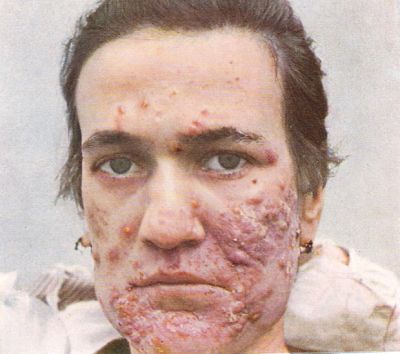
ACNE: the nightmare of adolescence
Overview
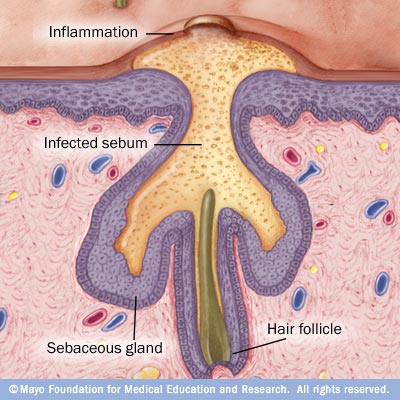
Acne is a common skin disease occurring mostly in young adults. It develops as a result of blockage of hair follicles. Sebaceous glands in skin enlarges & starts to produce more sebum(an oily substance secreted from our skin) under hormonal(androgen) influence at the onset of adolescence. These are commonly called pimples. Most pimples form on the face, neck, back, chest and shoulders. In these pimples bacteria (Propionibacterium acnes) start to grow & develop producing inflammation & the simple pimple is then converted into papules, infected pustules, or nodulesThese may produce mild to severe scarring of face . . Some others are cystic called nodulocystic acne. They produce severe scarring. Acne also affect psychology specially decreased self-esteem & depression. Severe form of acne is more common in male.
poll
have you suffered from acne in your life time?
severe acne


CAUSES
No one knows exactly what causes acne. But some probable reasons are
1.familial predisposition- A family history of acne is associated with occurrence of acne. Previous history of acne in the family and more specifically in the father or mother increases the risk of acne in children.
2.hormonal effects- During puberty, an increase in male sex hormones called androgens cause the follicular glands to get larger and make more sebum. During menstruation some hormonal changes takes place & causes exacerbation of acne.
3. Oily skin- this is because of increased sebum production. People having oily skin are more affected by acne. Sebum production is under control of androgen.
4. Early Onset of Acne Lesions- Acne lesions beginning before puberty increases the risk of severe acne.
5. Cigarette Smoking-acne is more frequent in smokers.
6. Drugs: (aggravating or inducing acne )
Steroids: first, it masks the condition then aggravates it.
Anabolic steroid.
Oral contraceptive pills ( norgesterone ) à androgen stimulants.
Thiazides
Rifampicin and lithium
Instructions to an acne patient:
1. The patient should know that it is long standing disease and self limited and require few years or at least 4 – 6 months to relieve ( as comedones need 4 months to appear )
2. Aim of treatment is healing with healthy skin without scar formation.
3. Treatment should include acne prone areas.
4. No use from excessive use of soap or excessive face washing.
5. Patient should not play with the lesions.
6. 5 % of patients may suffer from aggravation of the condition at first due to hydration of the skin by the vehicle if the drug.
7. Medical soap is ineffective as 1- the superficial bacteria has no role in the pathogenesis. 2 – the follicular bacteria can not be reached by this soap.
how acne forms
acne scars



TREATMENT OPTIONS
Non Inflammatory condition:
1. Tretinone
§ Best topical medication.
§ Conc. ( 0.01, 0.025, 0.05, 0.1 % )
§ 0.05 % is the most irritating conc.
§ Present in three forms : cream ( least irritating ), lotion and jell (most irritating )
§ Before use, a sensitivity test by application of the drug on dry skin at the night every other day for 3 times ( 6 days ) à if prove do be safe , continue treatment for 4 months.
§ You should start treatment by the lowest available conc. And the least possible irritating vehicle.
§ If no response, á irritation by changing the vehicle or á conc. Till reach the most suitable drug.
§ Application of the drug on exposure to UV rays or fluorescent lamp at 120 cm or less is unsafe. So, preferred to be applied at night or away from fluorescent lamp.
2. Azalenic Acid 20 % :
Slowly acting à gives best results after 8 weeks.
Used once daily at the first week à twice / day in the second week à till 8 weeks.
SE: pricking sensation
It should be applied on dry skin.
3. Irritant medications :
Tazarotene 0.1 ( ;ow irritant )
Iso trtinone 0.05 ( low irritant )
4. Non irritant medications : Adapalene 0.1
Inflammatory condition :
1. Benzoyl peroxidase :
§ Conc. : 2.5 % , 5%, 10 %
§ New conc. à 4% irritancy and 10 % efficacy.
§ New conc. à 8 % irritancy and 20 % efficacy.
§ Should be applied on skin for three days at night :
- If no response à give twice daily at night for 4 months
- If no sensitivity à give once daily at night for 4 months.
§ Disadvantages:
- Photo-pigmentation in fair skin.
- Dehydration à so , require more emollient.
2. Local Antibiotics:
i. Clindamycin 1 %
- Twice daily for 2 weeks.
- Effective but expensive.
ii. Erythromycin 2% or (4% +zinc):
- Twice daily with 8 – 10 hours interval.
- For 12 weeks then stop the drug for one week to prevent the development of resistance.
iii. Topical combined preparations:
- Benzoyl peroxidase 5% erythromycin 3%
- Erythromycin 3% + tretinone 0.03%
- Isotretinone 5% + clindamycin 1%
Systemic Preparations:
i.Macrolides:
- Tetracycline 1 / day
- Erythromycin 1g/ day
- Minocycline – doxyciline 100 mg / day
- The patient should e examined after 2 weeks.
- If good response à continue for 3 weeks.
- If not effective à double the dose for another 2 weeks.
- If no response à stop the drug and shift to another one.
- NB: never to mix topical and systemic antibiotics together
ii.Anti-androgens :
- Only for females > 35 years with other androgen dependent problems (hirsutism)
iii.Systemic retinoids:
- Only in severe nodulocystic acne, not responding to all other modalities.
- SE: hyperlipidemia , hepatotoxicity, GIT bleeding and teratogencity.
scars before & after treatment



Treatment of Post-acne scar:
1. Peeling:
- Never to be done with active acne as it is mutagenic and stimulates IL-1α.
- Pre-peeling preparations (tretinone for 6 weeks and glycolic acid ) are done firstà
Then one session / week .
- Never to exceed 5 sessions.
- Topical retinoids has the same effect and cheaper.
2. Blue light laser.
3. Photodynamic therapy
4. Intra-cystic steroids ( intra-regional) à mask the condition but not cure it
further readings
- Acne: MedlinePlus Medical Encyclopedia
- Acne
- Acne vulgaris - Wikipedia, the free encyclopedia
read further about acne
you may look into my other hubs
- HORMONE THERAPY FOR ACNE PATIENTS
an overview on hormonal therapy for acne patients. - AUTISM & DEALING WITH AUTISTIC BABIES
autism is a disorder of brain development where the patients suffer from impaired social interaction & communication. Their behavior is restrictive & repitative. Parents usually notice signs in the first... - PSYCHOLOGICAL DEVELOPMENT OF GIRLS DURING ADOLESCENCE
Adolescence is the most critical period of human life. It is the transition period between childhood & adulthood. This is further more critical for female as they have to pass through many drastic changes in... - what about anxiety disorder
Anxiety is a diffuse, vague apprehension associated with feelings on uncertainty and helplessness. This emotion has no specific object. It is subjectively experienced and communicated interpersonally. It is... - Anal Fissure
anal fissure A fissure-in-ano is a painful linear ulcer situated in the anal canal. It is a very common condition that causes suffering out of proportion to the size of the lesion. In the acute phase, the... - BLOOD IN URINE (HEMATURIA)
Gross hematuria (visible blood in the urine) can be one of the most frightening symptoms experienced by a patient. If encountered for the first time, a patient will notuncommonly consider it to represent an... - GLUCOMETER - An essential tool for diabetes control
Diabetes Mellitus is silent killer. It works continuously behind the patients eye. Sometimes the patient dont know about the killer that is working inside him. Occasionally he went to a doctor for a... - Anal itching or pruritus ani
Intractable itching around the anus may occur at any age but commonly in adult, more in men than women and more common in summer than winter and is not in itself a specific clinical entity or disease. The...