Bipolar Disorder and Management

Introduction and Case Study
Acute treatment of acute bipolar episodes targets symptom resolution and reducing immediate risk to oneself and others. [1] Long term aims are preventing future episodes, help regain a pre-morbid functioning capacity, improve physical health and minimize long-term suicide risks. [1] Despite the strength of current evidence-based treatments, definitive evidence on the best treatment choice is lacking. [1]
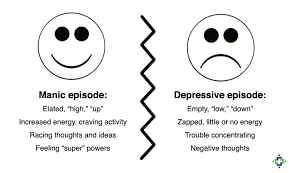
William displays elevated mood displayed by his presenting condition, elevated RR, HR and BP despite no added heart sounds to indicate cardiovascular disease. However we need to consider his propensity for cardiac disorders due to family history from his father. The recent loss of his father is a traumatic life event that precipitated his mood episode He also has a hereditability of 0.75 of developing depression like his mother. [1] Furthermore, manic and depressive symptoms often coexist in bipolar disorders so we need to address both poles in therapy. [1] Being 24 years old, he has early onset disorder triggered by recent stressors and possible alcohol disorder. [1]
Mania treatment requires inpatient care and his highly disturbing behaviour may require acute treatment with antipsychotics, benzodiazepines or both for rapid tranquilizing while avoiding excessive stimulation and provision of a calm environment. [1] An intensive support and treatment adjustment may be required to prevent escalating to mania in Bipolar 1 disorder. [1]

Available Treatments
Antipsychotics are first-line mania treatment especially in severe cases. [1] A multiple-treatments meta-analysis of 68 RCTs reported that antipsychotics, lithium, carbamazepine and valproate were more effective than placebo. [1] The most efficacious were haloperidol, risperidone and olanzapine ;all displaying better effectiveness than valproate. [1] Haloperidol is more efficacious than lithium. [1] It is recommended that therapies can be combined if monotherapy with an antipsychotic, lithium or valproate is not sufficient. [1] A meta-analysis of 8 RCTs reported better efficacy using combined antipsychotic and lithium or valproate versus lithium or valproate alone. [1]
Benzodiazepines may be required for short term management of insomnia and agitation. [1]
Those who alternate between mania or hypomania and depression are especially challenging to treat, thus mood stabilizing is as important as treating the acute episode. [1]
Depression is treated through removing precipitants like in elevated mood management. [1] Drug choice is guided by drug history and the requirement to avoid switching to elevated mood. Though there’s limited evidence for bipolar depression, a meta-analysis of 19 RCTs reported quetiapine as best evidence versus placebo. [1] Olanzapine and combined olanzapine/fluoxetine and lamotrigine were found to be effective too. [1] However, 15 RCTs found no significant benefits of antidepressants compared to placebo in treating bipolar depression. [1] Guidelines recommend that antidepressants must be combined with an anti-manic drug to minimize risks of destabilizing mood and should be withdrawn after depressive symptoms are resolved. [1] SSRIs are the treatment choice due to their minimized propensity to cause a switch to mania. [1] Psychological treatments used concomitantly with drugs are helpful in prolonged or recurrent depression or mild symptoms persist. [1]
A double-blind placebo-controlled Phase-III trial reported that the antipsychotic cariprazine 3-12mg/day was both safe and well-tolerated to treat manic and mixed episodes of bipolar 1 disorder. [2] Results show statistically significant better reductions in YMRS (Young Mania Rating Scale) at week 3 and most treatment-emergent adverse events (TEAEs) being mild or moderate (placebo 98.9%, cariprazine 97.2%) and benzodiazepine use as a rescue drug to control agitation was slightly higher in placebo (81%) versus cariprazine group (75%). [2] Cariprazine has great efficacy because if its high affinity and occupancy at Dopamine D2 and D3 receptors (Kiss et al 2012) and D2-receptor blockade could underlie the basic anti-manic effects of most antipsychotics (Harrison-Read 2009). [2] Moreover, recent evidence report that anti-manic effects of mood stabilizers (lithium and valproate) and antipsychotics could be partly mediated by the GSK-3 signalling pathway and activity at D3-receptors was shown to improve D2-receptor-mediated GSK-3 signalling (Bealieu et al.,2007). [2] Redent data found that cariprazine inhibits D-receptor/β-arrestin 2-dependent interactions at a potency that’s equal to haloperidol and fivefold better than aripiprazole (Gao et al.,2014) hence cariprazine’s high affinity and possible partial agonist effects at D3-receptors may be responsible for its strong anti-manic effects. [2]
Antipsychotics are commonly linked with weight-gain, metabolic problems, prolactin-increase, sedation and QT-interval prolongation. [2] Mean changes in bodyweight and metabolic changes were generally minute and similar between cariprazine and placebo groups and suggest a favourable metabolic profile of cariprazine although longer studies are warranted to better indicate its metabolic effects. [2] Cariprazine was not associated with cardiovascular adverse events or QT-prolongation, elevated prolactin levels or sedation(<3% of patients) and somnolence incidence was moderately higher with cariprazine (6%) versus placebo (1%). [2]
A multinational, multicenter trial by Durgam et al. reported that 1.5mg/day cariprazine showed consistent efficacy for treating bipolar 1 depression versus placebo and was generally well-tolerated. [3]
Quetiapine is the medication with greatest evidence for effectiveness in Bipolar 2 depression. [4] A RCT by Swartz et al. compared psychotherapy alone versus combined with medication to treat bipolar 2 depression reported that IPSRT/quetiapine combination caused greater symptomatic improvement but more side-effects versus IPSRT monotherapy, reiterating that harms versus benefits and preferences must be considered when recommending treatments for bipolar depression. [4]
A large multicenter double-blind placebo-controlled RCT by Weisler et al. reported that extended-release carbamazepine (ERC-CBZ) capsules initiated at 400mg/day and increased where needed and tolerated to a maximal 1600mg/day were effective as monotherapy in acute mania in bipolar patients with manic or mixed episodes and showed significantly better improvements in YRMS (p=0.032) with at least 50% reduction in YRMS score at endpoint (41.5& versus 22.4% in placebo; p=0.074) and significantly improved HAM-D (Hamilton Rating Scale for Depression) score on day 21 (p=0.01). [5] Adverse effects occurred more frequently in the ERC-CBZ group than placebo and included dizziness, somnolence and nausea. [5]
Weisler et al. 2006 also reported that ERC_CBZ is an effective treatment for bipolar 1 with either acute manic or mixed episodes. [6]
For mania and mixed states, drugs that displayed good evidence of efficacy are:
- Antipsychotics as a class [1]
- Lithium [1]
- Valproate [1]
- Combined treatment with antipsychotics plus lithium or valproate [1]
- Carbamazepine (suggestive evidence) [1]
- Short term benzodiazepines to treat agitation and insomnia
For depression, Quetiapine and cognitive behavioural therapy and family focused therapy displayed good evidence of efficacy whereas antidepressants showed poor evidence. [1]
Maintenance treatment to prevent relapse with good evidence are:
- lithium monotherapy (mania and depression) [1]
- Antipsychotics as a class (mania) [1]
- quetiapine (depression and mania) [1]
- olanzapine (mania>depression) [1]
- lamotrigine (depression>mania) [1]
- Combined therapy with antipsychotics and lithium or valproate (better versus lithium or valproate monotherapy) [1]
- Lithium & valproate (better versus valproate for overall relapse) [1]
- Quetiapine and lithium (better than valproate or lithium monotherapy for mania and depression) [1]
Juruena et al. reported that OXC (oxycarbazepine) seems to be significantly more efficacious and is better-tolerated than CBZ (carbamazepine) as an add-on treatment to lithium in bipolar I and II patients. [7] This is a pilot, randomized clinical trial and suggests the potential benefit of OXC as adjunctive therapy to lithium both in acute and long-term treatment of bipolar disorder. [7] More adequately placebo-controlled trials are needed. [7]
Treatment Plan
We need to tackle the problem by dealing with all facets; acute treatment and prevention of mania, depression and maintenance treatment to prevent relapse;
Quetiapine or Lithium monotherapy have comparable efficacy although quetiapine has better evidence of efficacy for acute treatment and prevention of depression symptoms. [8] Quetiapine/lithium combination is superior versus monotherapy of either medicine for treating acute mania although no benefit was observed for acute bipolar depression from the addition of lithium. [8]
It’s important to consider the side-effects from lithium (tremor, thyroid or gastrointestinal) and quetiapine (sedation/somnolence and weight gain) when recommending treatments. [8] Thus, combined therapy will yield additional adverse events. [8]
Prospective trials reported that in mixed mania/hypomania like William, Aripiprazole, asenapine, carbamazepine, olanzapine and ziprasidone showed strongest evidence of effectiveness in acute-phase therapy and quetiapine and divalproex/valroate were also effective. [9] In severe cases, combination therapies with these atypical antipsychotics and mood stabilizers can be utilised. [8] Olanzapine and quetiapine (monotherapy or combined with lithium or divalproex) showed best evidence in maintenance therapy. [9] Lithium and lamotrigine may have benefits in preventing suicide and depressive relapse. [9] Further prospective studies with primary focus on mixed states are needed. [9]
Carbiprazine 1.5mg/day (starting dose) is a good therapeutic option for manic or mixed episodes in bipolar i disorder but unfortunately is not available in Australia. [3,9] Doses are increased to 3mg on day 2 and further dose adjustments can be made in 1.5mg-3mg increments depending on clinical response and tolerability (Dose range =3-6mg/day). [10]
William suffers from constipation so maybe hold off on lithium due to gastrointestinal side effects risks. In most clinical practice guidelines, quetiapine is recommended over lithium with higher evidence of efficacy for treating acute bipolar depression and UK guidelines support quetiapine or lithium as first line treatments for those with predominant mania like William whereas quetiapine is recommended for those with predominant depression. [8,11]
A systematic review of RCTs of newer drugs in mania treatment reported that quetiapine, olanzapine and valproate semisodium were superior to placebo in reducing manic symptoms. [12] No differences in efficacy were reported between the above three drugs in comparison with lithium. [12]
His treatment should be [11,13]:
- For acute mania; Quetiapine XR 600mg/day is an effective target dose. [11]
- Bipolar disorder; Quetiapine (extended-release) 300mg/day on day 1 and 600mg/day on day 2 and for maintenance from day 4 onwards; 400-800mg/day [11, 13]
- Short term benzodiazepines to treat agitation and insomnia. [1]
Following the initial treatment, William was able to cope with this situation well. He re-joined his work a month later but appeared to have lost interest in his job. He finds it difficult to perform at the same level and seriously thinks of selling his firm to the junior partner. He believes that the medicines are slowing him down, but at least, he is able to function as a normal person and therefore, happy to continue like this. On the most recent visit to the Psychiatrist, William appears to gain significant weight that is anticipated due to the Sodium Valproate he is on. William is taking 2 tablets of 500mg each twice a day of Valproate and same PRN Temazepam 10-20mg for sleep. The Psychiatrist also noticed some bruising in both his arms and on questioning William showed him his abdomen with further signs of bruising.
REFERENCES
1)Anderson I, Haddad PM, Scott J. Bipolar disorder. BMJ 2012 Dec;345:e8508 doi.10.1136/bmj.e8508: Pages 1-10
2)Sachs GS, Greenberg WM, Starace A, Lu K, Ruth A, Laszlovskyj I et al. Cariprazine in the treatment of acute mania in bipolar 1 disorder: a double-blind, placebo-controlled, phase III trial. J Affec Disor. [Internet]. 2015 Mar 15;174:296-302. Available from: http://www.sciencedirect.com.ezproxy.utas.edu.au/science/article/pii/S0165032714007289?via%3Dihub
3) Durgam S, Earley W, Lipschitz A, Guo H, Laszlovsky I, Nemeth G et al. An 8-week randomized, double-blind,, placebo-controlled evaluation of the safety and efficacy of cariprazine in patients with bipolar 1 depression. Am J Psychiatry. [Internet]. 2016 Mar 1; 173(3):271-81. Available from: http://ajp.psychiatryonline.org/doi/abs/10.1176/appi.ajp.2015.15020164?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed
4)Swartz HA, Rucci P, Thase ME, Wallace M, Carretta E, Celedonia KL and Frank E. Psychotherapy alone and combined with mediation as treatments for Bipolar II depression: a randomized controlled trial. J Clin Psychiatry. [Internet]. 2017 Jul 11. Available from: http://www-psychiatrist-com.ezproxy.utas.edu.au/JCP/article/Pages/2017/v78n07/16m11027.aspx
5) Weisler RH, Kalali AH, Ketter TA. A multicenter, randomized, double-blind, placebo-controlled trial of extended-release carbamazepine capsules as monotherapy for bipolar disorder patients with manic or mixed episodes. J Clin Psychiatry. [Internet].2004 Apr;65(4):478-84. Available from: http://www-psychiatrist-com.ezproxy.utas.edu.au/jcp/article/Pages/2004/v65n04/v65n0405.aspx
6) Weisler RH, Hirschfield R, Cutler AJ, Gazda T, Ketter TA, Keck PE et al. Extended-release carbamazepine capsules as monotherapy in bipolar disorder: pooled results from two-randomised, double-blind, placebo-controlled trials. CNS Drugs.[Internet]. 2006;20(3):19-31. Available from: https://www-ncbi-nlm-nih-gov.ezproxy.utas.edu.au/pubmed/16529527
7) Juruena MF, Ottoni GL, Machado-Vieira R, Carneiro RM, Weingarthner N, Marquardt AR et al. Bipolar I and II disorder residual symptoms: Oxycarbazepine and carbamazepine as add-on treatment to lithium in a double-blind controlled randomized trial. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Feb 1;33(1):94-9. Available from: http://www.sciencedirect.com.ezproxy.utas.edu.au/science/article/pii/S0278584608003187?via%3Dihub
8) Ketter TA, Miller S, Dell’Osso B, Wang PW. Treatment of bipolar disorder: review of evidence regarding quetiapine and lithium. J Affect Disor. [Internet]. 2016 Feb;191:256-73. Available from: http://www.sciencedirect.com.ezproxy.utas.edu.au/science/article/pii/S0165032715307722?via%3Dihub
9) Takeshima M. Treating mixed mania/hypomania: a review and synthesis of evidence. CNS Spectrums 2017;22:177-185
10)Medscape. Carbiprazine(Rx). Available from: http://reference.medscape.com/drug/vraylar-cariprazine-999874
11) Vieta E, Goldberg JF, Mullen J, Vagero M and Paulsson B. Quetiapine in the treatment of acute mania: target dose for efficacious treatment. J Affect Disord.[Internet].2007;100(1):s23-31. Available from: http://www.jad-journal.com/article/S0165-0327(07)00081-X/fulltext
12) Bridle C, Palmer S, Bagnall AM, Darba J, Duffy S, Sculpher M and Riemsma R. A rapid and systematic review and economic evlaution of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder. Health Technol Assess.[Internet]. 2004 May;8(19):iii-iv,1-187. Available from: https://www-ncbi-nlm-nih-gov.ezproxy.utas.edu.au/pubmed/15147609
13) Sandford M,Keating GM. Quetiapine: a review of its use in the management of bipolar depression. CNS Drugs. [Internet]. 2012 May. Available from: https://psychopharmacologyinstitute.com/antipsychotics/quetiapine/quetiapine-for-bipolar-depression/