What Is Chronic Obstructive Pulmonary Disease (COPD)?
What exactly is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a lung disease in which the lungs are damaged, making it hard to breathe. In COPD the airways are partly obstructed. Causes of COPD are smoking and other lung irritants such as pollution, dust or chemicals over an extended period of time.
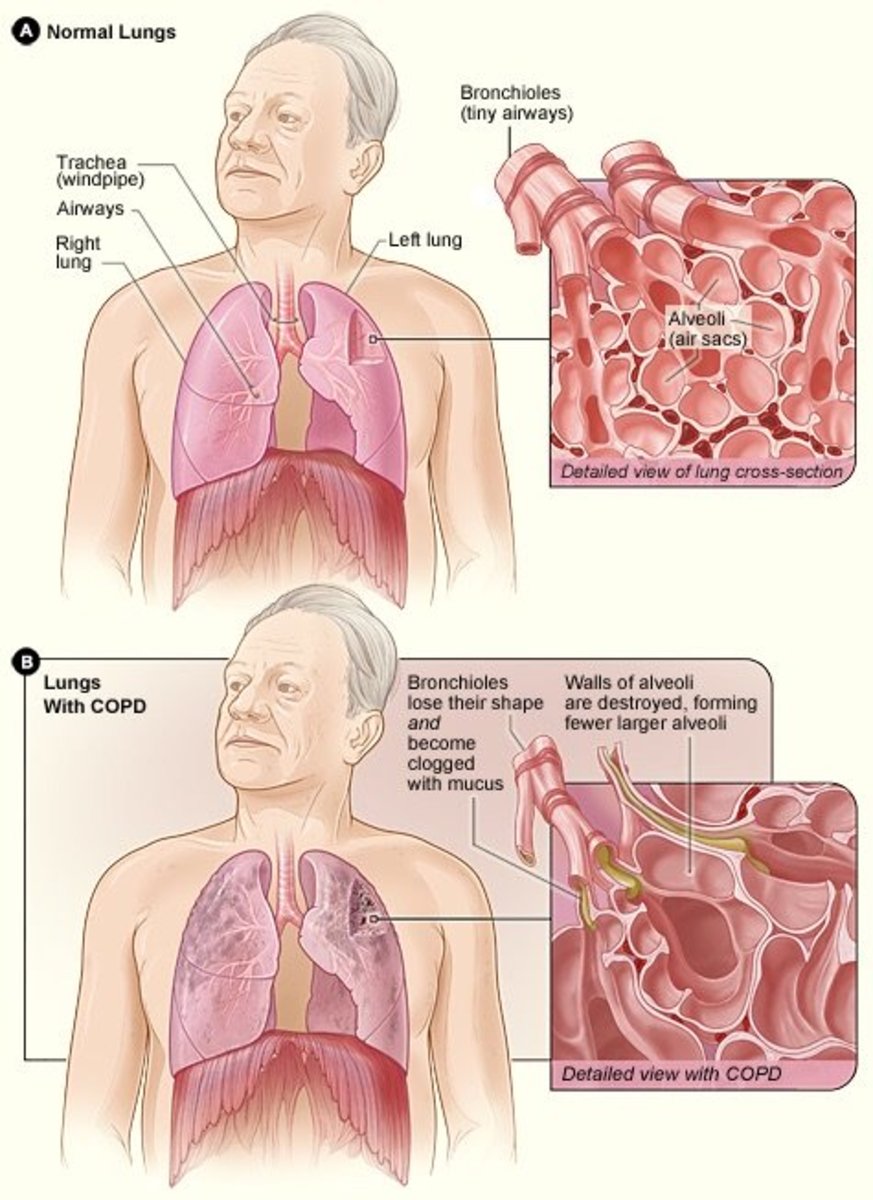
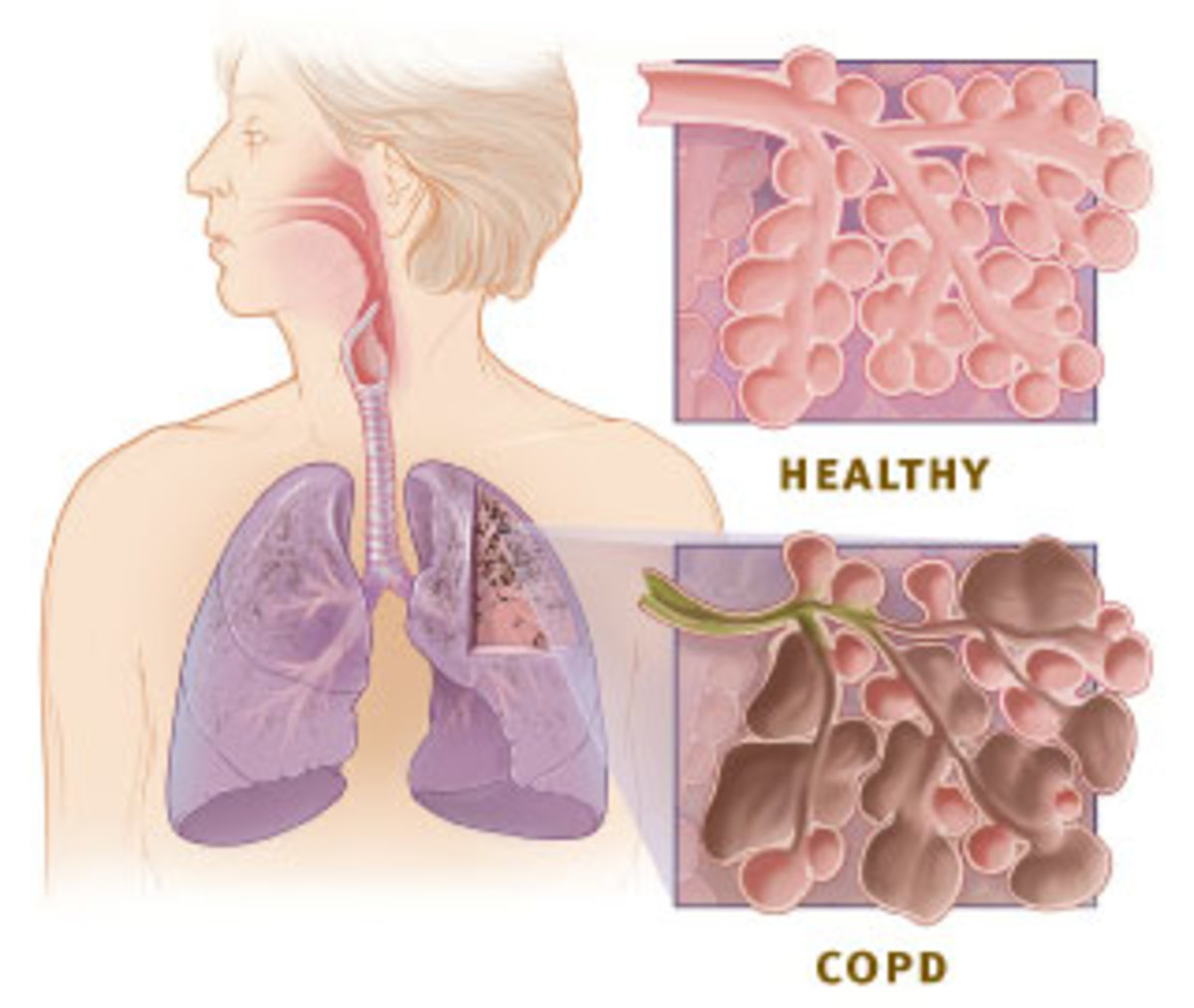
In healthy lungs, each airway is clear and open. The air sacs are small and dainty. Both the airways and air sacs are elastic and springy. When you breathe in, each air sac fills up with air like a small balloon. When you breathe out, the balloons deflate and the air goes out.
With COPD, the airways and air sacs lose their shape and become floppy. Less air gets in and less air goes out due to the following reasons:
- the airways and sacs lose their elasticity
- the walls between many of the air sacs are destroyed
- the walls of the airways become thick and inflamed
- cells in the airways make more mucus than usual, which tends to clog the airways
COPD developes slowley and it may be many years before you notice symptoms, such as feeling short of breath. Most of the time, COPD is diagnosed in middle-aged or older people.
COPD is a major cause of death and illness and is the fourth leading cause of death in the U.S. and throughout the world.
Signs and Symptoms
Symptoms of COPD may include:
- persistent cough
- sputum (mucus) production
- wheezing (a whistling or squeaky sound when you breathe)
- chest tightness
Cough that doesn't go away and coughing up lots of mucus are common signs of COPD. These often occur years before air flow through the lungs are reduced. However, not everyone who has COPD has a cough.
Severity of symptoms will depend on the amount of lung that has been destroyed. There is no cure for COPD. The damage to the lungs can not be reversed. However, there are treatments to help you feel better and slow the damage. COPD is not contagious nor is it a hereditary disease.

Diagnosis
Your doctor will use a breathing testing maching called a spirometer to confirm a diagnosis of COPD. The test is easy and painless. You will breathe hard into a large hose connected to the spirometer. When you breathe out, it measures how much air your lungs can hold and how fast you can blow the air out of your lungs.
Spirometer is the most sensitive and most commonly used test of lung functions. It is capable of detecting COPD long before you have significant symptoms. This test will help the doctor determine the severity of COPD when diagnosed by these classifications:
- At risk (for developing COPD) Breathing test is normal but patient exhibits mild signs, including a chronic cough and sputum production.
- Mild COPD Test shows mild airflow limitation. Signs may include chronic cough and sputum production. At this stage, you may be aware of airflow reduction.
- Moderate COPD Test shows a worsening airflow obstruction. By this stage, signs have increased. Shortness of breath occurs when working, walking fast or other brisk tasks.
- Severe COPD Test will show severe airflow obstruction. Shortness of breath occurs after small amounts of activity. In very severe COPD, complications may develope such as respiratory failure or signs of heart failure. At this stage, quality of life is greatly impaired and worsening symptoms may be life threatening.
In severe cases, doctors may regularly run a test called arterial blood gas (ABG), which is a blood test that measures the oxegen level in the blood. This test helps determine if oxygen treatment is necessary.
Treatment
The goals of COPD treatment are to
- relieve your symptoms with minimal to no side effects of the treatment
- slow the progress of the disease
- improve your ability to stay active
- prevent and treat complications and sudden onset of problems
- improve overall health
Your doctor may recommend medications called bronchodilators that work by relaxing the muscles around the airways. Bronchodilators can be either short-acting or long-acting. The short-acting bronchodilators last about 4 to 6 hours and are only used as needed. The long-lasting bronchodilators last about 12 hours or more and are used every day. Most bronchodilators are inhaled so they go directly into the lungs.
If you have mild COPD your doctor may recommend using a short-acting bronchodilator. If you have moderate to severe COPD he may recommend regular treatment with one or more bronchodilator. Some patients may need to use one short-acting and one long-acting bronchodilator. This is called combination therapy.

Inhaled Glucocorticosteroids (steroids)
Inhaled Glucocorticosteroids (steroids) are used for some patients with moderate to severe COPD. Inhaled steroids work to reduce airway inflammation. They are also useful in helping to strengthen the lungs.

Flu Shots
The flu (influenza) can cause serious problems in patients with COPD. Flu shots can reduce the chance of getting the flu.

Pneumococcal Vaccine
The Pneumococcal vaccine should be recommended to patients with COPD to prevent a common cause of pneumonia. Revaccination after 5 years may be necessary for patients over 65 years of age.
Pulmonary Rehabilitation (rehab)
Pulmonary Rehabilitation is a coordination of exercise, disease management training and counciling. What is included in your rehab program will be determined by you and your doctor.

Oxygen Treatment
If you have severe COPD and low oxygen levels in the blood, your physician may recommend oxygen therapy. You may need extra oxygen some of the time or all of the time. For cases of severe COPD, using extra oxygen for more than 15 hours a day may be necessary to help the patient
- do tasks or activities with less shortness of breath
- protect the heart and other organs from damage
- sleep more during the night and improve alertness during the day

Surgery
For some patients with severe COPD, surgery may be recommended. There are three types of surgery that are considered for patients with severe COPD.
- Bullectomy: In this procedure, surgeons remove one or more very large bullae from the lungs of people who have COPD (emphysema). Bullaes are air spaces that formed when the walls of the air sacs break. The air spaces can become so large that they interfere with breathing.
- Lung Volume Reduction surgery (LVRS): In this procedure, surgeons remove sections of the damaged tissue of the lungs in patients with COPD (emphysema).
- Lung Transplant: A lung transplant involves removing the lung of a person with COPD (emphysema) and replacing it with a healthy lung from a donor.
Dolly Corrine Noah November 2007

Living with COPD
While COPD is a very serious lung disease, with proper treatment, healthy diet and excercise, you can live a long and productive life. Both my parents had this disease. My Dad, who passed away in 1998 had this disease for about 30 years before his death. My Mom also has had COPD for 34 years. She will be 73 this year and while she has just been released after a short hospital stay to increase her oxygen level in her blood, she is still fairly active today. She is on permanent oxygen but has a portable tank that she can take with her when she goes out, she takes breathing treatments, which she also has a portable machine for traveling and she is on daily medications. While she may not be able to kick her nose anymore, she is still the backbone of our family and a very strong-willed lady.
If you are diagnosed with COPD, follow your doctors treatment advice and work diligently to maintain an active, healthy lifestyle.