Rubella Is Still Out There
Just One of the Many Viruses Out There

More Recent Concerns Are COVID-19 and Monkey Pox
Of course, these days everyone is more concerned about the pandemic of COVID-19 and all its variants, and Monkey Pox — as we should be. Still, we cannot let ourselves forget that other viruses are out there. Many of them we have fought for decades, even centuries. Others, we haven't seen yet. This article is about Rubella (German measles) because I know more about it.
We Previously Believed Rubella Had Been Wiped Out in the United States
Even though we have had a vaccine for rubella for decades, the disease is still a lingering threat, even in the United States For several decades, it was considered to have been eradicated in this country – but it comes back periodically. Most often, outbreaks in the U.S. occur in places of large populations that exist in close quarters, such as college campuses, prisons, and boarding schools, as well as close-knit neighborhoods like Amish communities where many people are not vaccinated.
One of the dreaded "childhood diseases", rubella can also attack adults. When I was a child there was no rubella vaccine. After the MMR (measles, mumps, rubella) vaccine became available, outbreaks of those diseases in this country became so infrequent that people stopped worrying about them -- even stopped thinking about them. This highly contagious disease, rubella, is still out there. It can still cause deafness, blindness, stillbirths, infertility, and other congenital birth defects.
While these diseases once seemed to re-emerge each spring, now they seem to emerge in crowded populations at random. Every year, as spring arrives, we should watch for symptoms, especially on the campuses of colleges, universities, and boarding schools.
Mom as Caregiver

Are Vaccines Effective?
As a master's level public health educator, I can tell you there is no vaccine that is 100% effective. A vaccine that has at or above 80% efficacy is considered to be very good. More than that is great.
Remember, vaccines take two weeks to take full effect, so you are exposed during that two-week timeframe, you may become ill.
Because, again, no vaccine is 100% effective, it is unfortunately possible you could still become infected. However, if you do get sick after taking a vaccine, you will have a far milder case of whatever disease the vaccine was meant to stop.
Boomers Remember the Fear and Hysteria
Until COVID-19 came along, many people of generations younger than Baby Boomers had no memory of, or experience with the fear, even outright hysteria, that once surrounded childhood diseases. During the time I was a child, the general population seemed to think of chicken pox as little more than a nuisance, but everyone feared measles, mumps, and polio. What we didn't know at that time, is that chicken pox (varicella-zoster virus), leaves people with a susceptibility to shingles, an extremely painful, stress-induced disease of adulthood.
Did You Have Any of the "Childhood Diseases"?
Did you suffer from childhood diseases, and if so, was it
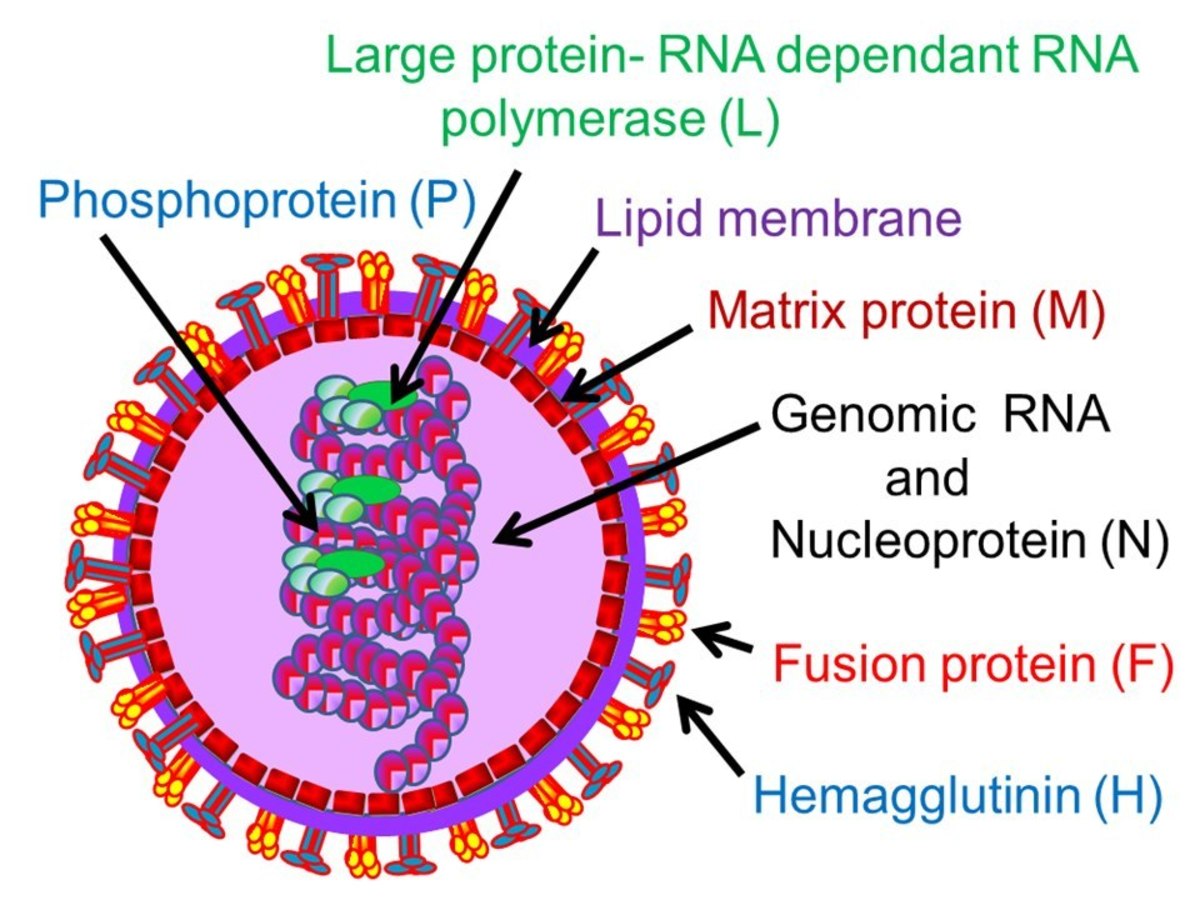
Zoomed in On an Evil Virus

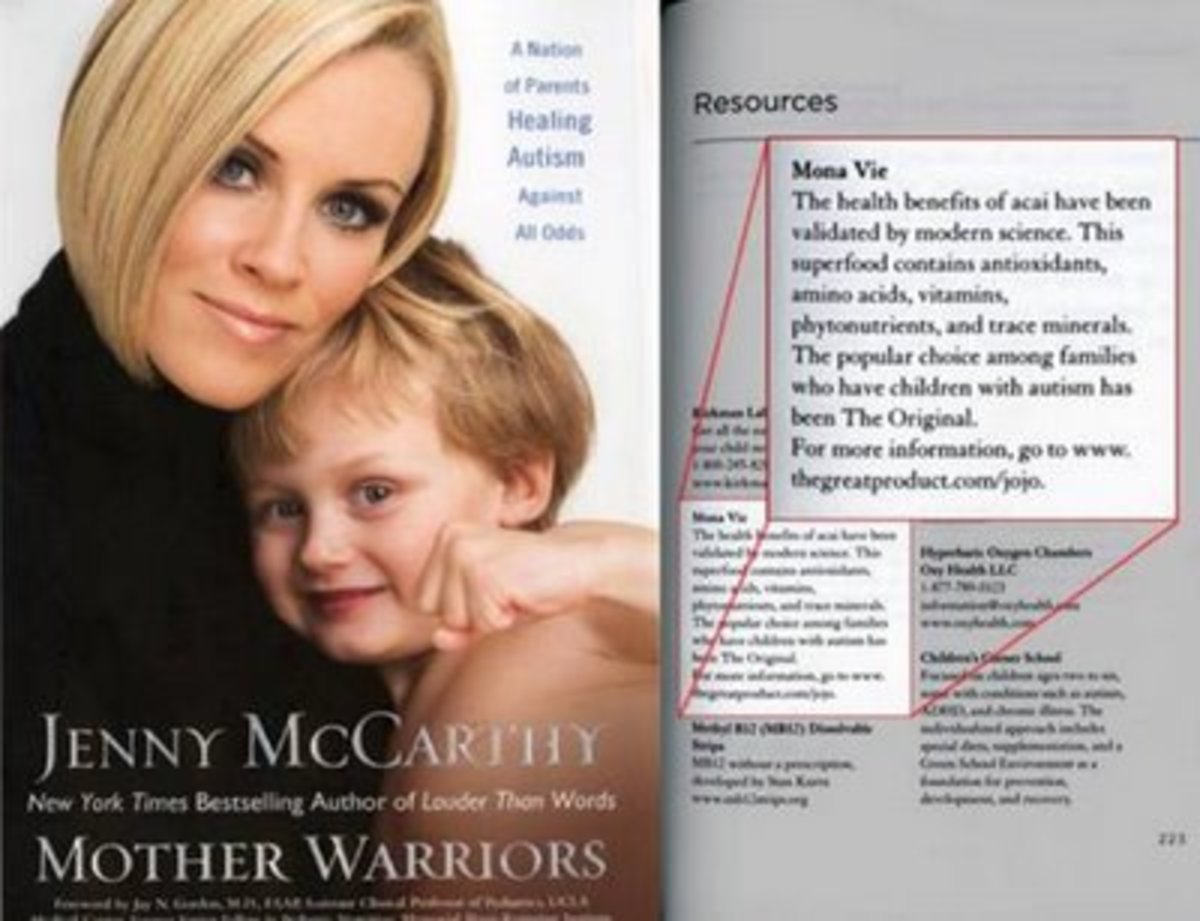
While it is not possible to prove a negative, there is absolutely NO legitimate clinical research that indicates any link between vaccines and autism or any other similar problems.
How It Spreads
Humans are the only known host for the rubella virus. As it moves from person to person, it takes an aerosol route (droplets from sneezes, coughs, etc.), which is the reason it flourishes in close-quartered populations such as classrooms, college dormitories, and prisons. The initial site of infection is the respiratory tract, one reason its symptoms can often be mistaken for the flu.
People Travel Here
Rubella can be brought into this, or any, country by unvaccinated visitors from other countries. This is what happened in a 1996-97 outbreak where most of the cases (83.3%) were in North Carolina. That outbreak was traced back to a child from another country who visited a popular theme park in Florida, then traveled to North Carolina to visit relatives, all the time not knowing he was infected.
We Travel There
It can also be brought here by unvaccinated American tourists and business travelers who visit other countries where the spread of rubella has not been controlled. They return here, also not knowing they have been infected. This seems to be what has happened with the most recent rubella outbreak.
Rubella Can Be a Relatively Mild Disease, But...
For children or adults, rubella is a fairly mild disease with flu-like symptoms, often accompanied by a rash. Approximately 50% of rubella cases have no symptoms, or such mild symptoms that the child or parents either don't notice it at all, or believe it is "just a cold". Rubella is often confused with rubeola (frequently called "the big red measles". There are usually no serious complications for a person with rubella, however, for the child of a pregnant woman, this disease can be devastating. I remember my fifth grade teacher had to have a therapeutic abortion because a lot of the kids at my school had rubella that year, and she contracted the disease from one of her students. Back then, they called it "taking the baby". She was devastated.
Thank Goodness for Modern Medical Technology

Modern Diagnostic Methods
Diagnostic methods such as ultrasound and amniocentesis, came into use in the 1970s and 1980s. Prior to that time, there was no way of knowing whether a fetus had been affected in utero after discovering its mother had been exposed to rubella. Because the disease had such devastating consequences for an unborn child, the standard procedure, at the time, was to "take the baby".
More than 80% of children whose mothers contract this disease during the first trimester of their pregnancies, have congenital defects such as deafness, heart defects, cataracts, psychomotor retardation and/or mental retardation, and many other life-threatening problems. My old instructors’ edition of the text that I used in teaching personal health (HEA-201) said it was 25%, but at some point, I had crossed that out and written in 80% due to learning of more current research of vaccine preventable infectious diseases. Either way, that is a lot of children with very serious congenital defects.
Memories of My Own Childhood Experiences
I remember community swimming pools being closed due to a fear of polio. My parents wouldn't let me read or watch TV when I had measles for fear it would "settle in my eyes" and cause blindness. I missed 30 consecutive days of the first grade because I had scarlet fever, rubeola, and chicken pox consecutively. I'm sure it was a challenge for my mom to keep me occupied, and to keep me from driving her nuts, because, along with feeling bad, I was bored to tears. During that time, she sat on my bed and taught me to tie my shoes, and to tell time with a clock she made out of a paper plate. She also read to me a lot.
I had mumps without knowing it, probably during that time. It was discovered when an employer required that I have a rubella titer drawn as a condition of employment. Because of that test, I learned I had had rubeola, but not rubella. Another surprise was that I had very high levels of mumps antibodies! So, when I had the opportunity to work with a local physician in Greensboro, NC, on a project to raise awareness of the still-lingering dangers of rubella, I joined the effort, and made it my own special research for my master's thesis.
Incubation & Contagion Periods and Signs & Symptoms
Incubation and Contagion Periods
The rubella virus replicates in the lymph nodes and epithelium, then spreads to other tissues. About half of cases (50%) will have no rash, but if a rash occurs, it usually begins about 2 weeks after the initial infection, but can be anywhere between 12 and 23 days afterward. The person with rubella is infectious (contagious) beginning about a week before onset of the rash, and continues to be infectious for about 2 weeks.
Signs and Symptoms
As stated above, about 50% of rubella cases have no symptoms, and a person can have the disease without ever knowing it — as I did with mumps. Symptoms include low grade fever, sore throat, and a rash that first appears on the face, then spreads to the rest of the body.
Fetus In Utero

A Child Infected During Pregnancy Can Be Contagious for Up to a Year After Birth
These children have what is called congenital infection syndrome. The virus from congenital infections will persist after birth, meaning these children can infect others after birth for a year or more. The virus is present in naso-pharyngeal (nasal) secretions, feces, and urine.
People with congenital rubella syndrome may develop additional complications later in life. These can include thyroid dysfunction, growth hormone deficiency, and visual complications. About 20% will develop diabetes.
One extremely rare complication of rubella is progressive rubella panencephalitis. It is a very slow viral disease that usually develops in the teens. Death usually occurs within 8 years. Most often it is associated with congenital rubella, but it can be associated with childhood rubella.
Have you had your children vaccinated?
Doing the Research
My master’s thesis was about rubella prevention and education during 1997, the second of two consecutive years in which North Carolina experienced a rubella outbreak. At that time 83.3% of the cases in the U.S. were in a few counties in North Carolina. The CDC and WHO (World Health Organization) became involved and traced the index case as described above.
My research was conducted in 10 private practice OB/GYN offices in Greensboro, North Carolina. My primary goal was to get those medical offices to make it a condition of employment that everyone in the offices show proof of immunity to rubella, or be immunized against rubella. Medical records quoting a diagnosis of rubella was, and is, not good enough. Proof is defined as a record of receiving the MMR vaccine, or a lab report showing rubella antibodies.
All of the medical offices agreed to make it a condition of employment for their employees. The problem was that the physicians did not consider themselves to be employees. One of those physicians, a middle-aged white male, was found not to be immune to rubella, but he refused to be immunized. He said he didn’t like needles, and that it was not necessary. This man was an OB doc, with direct and daily contact with pregnant women! I sincerely hope his colleagues convinced him to be a big boy and take the vaccine.
Are You Immune to Rubella?
Can you prove your immunity to rubella by records of antibodies or of vaccine?
Outdated Beliefs About Diseases Still Exist

Old Wives' Tales
There are many erroneous beliefs about what we have called “childhood diseases”. One of these is that, if a person had mumps on only one side, that person can still get them on the other side. This is false. Often, people will have the swelling that accompanies mumps on only one side of their faces, leading many to believe they could still have the swelling on the other side. Those folks would say something like, “I’ve had the mumps on one side, but not the other”.
As with any virus, the mumps virus enters the bloodstream, and is carried throughout the body. So, either you’ve had mumps, or you’ve not. Many people have no swelling of the face at all, leading them to believe they never had mumps. As mentioned above, I was one of those people.
Prevention and Treatment
Prevention
A live vaccine, consisting of an attenuated (weakened) strain is available. The virus used in producing this vaccine is grown in human diploid fibroblasts (blood cells). Because there is only one serotype, one dose of this vaccine provides lifelong protection. The vaccine cannot cause the attenuated virus to spread to others.
It is very important that women are vaccinated before their first pregnancy. The U.S. Public Health Service recommends all people be vaccinated in childhood, and that all disease-susceptible adolescents and non-pregnant adults also be vaccinated. Any pregnant woman who is found to be seronegative (non-immune) should be watched carefully by her obstetrician, and be vaccinated after giving birth.
While it is not possible to prove a negative, there is absolutely NO legitimate clinical research that indicates any link between vaccines and autism or any other similar problems.
Treatment
There is no cure for rubella. Prevention is the primary course to take.
About the Author
I hold a master's in public health from the University of North Carolina at Greensboro (UNCG) and a bachelor's degree in psychology from the University of Alabama at Birmingham (UAB).
At UNCG, my concentration of studies was cardiovascular disease (CVD) prevention and epidemiology. Because there was a local physician willing to pay me to do the research and statistical data analysis for his pet project, rubella awareness and prevention, I accepted this departure from CVD, and used his "baby" as my thesis research. I went on to be a part-time instructor at UNCG until grant funding ran out, then director of Community Partnership for Dental Health, a public health dental clinic, also in North Carolina. That was another deviation from CVD, but that is just one of many good things about careers in public health. It offers a huge array of career opportunities.
This content is accurate and true to the best of the author’s knowledge and is not meant to substitute for formal and individualized advice from a qualified professional.
© 2014 MariaMontgomery