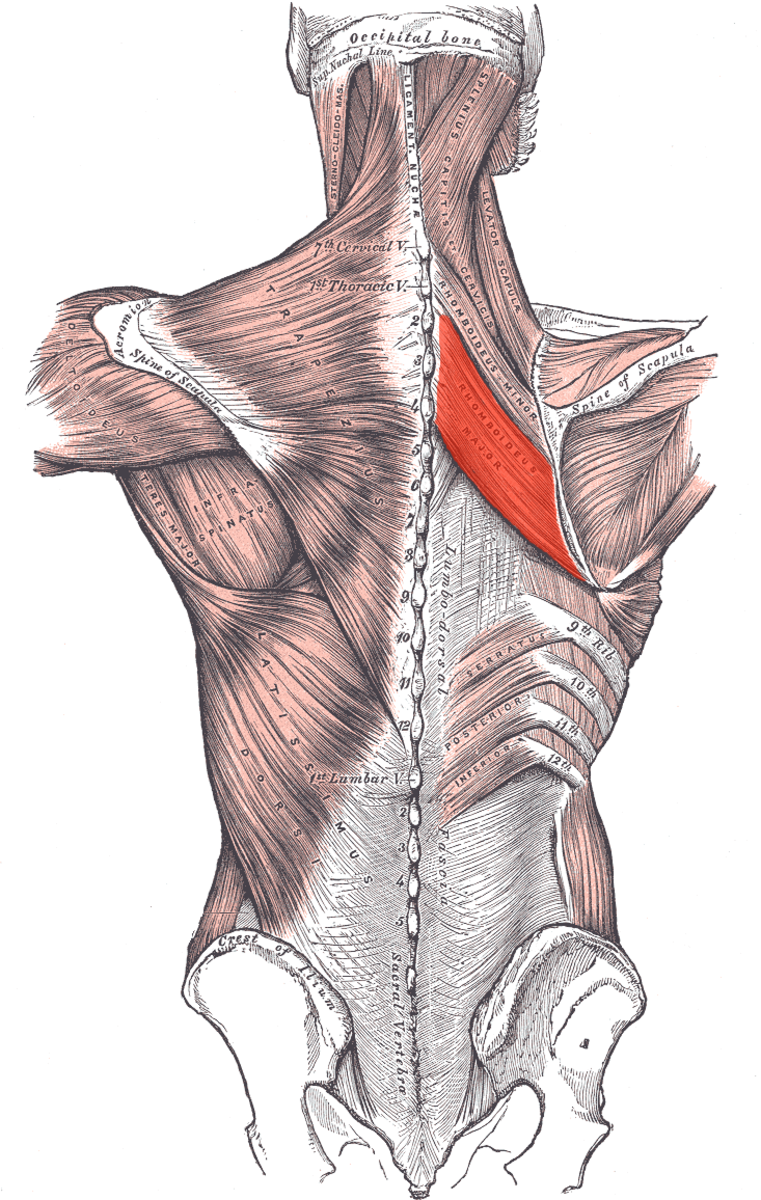
Endometriosis is diagnosed in up to one-third of women with chronic pelvic pain; other common etiologies include postoperative pelvic adhesions, pelvic varices, interstitial cystitis (IC), and irritable bowel syndrome (IBS). Musculoskeletal disorders such as myofascial pain syndrome and levator ani syndrome have also been linked to chronic pelvic pain.
Women with a history of physical and sexual abuse, pelvic inflammatory dis-ease, abdominopelvic surgery, or difficult obstetric deliveries are at increased risk for developing chronic pelvic pain.
Clinical Findings
A : Sign and Symptoms
Certain features of the history and physical examination can provide clues to the underlying diagnosis. Patients should be asked about the location, quality, and intensity of their pain as well as the relationship with the menstrual cycle, sexual activity, urination, and defecation.
Dysmenorrhea and dyspareunia are often experienced by patients with endometriosis, whereas dysuria, urgency, and frequency in association with pelvic pain are characteristic of IC. Pain related to pelvic varices is usually postural, worsening with prolonged standing and improving with leg elevation.
Patients with IBS often report abdominal pain, distention, and diarrhea or constipation. The physical examination, including the pelvic examination, is usually quite painful in the patient with chronic pelvic pain and should be done carefully.
A single digit internal vaginal examination should be done to localize the exact area of pain and to assess for trigger points along the pelvic floor muscles, which may indicate a musculoskeletal etiology for the pain. Palpable tenderness along the uterosacral liga-ments or cul de sac is suggestive of endometriosis, whereas women with IBS may experience anorectal tenderness.
Women with chronic pelvic infection may experience discomfort with palpation of the cervix and pelvic congestion may manifest as uterine enlargement or tenderness. The external genitalia should also be examined carefully to identify areas of vulvar discomfort because vulvodynia often coexists in patients with chronic pelvic pain. Notably, the absence of physical examination findings does not rule out significant pathology.
B. Laboratory Findings
Women who are at high risk for sexually transmitted dis-eases should be screened with cervical swabs for chlamydia and gonorrhea. Laboratory testing may be considered in women who have symptoms of IBS but also have associated anemia, rectal bleeding, or persistent watery diarrhea.
C. Diagnostic Testing and Imaging
Pelvic ultrasonography is useful for investigating any abnor-malities detected on physical examination, for screening patients in whom pelvic varices are suspected, and for pro-viding reassurance to the patient if the ultrasound is normal.
Additional testing may be done to confirm a suspected diag-nosis. Patients with IC often have a positive intravesical potassium chloride test or abnormalities detected on cystos-copy.
Laparoscopy may be helpful for diagnosing endometriosis or pelvic adhesions, although 35% of diagnostic laparoscopies are normal in patients with chronic pelvic pain.
Differential Diagnosis
Chronic pelvic pain is frequently a manifestation of another disease, as noted above. The history, physical examination, and diagnostic testing should be directed toward identifying patients with the most common "benign" underlying conditions, including endometriosis, pelvic adhesions, pelvic varices, IC, and IBS. Clinicians should be aware that patients frequently have more than one diagnosis contribut-ing to the chronic pelvic pain syndrome.
Less common but serious causes of chronic pelvic pain should also be considered in the differential diagnosis, including bladder malig-nancy, colon cancer, endometrial cancer, and inflammatory bowel disease. Accordingly, symptoms such as unexplained weight loss, hematochezia, and abnormal vaginal bleeding should be investigated thoroughly.
Many patients have no clear pathologic basis for their symptoms, and are thus diagnosed with idiopathic chronic pelvic pain.
Treatment
A. Medical Treatment
Medical treatment may focus on managing the chronic pain, the underlying condition, or both. Analgesics are com-monly used, and nonsteroidal anti-inflammatory drugs (NSAIDs), such as diclofenac and naproxen, are typically helpful.
However, patients and clinicians should be cautious about long-term use of these medications because long-term NSAID therapy can be associated with significant gastric toxicity. Antidepressants (eg, amitriptyline) and antiseizure medications (eg, gabapentin) (see Table 5-4), which have demonstrated efficacy in the treatment of other pain syndromes, may also be useful for chronic pelvic pain.
Opioid therapy improves pain but not functional or psy-chological outcomes and should generally be avoided. Hormonal therapies are used primarily for treating gynecologic sources of chronic pelvic pain. Women with endometriosis often benefit from treatment with combined oral contraceptive pills, which suppress ovulation and reduce dysmenorrhea.
Gonadotropin-releasing hormone (GnRH) agonists and progestins improve pain associated with endometriosis and pelvic varices. The decrease in BO associated with GnRH agonist treatment can be mitigated with estrogen or progesterone add-back therapy. Treatment with medroxyprogesterone improved pain scores in women with pelvic congestion, but symptoms returned with cessa-tion of treatment.
Medical therapies directed at the treatment of nongyne-cologic sources of chronic pelvic pain, including IC and IBS. Physical therapy and injection of identified trigger points provide signifi-cant pain relief in patients with musculoskeletal sources of pain. Similarly, physical therapy maneuvers that promote decongestion of the venous circulation (such as postural measures or manual drainage techniques) may be helpful in patients with pelvic congestion syndrome.
Psychological evaluation and treatment should also be strongly considered in all patients, both to improve treatment outcomes (particularly in patients with pelvic varices) as well as to address a history of sexual or physical abuse.
B. Surgical Treatment
Surgical treatment of chronic pelvic pain requires referral to a gynecologist. Condition-specific surgical treatments include ovarian or pelvic vein embolization in women with pelvic congestion syndrome, adhesiolysis in patients with pelvic adhesions and laparoscopic surgical destruction of implants in patients with endometriosis. Importantly, the efficacy of adhe-siolysis in the treatment of chronic pelvic pain is controversial. Presacral neurectomy has been shown to improve dysmenor-rhea in 80% of women with endometriosis.
Women with endometriosis who have persistent disease after medical and surgical therapies may benefit from hysterectomy, although his controversial as to whether concomitant oopherectomy improves symptoms further.
When to Refer
Patients should be referred to a gynecologist for diagnostic or therapeutic surgical procedures, if the underlying diag-nosis is unclear, or if the provider feels uncomfortable managing side effects associated with medical treatments lie, GnRH agonist therapy).