Pandemic Sheds Light on Failing U.S. Prison System

Since the beginning of the coronavirus pandemic, the US has seen a significant drop in the number of people behind bars in state and federal prisons. Between March and June, more than 100,000 inmates were released, a decrease of 8% of the total prison population.
According to data from the Marshall Project, prison head counts have decreased due to the fact that prisons have stopped accepting new prisoners from county jails to avoid importing the virus. Many courts across the nation are closed due to the pandemic, meaning fewer people received sentences, and parole officers stopped sending people back to prison for lower-level violations. Professor of Criminal Justice Martin Horn believes the pandemic has slowed down the entire criminal justice system, causing fewer people to go to prison in general. Across the US, more than 57,000 prisoners have reportedly tested positive for the coronavirus, including 34,000 recovered and 651 deaths.
The early release of so many prisoners comes at an interesting time considering nationwide protests against systemic racism (police brutality and a faulty prison system are key contributors to systemic racism in the US). The head count for July could rise again as many states enter into various phases of reopening. Whether prisoner populations rise when states reopen depends heavily on how these early releases are perceived by the public. If the public perceives a safety threat from people released early due to the pandemic, it is likely to affect the larger movement to reform US prisons.
Wanda Bertram of the Prison Policy Initiative explains how public perception could affect the movement in an interview with The Guardian. Bertram says if people leaving prison end up homeless, for example, they might be arrested for petty and/or nonviolent crimes like sleeping on the street, then the public may associate these early releases with increased crime.
Some proponents of criminal justice reform believe that the nationwide decreases in prison population is a step in the right direction. However, the numbers are disappointing considering the high risk that prisoners have of contracting coronavirus in prison conditions. It can be argued that prisons aren’t necessarily releasing the right prisoners, either.
For example, Stephanie Parris was just at the end of a two-year sentence for a probation violation when she was told that she’d be released early due to the pandemic. Parris says she felt bad leaving when she had only three weeks left – she wasn’t sick and there were no reported cases inside the prison. There were others inside at a higher risk, whose early release could mean life or death – “I would have helped someone who had nine or 10 months, someone who absolutely needed it…there was a lady in there who was very elderly and has bad health problems. I would have given my place to her,” says Parris.
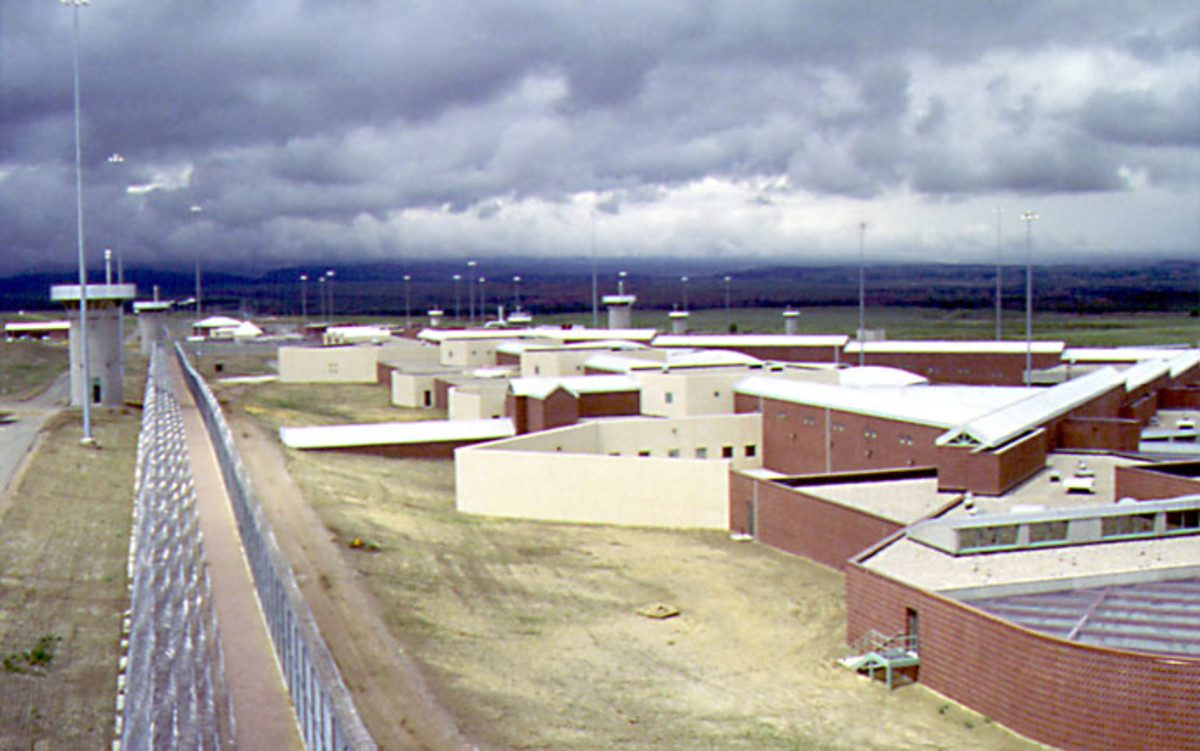
A recent case occurring at Butner federal prison suggests the number of prisoner infections and deaths may be incorrectly reported, and is in fact much higher. The coronavirus outbreak has been deadliest at the Butner complex near Durham, North Carolina, where 25 prisoners have died from coronavirus, plus one staff death, the most of any federal prison in the US.
On May 20, Alan Hurwitz was released from federal prison after being convicted of bank robbery over a decade earlier. Hurwitz is 79 years old and at a high risk of contracting COVID-19. The prison failed to test Hurwitz for COVID-19 and he carried it with him onto the plane home. Releasing incarcerated people without testing them, and a lack of access to basic medical care for many former prisoners has exposed countless people on the outside.
Hurwitz’s story highlights systemic problems in the prison system’s response to the coronavirus pandemic. Prison officials at Butner were admittedly slow to test for the virus, and enabled potentially infected inmates to spread it in tiny dorms where there is no possibility of social distancing. Some prisoners reported in sworn affidavits, that they were not tested for six weeks or more, even as their fellow inmates fell ill and died. Correctional officers and other workers in Butner transmitted the virus throughout the prison and carried it outside prison walls as well.
Despite being ordered by the US Attorney General to send the most medically vulnerable prisoners home, Butner was very slow to release them. Despite having a hospital and four prisons filled with thousands of vulnerable inmates, Butner released fewer than 50 out of the 4,700 people incarcerated there (that’s less than 1%). Former inmate Dan Johnson, who served one year at Butner for misusing a government credit card, says that “if a local jail did the things they do at Butner, federal officials would come and lock people up.”
Few prisons have been able to establish appropriate social distancing requirements, which is proven to be the most effective tool against coronavirus. Dr. Jody Rich, an infectious disease specialist, notes that “we shut down the whole economy to physically distance people, but you can’t do it in this confined setting, so you have to reduce the census.” Older prisoners generally have the most health problems and are the most vulnerable, so prisoner advocates argue that they should be among the first released.
Alan Hurwitz, who had suffered six heart attacks and four bouts of cancer, was so frail that he required an “inmate companion” to help him with general hygiene and getting around in his wheelchair. Hurwitz’s declining health and clean disciplinary record made him a strong candidate for finishing out his sentence at home. However, his criminal record continued to hold him back – Hurwitz had been convicted of two strings of bank robberies between 1990 and 2009. Although bank robbery is a violent crime, Hurwitz presents no danger to the community.
On April 3, the day after Alan Hurwitz applied for release, Attorney General William Barr issued a second order directing prisons to “immediately maximize” the transfer of people from prisons with outbreaks to home confinement. But it was too late for Butner, the first prisoner died there on April 9, and the next day officials reported 58 cases among prisoners and 22 among staff members.
In response, prison officials reopened an unused building formerly used for solitary confinement. Butner used the two-person cells to quarantine newly arrived prisoners and those who tested positive for the virus. These prisoners received reduced rations and were subject to extreme temperature conditions, causing some infected inmates to hide their symptoms in order to avoid being seemingly punished for having the coronavirus.
A month after Hurwitz applied for release, Warden Tamara Lyn sent him back a form letter denying the request, stating “Your concern about being potentially exposed to, or possibly contracting, COVID-10 does not currently warrant an early release from your sentence.” Rather than appealing the decision, Hurwitz took his case to federal court and won. On May 20, the day Hurwitz was released from prison, he suffered chest pains and a 104 degree fever on his plane home. He was taken to a nearby hospital where he spent the next five days sharing video chats with his family, including his children and grandchildren, before he peacefully passed away.
Hurwitz case shows how the prison system has failed to protect its inmate from coronavirus, as well as protecting communities from the preventable spread of the disease. It is important to note that the Bureau of Prisons does not count Hurwitz as one on Butner’s dead due to coronavirus.