Antibiotics 101: A Glimpse into the History, Types, and Use of Antibiotics

In the movie Midnight in Paris, the main character travels to the 1920s Paris but decides not to stay and return to his own time for a number of reasons, one being because “these people don’t have any antibiotics.” It’s true, we haven’t always had antibiotics.
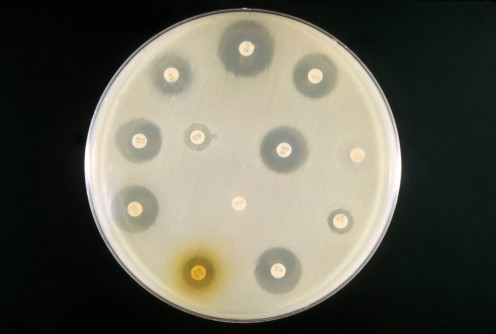
In fact, you could call the discovery of antibiotics a happy accident. Not meaning to, Alexander Fleming discovered the antibiotic penicillin in 1928.
After observing a fungus that developed on a culture plate of Staphylococcus Fleming saw that the fungus was effective in preventing Staphylococcus growth. This was soon tested and found to be highly successful. Thanks to this discovery, penicillin has become widely used to treat various infections.
So that’s how it was discovered, but what even are antibiotics and how do they work?
“Antibiotics are medicines that help stop infections caused by bacteria, according to WebMD. “They do this by killing the bacteria or by keeping them from copying themselves or reproducing.”
Without antibiotics many more people would die from infections like strep throat. Surgery also became safer with the use of antibiotics. Some common infections that are treated with antibiotics include ear and sinus infections, dental infections, skin infections, meningitis, strep throat, bladder and kidney infections, bacterial types of pneumonia, whooping cough, and STD’s.
Antibiotics aren’t a cure-all though. There are conditions antibiotics can’t treat because antibiotics only work against bacterial infections. Viral infections like colds, the flu, bronchitis, and stomach flu cannot be treated with antibiotics.
The nature of your infection isn’t always clear either, it may take some time for health professionals to distinguish if an infection is bacterial or viral.
Antibiotics are categorized into two groups: broad-spectrum and narrow-spectrum. Narrow-spectrum antibiotics only target certain bacteria, whereas broad-spectrum antibiotics combat various kinds.
As with any type of medication or treatment, there are often possible side-effects someone using them could experience.
Adam Felman of Medical News Today provides some side effects antibiotics can cause:
-
Diarrhea
-
Nausea
-
Vomiting
-
Rash
-
Upset stomach
-
Fungal infections of the mouth, digestive tract, and vagina
-
Kidney stones
-
Blood clotting
-
Sensitivity to sunlight
-
Blood disorders
-
Deafness
-
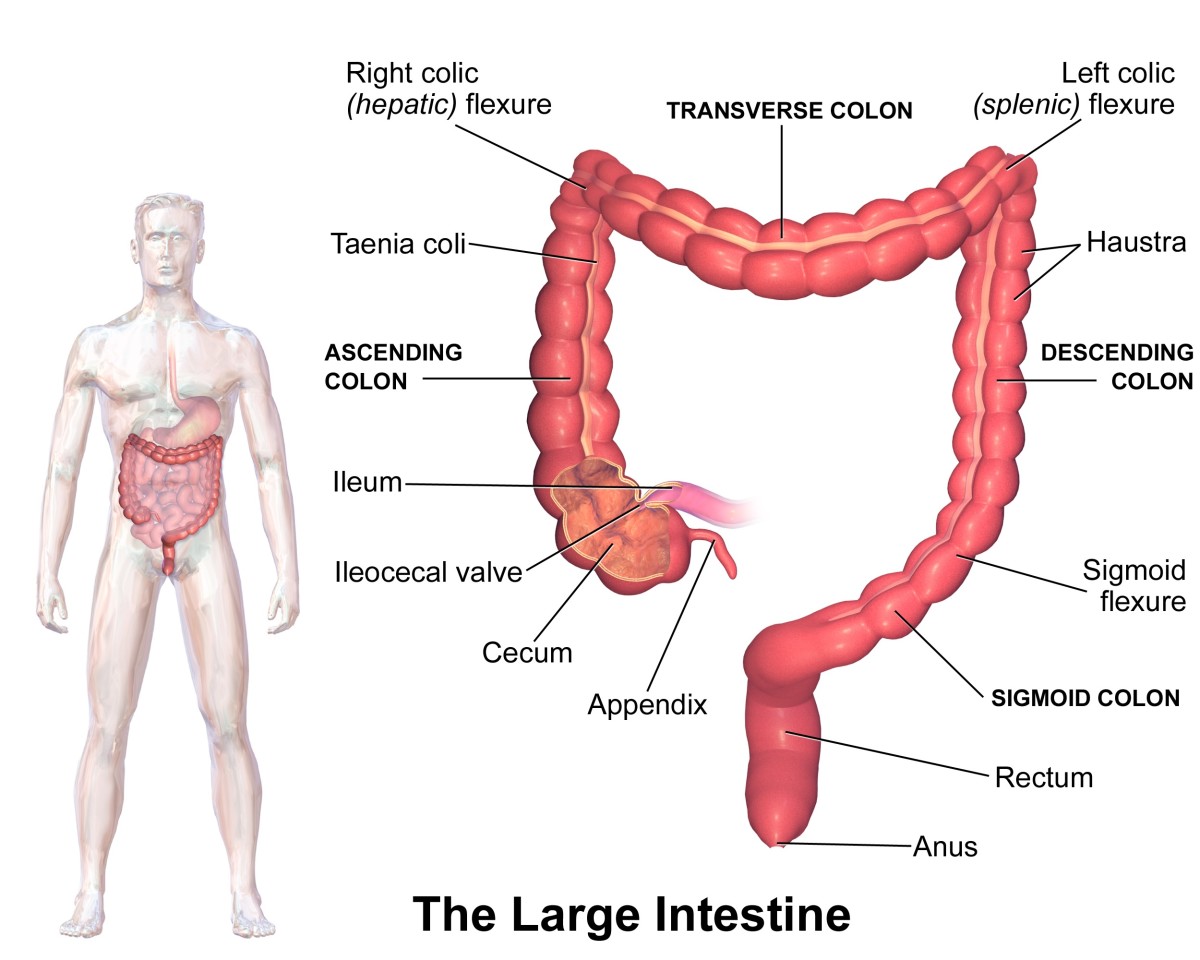
Bowel inflammation
Some of those are more common than others but all sound pretty unpleasant to me. Some of these symptoms may happen due to an allergic reaction. These can be serious so tell a doctor immediately if you experience one.
Antibiotics can have different instructions if you are prescribed some. Your doctor will often inform you how and when to take your antibiotics. One universal rule though is to take the whole course of medication. For instance, even if your infection goes away after three days of taking an antibiotic, take them the whole 10 days.
Types of Antibiotics
Drugs.com lists some common antibiotics such as amoxicillin, doxycycline, cephalexin, ciprofloxacin, clindamycin, metronidazole, azithromycin, sulfamethoxazole, trimethoprim, clavulanate, and levofloxacin. Antibiotics are usually sorted into classes or types.
Linda Crampton discusses the following types of antibiotics:
-
Beta-lactams
-
Macrolides
-
Quinolones
-
Tetracyclines
-
Aminoglycosides
-
Arylomycins
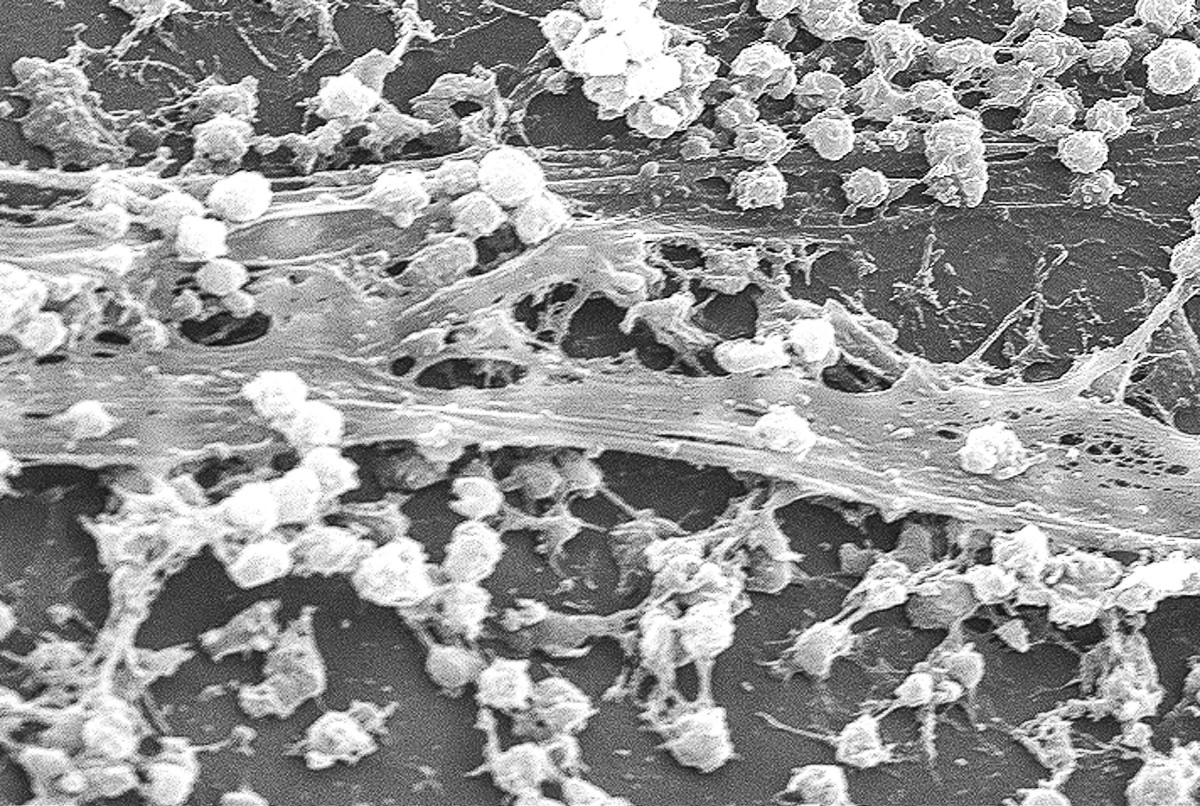
Antibiotics target bacteria either by preventing the reproduction of bacteria or by stopping mechanisms responsible for building cell walls Microbiology Society claims.
Crampton says that beta-lactams are broad-spectrum antibiotics like penicillin, ampicillin, and amoxicillin. This type binds to penicillin-binding proteins in order to stop amino acids from connecting chains that strengthen cell walls around bacterial cells.
Macrolides impede protein synthesis in bacteria which causes microbes to die, one common type of macrolide is erythromycin.
Quinolones are also known as fluoroquinolones such as ciprofloxacin. They kill bacteria by obstructing DNA gyrase or a specific enzyme. Each is involved in the process of DNA replication.
Tetracyclines come from soil bacteria originally but are partially synthetic. They kill bacteria that require oxygen to develop. They also hinder protein synthesis by attaching to bacteria’s ribosomes.
Aminoglycosides are narrow-spectrum antibiotics and combat bacteria by binding to a ribosome and impeding protein synthesis too. However, these can damage the kidney and ear as a side effect.
Unlike the other, arylomycins kill bacteria by sabotaging the structure and function of DNA or by interfering with folic acid synthesis. They do this by hindering a certain enzyme.
There are many different types of antibiotics and generic antibiotics within those types. If you are suffering from a bacterial infection, your doctor might use one to treat you. Antibiotics can be taken orally or administered intravenously or through an injection. However, some might work better than others depending on your history thanks to something called antibiotic resistance.


Antibiotic Resistance
According to the NHS, health organizations across the world have been trying to reduce the use of antibiotics because overuse causes them to become less effective. Some strains of bacteria have become resistant to antibiotics.
If antibiotics stop working, Microbiology Society says “modern medicine would be set back decades.”
For example, surgeries that wouldn't be otherwise would become dangerous to undergo because the risk of infection would rise such as blood poisoning.
WebMD provides that more than 150 million prescriptions are given in the United State for antibiotics and that 2 million infections are resistant to those antibiotics each year! No wonder bacteria is starting to adapt.
They say that bacteria can become resistant when their genes change or they revolve drug-resistant genes from other bacteria. In due time, we may need to look elsewhere for treatment. Antibiotic resistance is only making diseases more difficult to treat. And alternative drugs might take longer or cost more so it is important to not abuse the use of antibiotics.
The government has taken steps to resolve this issue with the National Action Plan. It consists of a five-year plan to reduce antibiotic resistance by doing three general things:
-
Innovating and researching prevention strategies
-
Improving surveillance
-
Adopting evidence-based stewardship strategies
It is a little hard to see how some of those things can help, but if it helps fight resistance then who am I to say.
According to SolvHealth, government sponsored antibiotic stewardship programs actually improve the use of antibiotics by educating medical facilities and their patients. They claim such programs can “optimize the treatment of infections and reduce adverse events associated with antibiotic use.” Programs do this by:
-
Increasing infection cure rates
-
Reducing treatment failure
-
Increasing the amount of accurate prescribing
None of this is to discourage you from using antibiotics, just be aware that it isn’t always necessary. You shouldn’t take them if your doctor says so or if you have a viral infection.
Antibiotic resistance explained (starting at 0:53 seconds)
Sources
This content is accurate and true to the best of the author’s knowledge and is not meant to substitute for formal and individualized advice from a qualified professional.
© 2020 Erin Day