Updates on BLS and ACLS
Whether you have taken CPR courses a thousand times, or are simply considering taking it because a family member has recently had an emergency, or you just want to be prepared, the skills learned in the BLS and ACLS courses are extremely valuable. There are a number of resources online that give the basics of CPR, but recently the American Heart Association (AHA) has made a number of important changes in an attempt to improve the quality of CPR and consequently improve outcomes. Information for this Hub was found using the Advanced Cardiovascular Life Support Provider Manual: Professional.
Disclaimer: These skills can be life saving and it is very important that they are taught by a professional who is trained in how to properly teach these techniques. This article is not meant to teach anyone the information and techniques needed to perform these skills. It is merely meant to provide an overview of what each protocol is and information regarding updates for those who may be re-certifying or looking into a CPR course.
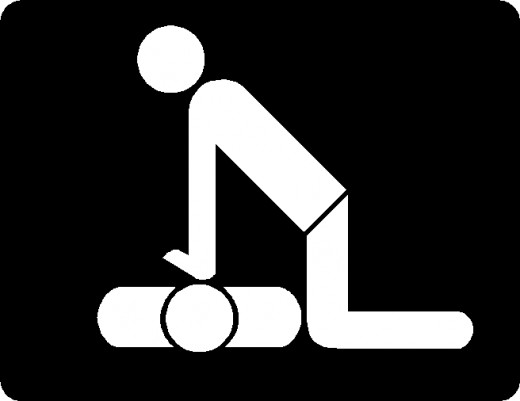
What are the Difference Between BLS and ACLS?
Basic Life Support (BLS) is intended to teach emergency responders of all levels the skills needed to recognize life-threatening situations and respond correctly by performing CPR, using an automated external defibrillator (AED), or relieving choking using various methods. The basic steps in the BLS survey include: checking level of responsiveness, activating the emergency response system, checking for a pulse and providing defibrillation if appropriate. BLS is typically provided prior to the patient reaching the hospital, and can be provided by almost anyone, including school teachers, day care providers, sports coaches, etc. Advanced Cardiac Life Support (ACLS) provides a more advanced response by further analyzing and properly treating emergency situations. It also differs from BLS in the range and invasiveness of resources available for the ACLS certified health professional to use. Healthcare professionals trained in ACLS must understand the use of assisted breathing devices, have the skill set to gain IV (or IO) access, and knowledge of appropriate pharmacologic therapies.
The Basics of BLS
BLS in based on a system of 4 steps designated 1-4. These 4 steps are always performed in the same sequence. First the responder checks responsiveness by loudly asking if the person is alright and scans the chest for any evidence of breathing by looking for movement. The second step in the BLS sequence is to make sure that proper help is called and that an AED is retrieved if available. It is important to be direct in asking bystanders to perform certain tasks. For example, instead of saying “someone call for help”, point to a particular person and say “You, go call 911 and you go retrieve an AED and bring it back”. A carotid pulse is then checked in the 3rd step and in the absence of a pulse, chest compressions are started immediately. The final step in the BLS process is the use of an AED to determine heart rhythm to decide is shock is advisable. Typically, BLS is continued until care can be passed off to individuals capable of higher, more intensive levels of care.
Links to More Detailed Information
- Red Cross CPR Certification
This Hub gave a lot of god information about getting CPR certified. - CPR
The American Heart Association provides information about CPR training and updates to the CPR protocol at their website. - BLS For Healthcare Providers
For more information about the specifics of CPR for various populations I found this Hub particularly useful.
Recent Updates to the BLS Protocol
- The AHA’s new model for successful resuscitation is represented by links within a chain. This chain, known as the Chain of Survival includes: recognition of the situation as cardiac arrest and activation of the emergency response system, early CPR that is high-quality and focuses on chest compressions, use of an AED rapidly if one is present to defibrillate shockable rhythms, effective ACLS, and proper care post cardiac arrest. These steps are those that were previously discussed in the Hub and were designated 1-4.
- Prior to 2010, the AHA’s model for resuscitation was represented by the pneumonic ABCD, which encompassed airway, breathing, circulation, and defibrillation. It is now recommended that chest compressions be started prior to giving any rescue breaths at a rate of at least 100 compressions/min at a depth of 2 inches and allowing the chest to recoil completely between each compression. This is a change from the prior recommended sequence of airway, breathing, circulation (ABCs) to circulation, airway, breathing (CAB). The emphasis is now placed on starting adequate chest compressions (as defined above) in a pulseless patient as early in the resuscitation process as possible.
- Providers no longer look, listen, and feel for breathing. Instead providers are instructed upon initial approach to the patient to scan the chest for any evidence of movement. It is important to remember that agonal gasps are not considered to be an effective breathing pattern.
- The AHA now places the continuous delivery of high quality CPR, with minimal breakage of compressions, at the forefront of CPR protocol. The new 2010 guidelines state stat stoppage of chest compressions for any reason (to check a pulse, apply AED pads, give rescue breaths in single responder CPR, etc.) should not exceed 10 seconds.
- Lastly, if more than one responder is present, responders should swith roles every 2 minutes (or 5 cycles of 30 chest compressions) to avoid fatigue and keep compression depth adequate at 2 inches.
The Basics of ACLS
ACLS lays out the proper treatment techniques for various emergency situations using a number of algorithms. Such emergency situations include: cardiac arrest, stroke, and cardiac rhythm disturbances. Unlike BLS, there isn’t a defined sequence of events, instead I think of it as one of those story books where the reader chooses the ending. The algorithms are like recipes, but the provider has to have enough training to put the right recipe with the correct patient and tools. If the provider is not properly trained, it would be like using a pizza recipe and a blender to make a cake! ACLS expands upon the foundations taught in basic CPR courses. Chest compressions and maintaining perfusion are the most important things, and without this foundation it doesn’t matter what drugs get thrown at a patient they are still doing to have a poor outcome.
ACLS Protocol Updates
- Waveform capnography is now used as the most reliable method of confirming and continuously monitoring placement of an Endotracheal (ET) tube.
- As of 2010, the use of cricoid pressure is not advised in maintaining a patient’s airway.
- Chest compressions should be continued while the defibrillator or AED is being prepared or charging, so as not to interrupt chest compressions any longer than necessary. As stated above, the maximum amount of time there should be a breakage in the chest compression cycle is 10 seconds.
- All advanced interventions, to include: obtaining IV access, placing an advanced airway, and giving medications should be performed around the cycle of chest compressions to keep chest compressions as continuous as possible. The AHA guidelines recommend performing such procedures during the brief pause in chest compressions that occurs immediately following defibrillation.
- Atropine is no longer recommended for use within the AHA’s PEA/asystole algorithm.
- The 2010 guidelines set new electrical parameters for the cardioversion of unstable patients. See table below.
- The AHA has deemed 5 things critical to the post-cardiac arrest care of the patient that has achieved return of spontaneous circulation (ROSC). These things include: optimizing the patient’s hemodymanics, getting a 12 lead EKG, induction of hypothermia, the use of waveform capnography to continually monitor the airway, and optimization of arterial oxygen saturation.
2010 Guidelines for the Initial Biphasic Dose in Cardioversion of Unstable Patients
Rhythm
| Initial Biphasic Energy Dose
|
|---|---|
Unstable Atrial Fibrillation
| 120-200 J
|
Unstable SVT or Unstable Atrial Flutter
| 50-100 J
|
Unstable Monomorphic VT
| 100 J
|
Let's Recap!!!
- Look, listen, and feel followed by 2 rescue breaths has been eliminated from the BLS procedure to facilitate more rapid initiation of chest compressions. We now start with chest compressions instead of giving 2 rescue breaths.
- The BLS procedure is no longer represented by the pneumonic A,B,C,D, as this sequence delays starting chest compressions, instead it is represented within the Chain of Survival by the numbers 1,2,3,4.
- High quality CPR is defined as chest compressions at a rate of at least 100 compressions/min at a depth of 2 inches allowing for complete recoil between compressions.
- Chest compressions should be continued while the AED or defibrillator is being readied and while it is charging in efforts to minimize breaks in chest compressions. Stoppage of chest compressions for any reason should be limited to <10 seconds.
- It is important to be properly trained in BLS or ACLS techniques. It is also important to be re-certified and updated on changes in procedure, so that those we help can have the best possible outcomes.
Works Cited
Sinz MD, Elizabeth. Advanced Cardiac Life Support Provider Manual: Professional. American Heart Association. 2010.