Soteria: Loren Mosher's Soteria approach as an alternative intervention for acute psychosis
Introduction
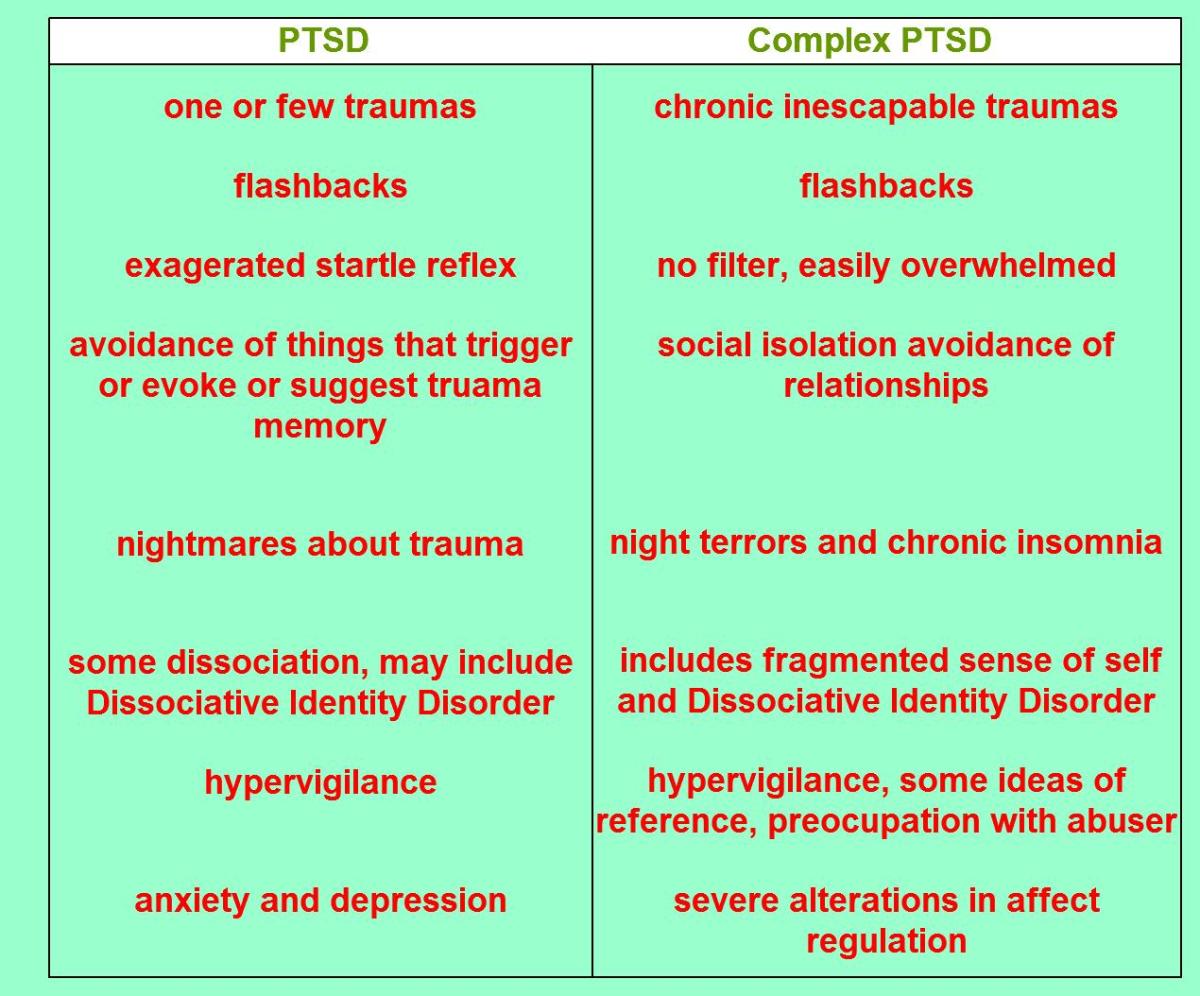
The Soteria project, a radical approach to the treatment of severely distressed people with a diagnosis of “schizophrenia”, opened its doors over 40 years ago (1). The brainchild of dissident American psychiatrist, Loren Mosher, the Soteria approach demonstrated that small crisis-support houses staffed by non-professionals achieved outcomes that were at least as good as the traditional acute psychiatric hospital treatment. Furthermore, the Soteria initiative involved only minimal use of medication, in contrast to the conventional hospital intervention that relied heavily on toxic antipsychotic drugs.
Remarkably, despite costing significantly less (in both economic and physical health terms) than the psychiatric hospital-medication approach, Soteria lost funding and was forced to close its doors 11 years after its instigation, an outcome that bears testimony to the power of the vested interests of both traditional psychiatry and the pharmaceutical industry.

Soteria House: details of the project
In 1972, in an impoverished area of downtown California, Soteria House welcomed its first six residents, each recruited from the Emergency Rooms of local hospitals where they had presented in acute crisis, suffering some combination of voice hearing and paranoia (a mental state described as a psychotic episode and one which typically attracts a diagnostic label of schizophrenia). Rather than psychiatric professionals, Soteria House utilized unqualified staff who were chosen for their personal qualities, such as a respectful manner and a tolerance of differences.
The staff lived with the residents and strived to create a homely, non-intrusive environment to enable the inmates to make sense of their psychotic experiences. In Mosher’s own words: “… staff worked gently to build bridges, over time, between individuals’ emotionally disorganized states to the life events that seemed to have precipitated their psychological disintegration” (1). A positive expectation of recovery permeated the project.
Soteria is a Greek word for “deliverance”, a title that captures the sense of rescuing people from both their emotional turmoil and exposure to conventional psychiatric practices. In stark contrast to the traditional psychiatric approach, no medication was used in the first six weeks of residence (except for emergencies).

Soteria approach: evaluation
Loren Mosher possessed research expertise and vigorously evaluated his innovative approach (1). He directly compared the outcomes for people involved in Soteria with those of patients in receipt of traditional psychiatric treatment (comprising an inpatient psychiatric hospital stay, regular antipsychotic medication and routine contact with psychiatric experts).
The results of the evaluation were astonishing. The benefits for the Soteria residents within their first few weeks of stay, with regards to psychotic symptoms such as voice hearing and paranoia, were comparable to those achieved by patients following the traditional route. At 2-years follow up, the Soteria group were progressing at least as well as those receiving conventional treatment, with even a suggestion of modest superiority; the Soteria participants achieved greater success in the job market and were living more independently.
The average length of stay at Soteria House was five months, although most were much improved after the initial, drug-free, six weeks.
A recent, comprehensive evaluation of the Soteria approach (2) (incorporating the original project and subsequent replications) confirmed the success of this compassionate, minimal-drug alternative to traditional psychiatry. Importantly, Mosher and colleagues provided convincing evidence that around 40% of psychosis sufferers can improve without any medication at all (3)(4).
Loren Mosher discusses Soteria
Loren Mosher: a brief biography
As a young man, Mosher worked in the oil fields of the American West to fund his entry into medical school at the prestigious Harvard University. He qualified as a doctor in 1961 and pursued further training in psychiatry. His career subsequently progressed at a precipitous rate. As a researcher he was a prolific contributor to scientific journals. In 1968 he became the first chief of the National Institute for Mental Health (NIMH) Center for Studies of Schizophrenia, a post he held for 12 years. In addition, he founded and edited the Schizophrenia Bulletin, a scholarly, high-profile journal for schizophrenia research. As a clinician, he specialized in helping troubled adolescents and their families.
Mosher’s compassionate, humanising approach to people with mental health problems, with its emphasis on trying to understand psychotic experiences rather than striving to tranquillize them away with antipsychotic drugs, soon brought him into conflict with the mainstay of the psychiatric profession. Marginalized by his peers at NIMH, Mosher experienced increasing alienation from the traditional psychiatric arena with its obsessive search for brain diseases and illusory chemical cures.
After 35 years as a member of the American Psychiatric Association (APA), he resigned in 1998 via a public letter in which he condemned the organisation for having been “almost completely bought out by the drug companies”. Further criticism targeted the APA’s neglect of the social context and the fixation on brain biochemistry: “… we are there to realign our patients’ neurotransmitters. The problem is that it is very difficult to have a relationship with a neurotransmitter – whatever its configuration.” His resignation letter also denounced his profession’s misuse of power: “I want no part of a psychiatry of oppression and social control” (5).
Sadly, this principled and compassionate innovator died of liver cancer on July 10th 2004, aged 70.
Replications of Soteria
Three years after the opening of Soteria House, Mosher developed another facility (referred to as “Emanon”) based on the same philosophy, and achieving the same impressive results. In 1984, a similar project, employing a slightly modified version of Soteria, was developed in Berne (Switzerland) (6).
Houses based on the Soteria philosophy can currently be found in Sweden, Finland, Switzerland, Germany and Hungary. An organization named “Soteria – Brighton” formed in 2011 with the primary aim of establishing the approach in the United Kingdom.
Why has the Soteria approach been ignored?
Despite its effectiveness, acceptability to service users, and relatively low cost, the Soteria project endured hostility from mainstream psychiatry and the drug industry. Traditional psychiatrists, wedded to the idea that schizophrenia is a brain disease, challenged the validity of the Soteria findings, despite Mosher’s meticulous approach to evaluation. As a result of insufficient funding, the original Soteria House was forced to close its doors in 1983.
Notwithstanding the innovative replications (outlined above), the Soteria approach to psychosis has been disregarded by western psychiatry. Mosher himself offered an explanation for this curious state of affairs whereby “Soteria disappeared from the consciousness of American society” (1). To traditional psychiatrists, Soteria’s fundamental flaws were associated with its relative disregard of the cornerstones of psychiatric ideology, namely: antipsychotic medication (or “neuroleptics” as they were then called), prominent medical input, inpatient psychiatric hospitals and professionally-led services. As such, it presented (and continues to present) a threat to established psychiatric practice and the vested interests therein.
Regrettably, a decade on since Mosher’s death, little has changed, the “medicate and hospitalize” approach continuing to dominate the psychiatric landscape, a stark example of dogma triumphing over reason.
References
1. Mosher, L. (1999). Soteria and other alternatives to acute psychiatric hospitalization: A personal and professional review. Journal of Nervous and Mental Disease, 187, 142 – 49. Retrieved 25 March 2014 from, http://www.moshersoteria.com/articles/soteria-and-other-alternatives-to-acute-psychiatric-hospitalization/
2. Calton, T., Ferriter, M., Huband, N. & Spandler, H. (2008). A systematic review of the Soteria paradigm for the treatment of people diagnosed with schizophrenia. Schizophrenia Bulletin, 34, 181 – 192
3. Bola, J.R. & Mosher, L. (2002). Predicting drug-free treatment response in acute psychosis from the Soteria project. Schizophrenia Bulletin, 28, 559 – 75.
4. Bola, J.R., Lehtinen, K., Aaltonen, J., Rakkolainen, V., Syvalahti, E. & Lehtinen, V. (2006). Predicting medication-free treatment responders in acute psychosis: cross-validation from the Finnish-need adapted project. Journal of Nervous and Mental Disease, 194, 732 – 39.
5. See www.moshersoteria.com for full resignation letter
6. Ciompi, L., Dauwalder, H.P. & Maier, C. (1992). The pilot project ‘Soteria Berne’. Clinical experiences and results. British Journal of Psychiatry, 161, 145 – 153.