Medicare and Medicaid Fraud:Get Angry and Learn how to Fight it
President Lyndon Johnson signing the Medicare bill on July 30, 1965

Have you ever stopped to review your discharge papers after leaving an emergency room? Have you ever sat down to review an explanation of benefits letter received from you health insurance company? Do you check billing statements from providers for mistakes?
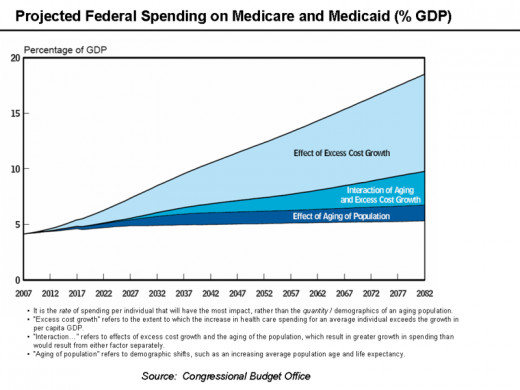
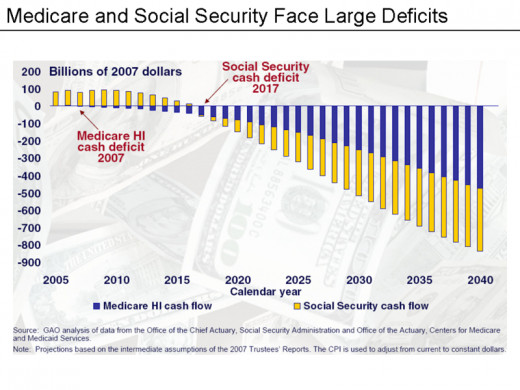
Despite the numerous concerns that Medicare funds could be depleted by 2024, many people being asked these questions, have responded in the negative. In order to fully appreciate this concern you need to have a better understanding of Medicare and Medicaid.
Medicare
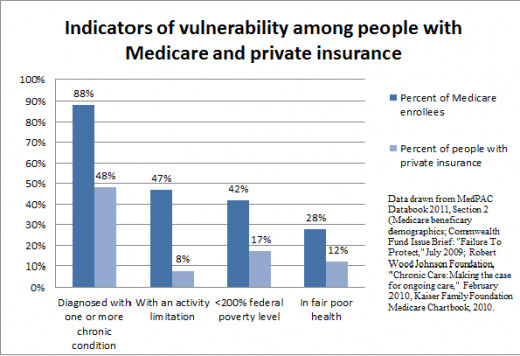
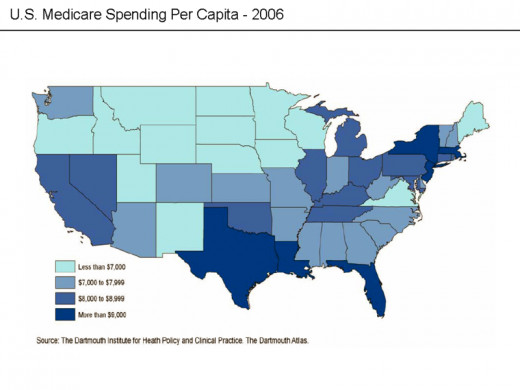
Medicare is a social insurance program. There are approximately 48 million people in the United States who are enrolled in Medicare. People who are over age 65, younger than age 65 with specific disabilities and those who are receiving renal dialysis are eligible for Medicare. The annual net spending on Medicare is approximately $508 billion dollars. According to reports, the number of individuals enrolled in Medicare is expected to increase by 36 % by the end of 2023.
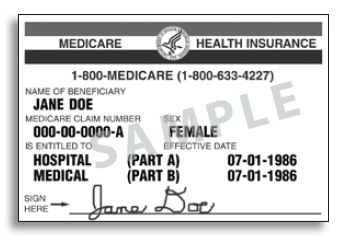
Medicare consists of a Parts A , B, C and D. Medicare Part A covers hospices, hospitals, primary doctors and skilled nursing facilities. Medicare Part B covers services like diagnostic testing as well as preventative care. Preventative care includes services such as mammogram screening, prostrate exams and pap smears. Medicare Part C allows private insurers to provide Medicare under PPO and HMO plans. Medicare Part D is an optional plan provided through private insurers who contract with the government. Part D provides for outpatient prescription drug coverage.
Medicare is funded by payroll taxes of employees, employers and by small business owners. Medicare is also funded by social security taxes and income earned on trust funds. It is also funded by premiums paid on Medicare Part A. Medicare was the primary payer for inpatient hospitalization in 2011.

Medicaid
Medicaid is a social health care program for families and people with low income. One third of all children and approximately 60% of low income children are on Medicaid. Medicaid covers many services that include Nursing home care, family planning, transportation services to appointments, dental care, treatment in psychiatric hospitals, medical equipment and others. Eligibility for Medicaid requires a disability and receipt of Supplemental Security Insurance benefits (SSI).
Medicaid is funded by both state and federal funds. Each state determines how its Medicaid program is run. Medicaid enrollment continues to rise. For example, Washington State is expected to enroll approximately 270,000 by the end of 2014. In Oregon, 70,000 people signed up for Medicaid in a single month. It is expected that 223,000 people on Oregon will be enrolled by 2015. Maryland is expected to enroll 110,000 by the end of 2014.
Combined, Medicare and Medicaid enrolees outnumber the number of people employed in private sector positions. This should concern all of us. Based on our aging population and the high incidence of chronic diseases resulting in disability, you could be the next enrolee under the Medicare or Medicaid program.
An ordinary citizen who is self educated on Medicare/Medicaid fraud
Medicare and Medicaid Fraud
You may not be aware that millions of dollars of Medicare and Medicaid monies are wasted each year due to fraud. The Federal False claim act of 1986 prohibits the knowing submission of false claims to the federal government. The United States may sue false claim perpetrators for treble damages plus $5,000 to $10,000 for each false claim presented. Individuals (relators) may also sue on behalf of the government. Claims brought by individuals on behalf of the government are called qui tam claims.
Relators are entitled to 15 to 25% of the monies recovered on behalf of the government. Relators usually recover more than $1million for reporting Medicare/Medicaid fraud. If you report fraud against your employer, you are protected by a whistleblower protection act of 1989. The whistleblower protection act prohibits your employer from demoting, suspending, harassing, terminating or taking other adverse acts against you for filing a complaint.
There are several types of Medicare and Medicaid fraud that you should be aware of. They are as follows:
- Billing for Services that were never provided
- Prescription Fraud
- Billing for Worthless services
- Up-coding
- Billing for care that was unnecessary
- kick backs for prescribing or promoting Medical Products
This list is not all inclusive
Kathleen Sebelius, Secretary of Health and Human Services (HHS) announced initiative in 2009 to fight Medicare fraud, waste and abuse

Have you or any family member ever encountered Medicare/Medicaid fraud?
Billing for Services that were never provided
How can you tell that a service that was billed for was not rendered? The answer may lie in your Medicare Summary Notice (MSN). The MSN shows all services that were billed to Medicare with the name of each provider. The MSN also shows what bills were paid by Medicare as well as any monies owed by you. A MSN will be sent to you every three months if you are a recipient of Medicare. The MSN may also be accessed on line from MyMedicare.gov within 24 hours after the claim has been processed by Medicare.
You should examine your MSN closely for mistakes. If you see a procedure listed on your MSN that does not match your diagnosis, or if you see a procedure that you know was never performed, you should contact Medicare. Medicare will also send you an explanation of benefits (EOB) letter related to your prescription plan. This shows what claims were made, the date and the costs. Review the EOB carefully for mistakes. Contact Medicare for irregularities. For example, irregularities may exist if you see items that were never provided to you, or if you notice the name of a brand name drug despite being given a generic drug.
Medicaid does not usually provide an EOB letter. However, you should not hesitate to contact the social worker at a hospital or nursing home, or a case manager for help with explanation of benefits. You may receive a bill from a provider despite being covered by Medicaid. If that problem persists after notifying the provider, you may contact your local Medicare office. Providers are not allowed to bill you if you have Medicaid.
The phone number for Medicaid should be printed on the back of your Medicaid card. You may also go to the Medicaid.gov website and click on your state link to get the phone number. Review any information sent to you from Medicaid.
Make sure that you review your discharge papers after leaving an emergency room. You should ask for a print out of services provided from the provider before leaving a doctor’s office. A doctor who is running a clean operation should have no problems giving this to you.
If you believe that a provider made an honest mistake you may contact your healthcare provider prior to contacting Medicare and Medicaid.
Medicare round table with seniors. Talking about the issues is one step in the fight against Medicare/Medicaid fraud

Remember that these are common types of fraud
- Billing for Services that were never provided
- Prescription Fraud
- Billing for Worthless services
- Up-coding
- Billing for care that was unnecessary
- kick backs for prescribing or promoting Medical Products
Cases where providers have billed Medicare and Medicaid for services that were never provided
There are countless cases where providers have billed Medicare and Medicaid for services that were never provided.
On October 8, 2013, Richard Hogan and Glenn English of Detroit were convicted of conspiracy to commit healthcare fraud and fraud respectively. The fraud scheme consisted of billing for services that were never provided. Both Defendants operated New Century Adult day care in Michigan. The pair brought in patients that were mentally disabled, and patients seeking narcotic drugs. The perpetrators then used the patient’s names to bill for psychotherapy that was never provided. In order to lure the drug seeking patients in, the defendants had advised them that if they signed up for the psychotherapy program they would get the narcotic drugs that they were seeking [1]
In another case, Maxim Health Care Services (Maxim), a privately held home health care agency headquartered in Maryland, defrauded the federal government out of millions over several years. In 2011, Maxim admitted to defrauding the federal government out of $61 million. The fraud was discovered by a patient who was told that he had exceeded his eligible hours of home care services. The patient was disabled and needed home health aides to assist him at home. The concerned patient dug through his records and upon review, found that he was billed for numerous hours of care by aides who were never provided. [2]
Upon further investigation, it was discovered that Maxim was reimbursed $2 billion dollars over a six year period for their billing statements. The Maxim employees who orchestrated the scheme were indicted and given various sentences. The company was required to pay penalties totaling $150 million dollars. [2]
Victim of Medicare Fraud Speaks Out
Declare war against Prescription fraud

Prescription Fraud
Pharmacies may engage in health care fraud by billing for prescriptions that were never filled. The monies are then pocked by perpetrators. As such, don’t simply throw letters received for a decedent from insurers in the garbage.
In 2013, a Florida a pharmacist and his mother were indicted for health care fraud. The pair orchestrated a scheme whereby they billed the federal government for numerous prescriptions that were never filled. The names on the prescriptions belonged to many deceased patients. The scheme included other patients who were unaware that their names were being used. The defendants were required to return $350,000 to the federal government and face up to 10 years in prison. [3]
In 2009, pharmacist Brian Ulloman of Kentucky was sentenced in federal court for prescription fraud. This pharmacist knowingly collected drug samples from doctors and a pharmaceutical company representative then relabeled and sold them at his pharmacy. Samples cannot be sold on the market. Many of these drugs were sold to recipients of Medicare and Medicaid. Brian Ulloman was sentenced to 1year and three months in prison. He was required to repay $2.3 million dollars for the fraud count and other crimes. [4]

Billing for worthless services
Worthless services are services that are so deficiently performed that the patient did not get a benefit from them. The theory behind worthless service is that the service was so poorly performed that it equated to never being performed at all. Carefully examining health care environments may help you detect worthless services. When you go to a Nursing home, walk around and look. Does the room smell? Are there bugs running around? Are the floors dirty?Do nurses make infrequent rounds?
Many nursing homes provide deficient care to patients. Billing for services that were too deficient to be qualified as being performed is Medicaid fraud. Worthless services occur where Medicaid is billed for services where there is severe staff shortage, insanitary conditions, high rate of bed sores serious falls, failure to meet nutritional and rehabilitation needs and the service so lacking that it cannot enhance quality of life. This list is not all inclusive.
Most Nursing homes accused of providing worthless services usually pay a fine and are not eligible for Medicaid reimbursement. In 2012, the operator of three Georgia Nursing homes was indicted for Medicaid fraud for providing worthless care to residents. The evidence revealed that patients at the Mount Berry, Moran Lake and a Wildwood Nursing homes were subjected to food shortage, lack of staff, leaking roofs, lack of adequate housekeeping services, insects, rotting garbage and moldy insanitary conditions. The defendants billed Medicaid for $32.9 million dollars. The defendants face up to 20 years in jail. [5]
Two employees at the Momence Meadows Nursing home in Illinois reported the facility for providing worthless care. The care provided by Momence Meadows resulted in the death of three patients. The patients at that facility had numerous bed sores. A $28 million dollar fine verdict was imposed upon the defendants. [6]

Billing for care that was unnecessary
Billing for unnecessary care is one of the most frequent types of health care fraud schemes. Closely examining your MSN or a billing statement from a provider may help you detect this type of fraud. You may also have access to this information if you work in a health care facility or related to a patient who had the unnecessary procedure. You must disclose the patient's full information if known, date of the procedure, type and the provider's name.
For example, two doctors and a therapist from a Miami Mental health clinic orchestrated a scheme whereby patients were paid to recruit ineligible beneficiaries to the Clinic for therapy. The patients selected either would not benefit from therapy or did not have a mental health diagnosis. The providers in the clinic created false therapy notes and submitted false claims to the Medicare totaling $100 million. Careful review of those claims led to the discovery of Medicare fraud. The perpetrators were indicted and given up to 50 years in jail. [7]
In January 2014, St Mary’s Hospital in London Kentucky settled an unnecessary care claim with the Federal Government for $16.5 million. St Mary’s cardiologist Dr. Sandesh Patish admitted to routinely performing cardiac stents on patients who did not need them. The cost of performing these stents was billed to Medicare. Dr. Patish faces up to 30 months in prison. [8]
The case against St. Mary exemplifies how the lives of patients may be placed in jeopardy by health care fraud, as heart procedures by nature place patients at risk of death.
Up-coding
Fraud related to up-coding cost Medicare millions of dollars every year. Up-coding is the process of billing for a procedure at a higher procedure code than what was actually performed. Up-coding may result in prescribing a more expensive drug or therapy than the patient actually needs. All medical conditions, treatments and tests have a CPT and ICD9 codes. The CPT codes are used for identifying procedures and services of physicians. CPT codes are universal and specifies the payment amount. ICD9 codes represent types of diseases and diagnoses.
If you look at your medical bill, you may see a number beside the test (CPT) that was allegedly done or beside your diagnosis(ICD9). The Center for Medicare and Medicaid services has a fee schedule for certain services posted on its website. The website address is:
http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/FeeScheduleGenInfo/
Information on CPT codes may also be obtained from the American Medical Association at http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/cpt/about-cpt.page. Up-coding is a common practice. A patient may go to an emergency room with a particular complaint only to read her discharge note and see a diagnosis unrelated to her care. This happened to my friend recently. She went to a hospital complaining of chest pain and was given an admitting diagnosis unrelated to her care.
A criminal complaint for up-coding was recently filed against a Dike Ajiri from Chicago. Dike Ajiri owned and operated a mobile medical service for people who were confined to their homes. Dike Ajiri and a doctor allegedly orchestrated a scheme whereby bills were up-coded at a higher rate by contending that the procedures performed in patient homes were more difficult and required a longer time.
Employees and patients of the mobile service who were interviewed by the Department of Justice stated that the procedures conducted in the home lasted 10 to 30 minutes. However, the mobile service's minimum documented time was 40 minutes. The billing code for the mobile service was $122.82. The highest code average cost for the procedure was $171.25. Between January 2007 and June 2008 all of mobile company's procedure were billed only at the highest code fee. The doctor and Dike Ajiri face a maximum of 5 to 10 years respectively in prison and a $250,000 fine. [9]
In February 2012, Endogastric Solutions Inc., in Washington, was forced to pay the government up to $5.25 million for fraud related to up-coding. Endogastric solutions Inc., was the maker of a new device used to test for gastro esophageal disease. This equipment was a new less invasive device. The maker of the device trained the physicians in the use of the device and knowingly misled them into using a higher incorrect CPT code for procedure billing. The physicians performed the procedure for gastro esophageal disease on numerous patients and billed Medicare for performance of the more invasive procedure. [10]


Kickbacks for prescribing or promoting Medical Products
Despite, the many reprimands and publicized cases, people in the health care industry still violate the anti kickback law due to the appealing financial incentives. The federal anti kickback statute prevents any type of remuneration to induce items, services or referrals that are paid for by the Federal government. Kick backs occur in many ways. For example, you may notice an unusual relationship between a doctor and a pharmaceutical company representative. You may also notice a facility getting lavish gifts for sending patients to a particular lab. If you see something, say something.
In April 2013, the Federal government filed a fraud claim against Novartis for violation of the anti kick back laws. Novartis is New Jersey drug manufacturer. For over 10 years, Novartis allegedly paid remuneration to doctors for promoting its drugs. Novartis gave monies and lavish dinners to doctors who spoke at seminars advertising its brand name drugs. Most of these dinners were at high end restaurants. Based on this scheme, Novartis caused several claims to be submitted to Medicare and Medicaid. [11]
In February 2014, Omnicare National pharmacy settled with the Federal Government for $4.19 Million for allegations that it participated in a kickback scheme. Omnicare solicited and received kickbacks for Amgen. Amgen is a large pharmaceutical company. Omnicare orchestrated with Amgen to implement a program whereby Medicare/Medicare patients were switched from a less expensive drug product to Aranesp, a brand name drug manufactured by Amgen. [12]. Aranesp is primarily used for treating anemia in patients on chemotherapy or those with chronic renal failure.
Prior to this, Omnicare settled another kickback claim with the federal government for $98 million. According to the indictment, Omnicare accepted payments from Johnson and Johnson (J&J) for recommending its brand name drug Risperdal (an antipsychotic drug) to nursing homes. Omnicare was given market shares and payments disguised as fees by J&J. Omnicare in turn offered kickbacks to the Nursing home who agreed to carry Risperdal. [13]

Reporting Fraud
Now that you have learned about several types of fraud, the next step is the reporting process. Don't be afraid. Remember that anyone can report Medicare/Medicaid fraud. To report fraud you may contact 1800 Medicare or the Office of Inspector General's website at: https://forms.oig.hhs.gov/hotlineoperations/
Prior to making the report you should gather the following information:
- The Hospital and or health care provider’s name
- The date the services were performed
- The types of services
- The amount of monies that was paid by Medicare insurance or the amount that was approved
- The reason why you believe that the hospital of health care provided should not be paid
The online reporting form that is provided by the Office of Inspector General has several sections.Carefully complete each section by answering all questions that are asked. Once submitted, this form will be forwarded to a field investigator in the city where the fraud occurred.
Remember, that if are covered under both Medicare and Medicaid, and you received services covered under Medicare, your health acre provide cannot bill you for a Medicare co-pay. If you are a Qualified Medicare Beneficiary (QMB) and was billed for a co-pay for Medicare, you should report this to Medicare. A QMB is a person whose income does not exceed 100% of the federal poverty limit. If you are a QMB, Medicare pays all your premiums, coinsurance and deductibles for Parts A and Part B.
There is also a monetary incentive for reporting fraud. If you report Medicare fraud, you are entitled to a $1000.00 reward. However, to be eligible for the award, the fraud that you reported must be confirmed by the Federal government. The reporter must not be a participant in the fraud. Moreover, if the health care provider or the hospital is already under investigation then the reporter is not eligible for the reward. Additionally, the federal government must recover at least $100.00 of its monies for the reward to be given.
In 2007, the United States Department of Justice initiated a new Medicare Fraud Strike Force to address the high rate of Medicare/ Medicaid fraud. The task force has prosecuted over 15,000 individuals who have billed the government over $5 billion dollars collectively.
Have this information handy when reporting Fraud
Name
| The Hospital and or health care provider’s name
|
Date
| The date the services were performed.
|
Type
| The types of services
|
Monies
| The amount of monies that was paid by Medicare insurance or the amount that was approved
|
Reason
| The reason why you believe that the hospital or health care provided should not be paid
|
Conclusion
The government cannot fight fraud successfully without your help. Fraud not only depletes government funds but also cause health care providers to place patient lives at risk. Remember that doctors who prescribe drugs or use medical equipment based on financial incentives, are not using their best judgment in providing you with medical care.
As a Medicare or Medicaid recipient, educating yourself about the monies that are being paid on your behalf is one step in helping to prevent our Medicare Medicaid system from crashing. Every America citizen has a duty to help the government preserve Medicare and Medicaid monies so that these funds will be available when we need them.
References
[1] Owner of fake Michigan Psychotherapy Clinic sentenced for Role in Medicare fraud scheme: Retrieved from: USDOJ. http://www.justice.gov/opa/pr/2014/February/14-crm-217.html
[2] Maxim Healthcare Services charged with fraud, Agrees to pay approximately $150 Million, enact reforms after false billing revealed, as common practice. USDOJ. Retrieved from:
http://www.justice.gov/opa/pr/2011/September/11-civ-1169.html
[3] Florida pharmacist, mom submitted prescription bills for dead people. Retrieved from: ABC-7.com http://www.insurancefraud.org/IFNS-detail.htm?key=17553#.Uw9ctfldUlo
[4] Local pharmacist sentenced to 1 year and three months for health care fraud; and campaign contribution fraud. Also enters in $300,000 civil settlement for healthcare fraud. Retrieved from: http://www.fda.gov/downloads/NewsEvents/Newsroom/PressAnnouncements/UCM179395.pdf
[5] Atlanta Man Convicted for Billing 32.9 Million for worthless services while operating “Horrendous” nursing home. USDOJ. Retrieved from: http://www.justice.gov/usao/gan/press/2012/04-03-12.html
[6] Federal Courts should not be rigged in favor of corporations; Retrieved from:http://www.fbi.gov/atlanta/press-releases/2012/atlanta-man-convicted-of-billing-32.9-million-for-worthless-services-while-operating-horrendous-nursing-homes
[7] Doctors, Therapist and Recruiters from Miami-Area Mental Health Care Corporation
Convicted for Participating in $205 Million Medicare Fraud Scheme. USDOJ. Retrieved from:
http://www.justice.gov/opa/pr/2012/June/12-crm-708.html
[8] St Joseph’s London Hospital to Pay $16.5 million to settle false claims act allegations of Unnecessary Heart Procedures. USDOJ. Retrieved from:http://www.justice.gov/usao/kye/news/2014/2014-01-28-sjhlondon.html
[9] Mobile Doctor’s Chicago CEO and Doctor’s Arrested on Federal Health Care Fraud Charges; Offices Searched in Three Cities. USDOJ. Retrieved from: http://www.justice.gov/usao/iln/pr/chicago/2013/pr0827_01.html
[10] Washington based Medical device Manufacturer to pay up to $5.2 million to settle Allegations of causing false Billing of Federal Health Care programs: USDOJ. Retrieved from: http://www.justice.gov/opa/pr/2014/February/14-civ-173.html
[11] United States files complaint against Novartis Pharmaceutical corp. for allegedly paying kickbacks to Doctors in exchange for prescribing its Drugs. USDOJ. Retrieved from: http://www.justice.gov/opa/pr/2013/April/13-civ-481.html
[12] Omnicare to pay Government $4.19 million to resolve false claims acts allegations. USDOJ. Retrieved from: http://www.justice.gov/opa/pr/2014/February/14-civ-216.html
[13] Nation’s largest nursing home pharmacy and pharmaceutical manufacturer pays $112 million to settle False Claims act case. USDOJ. Retrieved from:http://behnwyetzner.com/sites/default/files/omnicarekickbacks/Omnicare-USDOJ-Release.pdf
Other Resources
Cecile Portilla - Managing Obstacles to Employment after Termination
Cecile Portilla- Why the Concept of High Quality Healthcare while Making Big Profits is often Misleading. (This article can be googled or accessed by going to ezine pages at http://ezinearticles.com/?expert=Cecile_Portilla)