How I Lost 100 Pounds After Finally Understanding My Pcos.

I’ve been overweight my entire life. Not in a “gained a bit in college” way, but in a “this has been my reality since childhood” way. I was the kid in gym class trying to disappear into the wall during weigh-ins. I learned to be funny, charming, and confident because I figured if people were busy laughing, they weren’t focusing on my size. I was also the one being told by doctors year after year to “just lose weight,” with no regard for what was happening inside my body.
At 14, I was diagnosed with PCOS — Polycystic Ovarian Syndrome. It was the trifecta of signs: extra weight, irregular (read: non-existent) periods, and that darker skin around my neck (a classic sign of insulin resistance) that made the doctors take a closer look. I also had facial hair growth that made me self-conscious enough to carry tweezers in my school bag.
They did some bloodwork, gave me a diagnosis, and handed me a prescription for Metformin — the go-to med for PCOS. But I was 14. And honestly? I liked not having periods. I didn’t fully understand what this condition meant for me long-term, so I mostly ignored it. Took the script home, tossed it in a drawer, and got on with being a teenager.
Looking back, that was the first domino. Not the diagnosis itself, but how little I understood what it meant. And how little support I was given to truly understand it. I wasn’t told that this wasn’t just about periods. That it could impact my fertility, my skin, my mood, my metabolism, my blood sugar, my cardiovascular health — and my long-term quality of life. It was handed to me like a label, not a roadmap. And for a long time, I wandered through my health journey without a compass.
When “Eat Less, Move More” Doesn’t Work
As I got older, the weight kept piling on. And not because I was bingeing fast food or eating my feelings. My mom is a health nut, and that rubbed off on us. No chips, no pop, no sugary cereals in the house. I wasn’t perfect, but I wasn’t doing anything extreme either. And yet, the scale continued its steady upward climb.
By my late teens and early 20s, I felt like I was living in a body that was actively working against me. I would try a new workout program, or count calories, or eat “clean,” and get nothing in return. Not a single reward from my body for the effort. No lost pounds. No extra energy. Just frustration and self-blame.
At 21, I had a wake-up call. I learned the risks of unmanaged PCOS — like endometrial cancer due to lack of proper shedding — and finally started taking it seriously. I took my Metformin daily. I waited. One period came, then… nothing. The weight stayed put.
Back to the doctor I went. Their answer? “We’ve done what we can. There’s no cure.”
Cool.
So I got dramatic and asked about getting my ovaries removed. I figured hey, if it’s an ovarian syndrome, why not cut out the middleman? But that suggestion was met with dismissiveness and vague reassurances. I was repeatedly told that I just needed to try harder, lose weight, or accept that this was simply ‘how my body is.’ No one bothered to correct my fundamental misunderstanding of the condition’s root cause. That kind of repeated dismissal — combined with the lack of clear information and actionable help — is exactly where the medical gaslighting really kicked in.
It wasn’t just the words — it was the tone. The eye rolls. The sighs. The subtle implication that I was just looking for an easy way out or overreacting. One doctor even said, “Well, some women just have a harder time with weight. You’ll have to learn to manage your expectations.” And not once did anyone say, “Let’s dig deeper. Let’s look at why your body isn’t responding.” It was all, “Try harder, and if that doesn’t work, just accept it.”
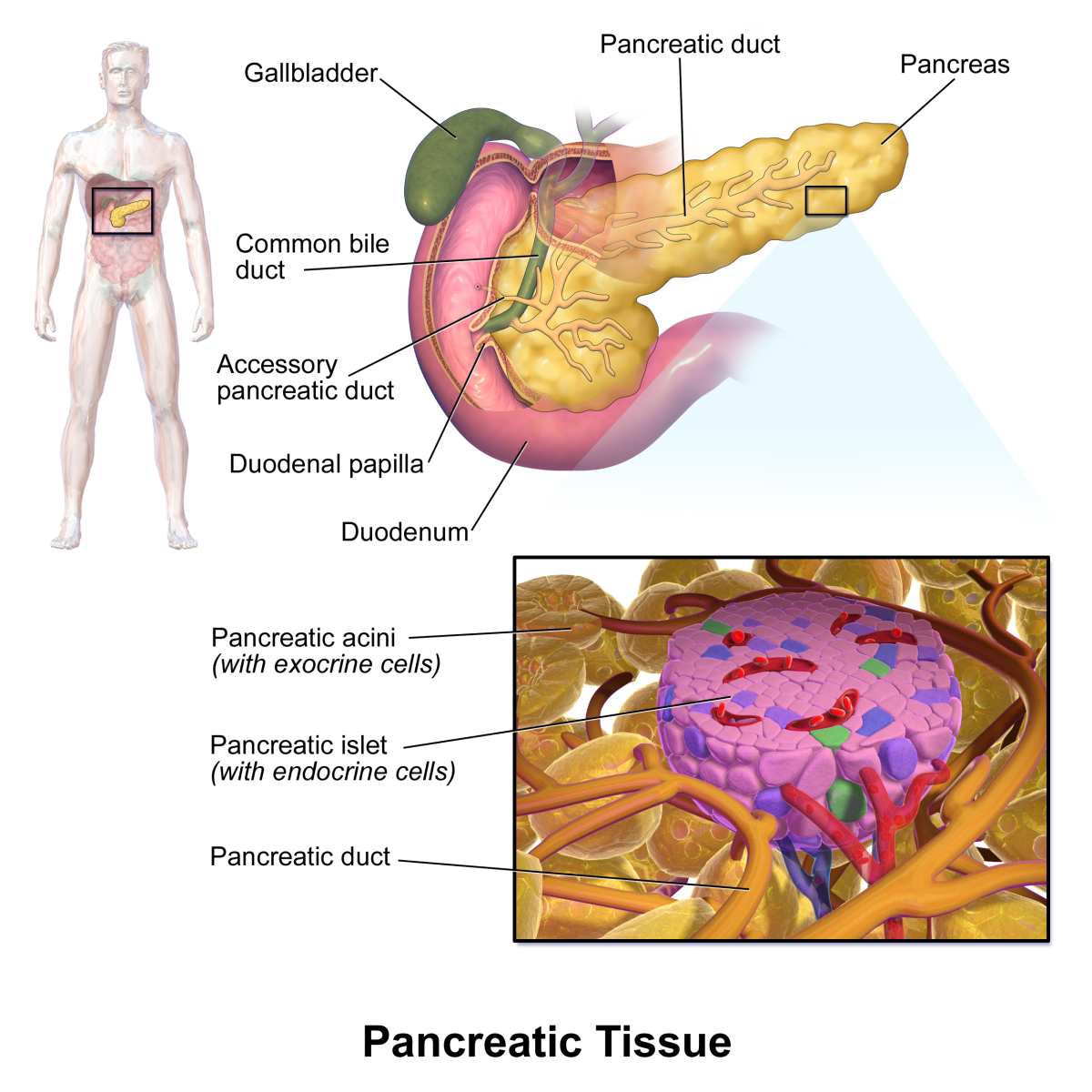
It’s an Endocrine Disorder, Not an Ovary Problem
The referral to an endocrinologist didn’t come easy. I had to push for it — hard. After years of hearing the same dismissive lines from primary care doctors, I started doing my own research. I stumbled across a few online forums where women were discussing their experiences with PCOS and how seeing an endocrinologist finally gave them answers. That planted the seed. At my next appointment, I asked my doctor point-blank for a referral. At first, they hesitated — told me it wasn’t necessary, that I “wasn’t diabetic.” But I insisted. I was tired of being handed prescriptions and sent on my way. I wanted someone who specialized in hormones, who could help me understand what was actually happening in my body.
After finally getting referred to an endocrinologist, I learned that PCOS is more accurately an endocrine disorder. Meaning it’s rooted in hormones — specifically, how your body produces and responds to them. The cysts? Just a symptom. The irregular periods? Symptom. The weight gain, acne, mood swings, unwanted facial hair, and skin darkening? Yep, all symptoms.
But the root cause is often hormonal imbalance — usually involving androgens (male hormones), insulin, and inflammation. For me, insulin was the big villain.
Turns out, my body makes insulin, but doesn’t use it. It just kind of… sits there. This is called insulin resistance, and it’s a major player in PCOS-related weight gain. Instead of breaking down sugars and using them for energy, my body stores them as fat. Neat.
This was the first time I felt like I had context for what was happening. Not just vague advice or scripts, but a biological explanation that made sense. And with that came the motivation to learn more — not because I hated my body, but because I was finally beginning to understand it.
I Did Everything Right — and Nothing Happened
Armed with a little more knowledge and a diagnosis that felt more specific than “just lose weight,” I was ready to take action. I wanted to do things the “right” way. No crash diets, no magic pills, no starvation. I signed up with a personal trainer who had experience working with women who had hormonal imbalances. I also consulted both a dietitian and a nutritionist. Together, we created a plan that ticked every box in the book: a modest calorie deficit, high protein, high fiber, whole foods, minimal processed junk, and just enough flexibility that I wouldn’t spiral into bingeing.
I tracked my meals with religious precision. I meal-prepped like I was auditioning for a YouTube channel. I worked out with my trainer three times a week, pushed myself through strength training and cardio intervals, and added in walks on my off days. I did everything that’s supposed to work.
And… nothing happened.
Not a pound lost. Not a single inch off my waist. No improved energy, no change in how my clothes fit. I was doing all the right things and getting none of the results. I felt like I was screaming into a void while people on Instagram lost 20 pounds in a month drinking “greens powder.”
And it’s not like I was building muscle and losing fat. I wasn’t losing anything. Even my trainer — who had initially been optimistic — started looking confused. I remember one check-in where he looked over my food log and said, “This should be working. I don’t get it.”
That’s the part no one talks about. When the professionals you trust start running out of ideas. When you’re the outlier. The exception. The mystery. And the worst part? Everyone assumes you’re cheating. Lying. Eating donuts in secret.
I wasn’t. I was exhausted, discouraged, and ready to give up entirely.
Everywhere you look — social media, YouTube, fitness forums — it’s the same mantra: “calorie deficit is king.” Eat fewer calories than you burn, and you will lose weight. It’s touted as universal truth. Science. Math. Unquestionable.
But here’s the thing no one tells you: that entire equation assumes your body is functioning properly. It assumes your metabolism is firing the way it should. That your hormones aren’t throwing a wrench into the machinery. That you don’t have a condition quietly hijacking your progress from behind the scenes.
The fitness industry doesn’t account for people like me. And truthfully? Neither do most professionals. Most personal trainers aren’t taught about endocrine disorders. Most dietitians aren’t trained to spot the subtle signs of hormonal imbalances. Unless you land with someone truly specialized, the advice you get will likely be generic — and ineffective.
So yes, a calorie deficit might work for someone with a healthy, functioning system. But for people with insulin resistance? That deficit might just mean fewer nutrients going into a body that’s already in chaos. It’s not as simple as “eat less, move more.” And I wish more people — especially in the health world — would say that out loud.
The Diet That Finally Worked — for Me
Once I understood that insulin resistance was the real culprit in my case — not a lack of discipline or motivation — I started seeking out support from people who actually got it. I found a dietitian who specialized in hormonal imbalances and had extensive experience with PCOS. That already felt like a miracle. From our first session, it was obvious she was operating on a different level than anyone I’d worked with before. She didn’t roll her eyes when I explained my symptoms. She didn’t say “just eat less.” She listened. And she tailored a plan to my body.
She explained that the goal wasn’t to eat less — it was to stabilize blood sugar. PCOS and insulin resistance create this vicious cycle where your blood sugar spikes, crashes, and sends your body into panic mode, causing cravings, fatigue, and fat storage. Breaking that cycle was key. That meant focusing on:
- Low-glycemic, complex carbohydrates (like lentils, sweet potatoes, and steel-cut oats)
- Pairing every carb with protein and healthy fat
- Eating on a consistent schedule (no skipping meals!)
- Cutting out refined sugar as much as possible
- Reducing inflammation-triggering foods like processed snacks and industrial oils
What really helped was reframing how I looked at food. This wasn’t a “diet” in the typical restrictive sense — it was a way to eat that supported my hormones instead of sabotaging them. Instead of obsessing over calories, I focused on balance. I started plating meals with intention: half veggies, a quarter lean protein, a quarter slow carbs. I still ate carbs. I still had chocolate sometimes. I didn’t feel deprived.
And for exercise? I stopped treating it like punishment. I didn’t force myself to do 90-minute gym sessions or sign up for boot camps I dreaded. Instead, I moved in ways that felt good. Some days it was a walk. Some days it was dancing in the kitchen while cooking. Some days it was nothing — and that was okay too. I prioritized consistency over intensity.
The difference was almost immediate. Not in the numbers, but in how I felt. I had more energy. My sleep improved. My skin looked clearer. And eventually, yes — the weight began to come off.
But it wasn’t the scale that motivated me anymore. It was feeling like I had finally found a rhythm with my body instead of fighting it tooth and nail.
Then the Weight Started Melting Off
At first, it was slow — like a couple pounds here and there. Just enough that I could convince myself it wasn’t a fluke. Then, suddenly, the needle started to move fast. It felt like every week I was noticing another difference. My jeans got baggier. My bras started gaping. I had to add a new notch to my belt.
In seven months, I lost 103 pounds. No surgery. No starvation. No Ozempic. Just science that actually applied to me.
Yes, really. Just food that worked for my body and movement that didn’t feel like torture. And Metformin, of course — which I finally took consistently and correctly alongside the diet.
It was shocking how quickly things changed once I aligned my eating habits with my physiology. My doctors weren’t concerned about the speed of my weight loss. In fact, one of them said, “This isn’t unhealthy. This is your body finally letting go of what it’s been holding onto for years.”
I started at 289 pounds. I now sit around 176. I’ve hit plateaus, sure — but that’s normal. What matters most is that I feel good. I can walk through a grocery store without back pain. My knees don’t ache. I don’t dread putting on clothes or seeing my reflection in store windows. I can exist in my body without feeling like I’m being punished for something.
And perhaps most importantly, I feel proud. Not just for the weight I lost, but for the persistence it took to finally understand how my body works — and how to work with it instead of against it.
This Isn’t a “How-To” — It’s a “Here’s What Helped Me”
Before anyone goes searching for a carbon copy of my meal plan or exercise routine, let me say this clearly: your PCOS is not my PCOS.
Some people with PCOS have zero weight issues. Some don’t have insulin resistance. Some have adrenal-type PCOS. Some can manage their symptoms through lifestyle alone. Others need medication, or even multiple types of medication. Some people thrive on intermittent fasting. For others, skipping meals throws their entire system into chaos. This isn’t a one-size-fits-all condition — and anyone who tells you otherwise is either selling something or oversimplifying the hell out of it.
Everything I shared here is simply what finally worked for me, after years of trial and error, failed attempts, medical dismissals, and a lot of unlearning. I’m not a doctor, dietitian, or hormone whisperer. I’m just someone who spent over a decade living in a body I didn’t understand and finally cracked the code — my code.
This isn’t medical advice. It’s lived experience. It’s a personal victory I wanted to share because I know there are thousands of women out there feeling defeated, ignored, and broken. If you’re one of them, please know: you’re not any of those things. You’re not lazy. You’re not doing it wrong. You might just be missing the right map.
So take what helps, leave what doesn’t, and never stop advocating for yourself. You know your body better than anyone.
And if there’s one thing I’ve learned through all of this, it’s that being an advocate for yourself isn’t optional — it’s essential. Women are dismissed by medical professionals at an alarming rate. Overweight women? Even more so. There is a distinct lack of care, empathy, and understanding when you walk into a clinic in a larger body and ask for help. The default assumption is often that you’re lazy, irresponsible, or simply not trying hard enough. You have to fight harder. Push louder. Ask better questions. Demand referrals. Insist on second opinions. Advocate fiercely to get the tests, the appointments, and the answers you deserve. Because generic advice doesn’t work when your body is dealing with something specific and complicated.
You have every right to take up space in a medical office. And you have every right to be taken seriously.
You’re not just allowed to take up space — you’re allowed to take control of it, too.
This content is accurate and true to the best of the author’s knowledge and does not substitute for diagnosis, prognosis, treatment, prescription, and/or dietary advice from a licensed health professional. Drugs, supplements, and natural remedies may have dangerous side effects. If pregnant or nursing, consult with a qualified provider on an individual basis. Seek immediate help if you are experiencing a medical emergency.
© 2025 Callie James