Cardiovascular Disease in America - Simple Answers to Cut Costs and Suffering
Valenine's Day Can Help Us Remember the Heart Anywhere

America's Number One Killer
Cardiovascular Disease in America - © Patty Inglish, 2007; 2013
Cardiovascular Disease, also known as CVD, is the Number One Cause of Mortality (death) among American women and men. It kills the most men and women of any disease or condition.
- CVD affects over 33 million women and 31 million men in America as of the mid 2000s, and additional people suffer, but do not know at all that they do suffer from the disease (reference: Heart Disease and Stroke Statistics – 2004 Update.) Larger numbers of women of all races suffer CVD than do men and after age 75, even more women than men suffer from it among all diversities.
- CVD also affects American children and is the Number Three Cause of Death in children under the age of 15. (same reference).
Cardiovascular disease affects people of all ages in America and is an expensive health care consideration. CVD risk factors and inadequate treatment provided to American women and girls combine to produce the largest portion of CVD death and illness in the USA. This cost America over $368 billion yearly for CVD treatment and associated costs alone. CVD is a killer and it is an expensive killer.
In order to target this Number One National Health Problem, The American Heart Association (AHA) updated CVD prevention guidelines for women in early 2007, promoting a healthy lifestyle from early childhood or even infancy, throughout the lifespan. The AHA guidelines include a healthy diet, regular exercise, adequate sleep, and several other elements. These quidelines are particularly vital to the health of America’s children in the late 2000s, since US children are obese by a large proportion. See the AHA Healthy Lifestyle guidelines in the left sidebar on their website at American Heart Association.
Health Care in America

Inadequate Treatment
Formerly, CVD was thought to attack a larger segment of American men than women, but that was incorrect. However, this notion was reinforced by the fact that clinical trials examining cardiovascular function and risk factors overwhelmingly examined males rather than females. In addition, women are less likely to show cardiovascular symptoms as early in life as do males -- Women begin to show symptoms an average of 10 years later in life.
CVD research literature and published insurance analyses (Murasko, pg. 1746) show that American women continue to receive less aggressive treatment for CVD events (popularly called “illnesses” , “attacks”, “episodes”, or “spells”) than do men. This is inadequate treatment that becomes worse as female patients become older. (reference: Murasko, ppg. 1746, 1755-6; Sarafidis, pg. 224; Alter et al., pg. 1916).
However, more American women survive CVD events like MI (myocardial infarction) than do American men. This adds additional long-term health related costs to American women that include the elderly with cardiac history that consistently received inadequate treatment in their medical histories. The risk to these American women of further CVD events in their futures is 1.5% to 15% higher than the average risk for all:
“After adjusting for baseline differences, the relative rates of angiography and follow-up specialist care for women relative to men, respectively, fell 17.5% (95% confidence interval [CI], 13.6 to 21.3, p < 0.001) and 10.2% (95% CI, 7.1 to 13.2, p < 0.001) for every 10-year increase in age [this means both treatments were inadequate for women in a significant way]. Conversely, long-term AMI survival rates in women relative to men improved with increasing age, such that the relative survival in women rose 14.2% (95% CI, 10.1 to 17.5, p < 0.001) for every 10-year age increase” [also significant - women survive more often]. (Alter, et al., pg. 1915).
“… for individuals with previously diagnosed heart disease or stroke, a lack of coverage [health insurance] is more strongly associated with lower rates of screening, pharmaceutical management, and physician contact in women than men.” (Murasko, pg. 1755).
These facts increase the total healthcare cost burden to the nation. CVD is a serious US Public Health Problem that requires focused priority attention to screening, testing, and treatment procedures; but most vitally to prevention throughout the lifespan.
Valentine's Day Can Remind Us Of Heart Health

Women and Heart Disease

International Unity
- The Heart Truth: A Campaign for Women About Heart Disease, HHS, NIH, NHLBI
The Heart Truth campaign raises awareness about heart disease in women. - The Heart Truth Canada
Women Live Longer and Suffer Longer
American females outlive American males by an average of 5 years or more and females over the age of 75 make up the fastest growing segment of the US population (Heart Disease and Stroke Statistics – 2004 Update.) CVD in America is quickly affecting a larger proportion of older women, thereby increasing their health care costs, and becoming a hallmark disease of “older women” that do not generally receive adequate treatment.
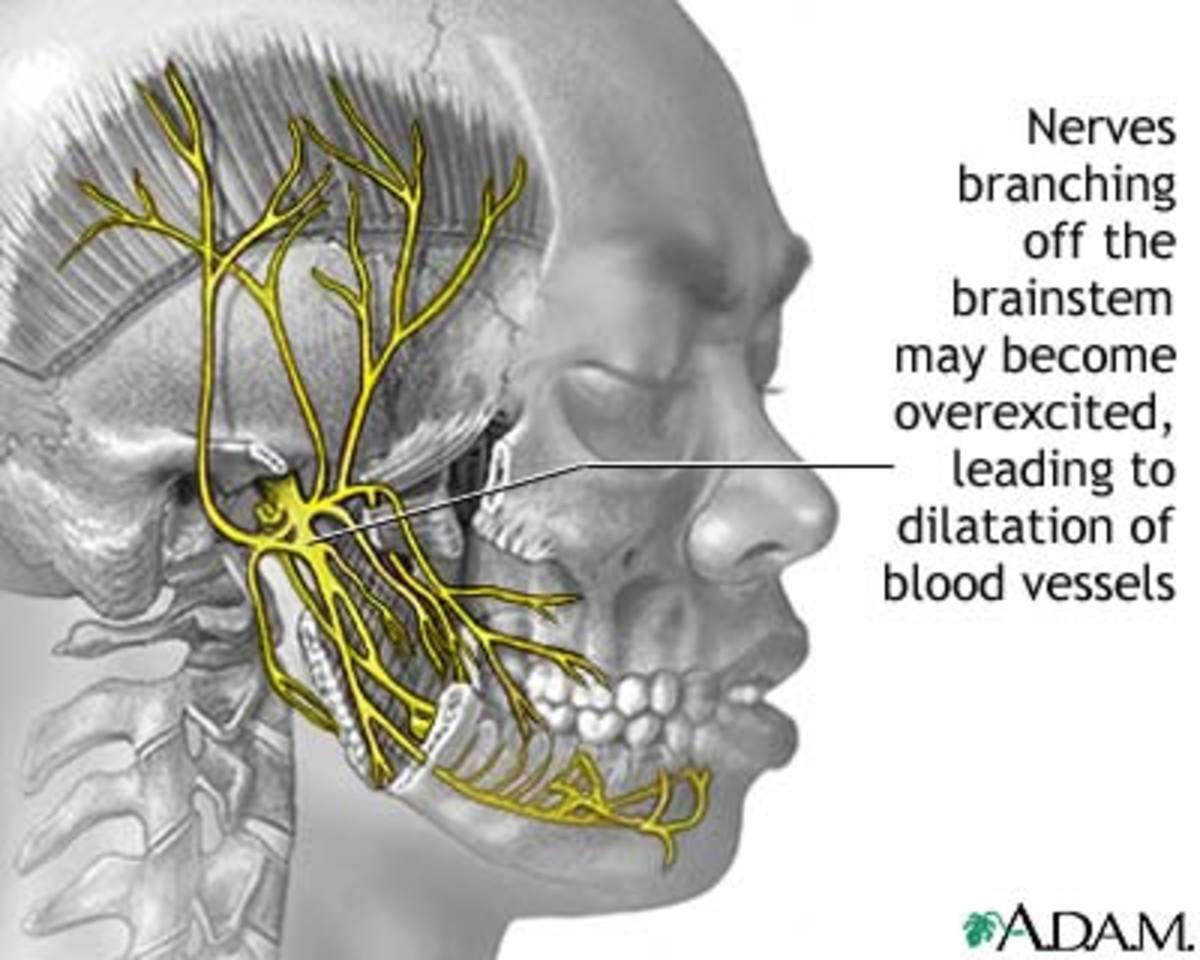
CVD can also be tricky. Among US women, up to 20% of CVD events happen without the following risk factors: advanced age, diabetes, hypertension, hyperlipidemia, and smoking. These women seem to have a CVD event “out of the blue.” In fact, about 2/3 of female CVD cases in the US are in women suffering a first CVD event without any previous cardiac history at all. This all makes CVD more difficult to detect in screenings among women than among men. American men usually have physical CVD symptoms, often chest pain (Heart Disease and Stroke Statistics – 2004 Update; Ridker, ppg. 611-12).
First Heart Health Fashion Show, 2011 @ Lincoln Center

Reynolds Risk Score
See how the Reynolds Risk Score works at this link: Calculating Heart and Stroke Risk for Women and Men.
The Harvard Health Newsletter compares the Framingham Risk Score with the Reynolds Risk Score at Heart Attack Risk.
Healthy Lifestyle
New Information and New Hope
The AHA has established three new levels of CVD risk in 2007: high risk, at risk, and optimal risk, replacing the previous four levels of the Framingham model for CVD. Dr. Mosca noted that the new AHA model is better and more appropriate, because it accounts for overall lifetime risk, diversity, and stroke risk.
At the same time, the AHA model may be improved by recent findings. Ridker et al., in a 10-year study of 16,400 American females at least 45 years old and older, found in 2006 that two additional factors would help doctors to zone in on the accurate CVD risk for women across a period of time of 2 to 3 decades. This resulted in the Reynolds Risk Score.
The Reynolds Risk Score more accurately measures the amount and nature of CVD risk factors which, in turn, facilitates early prevention of Cardiovascular Disease. The added factors include 1.) a very accurate family health history that included CVD and 2.) the level of inflammation present in the patient, found by looking at “C-reactive protein levels” or CRP, which can be easily measured by the blood test known as “hsCRP.”
The good news is that if it is consistently put to use, the Reynolds Rock Score can find American women and girls that can benefit from early prevention programs like low-dose daily aspirin and lipid-lowering treatments. This is very simple and can be easily used to cut healthcare costs among both women and men in America and reduce the suffering caused by CVD – especially the sneak attack of CVD without any previous symptoms or risk factors.
Reduce Cardiovascular Risk
Heart Healthy Nutrition
A Simple Answer
The fact of the matter is that all family health history should be included in any medical case or long-term healthcare record (at the family doctor’s office or neighborhood clinic, for instance) as standard practice and the Reynolds Risk Score can be used as a wellness procedure.
It can be used well with American males, but it will definitely 1.) identify females without symptoms that are still at risk for CVD, 2.) provide the reason to treat to these people in a prevention program, 3.) reduce individual and national healthcare costs, and 4.) increase the overall quality of life for the fastest growing sector of the American population (older women). This is the remainder of the Greatest Generation and the Baby Boom Generation in the late 2000s; but the scenario will replay itself beginning in 30 years around 2035, when the Millennial Generation of the same approximate size as the Boomers begins to reach the same advanced age. This is a simple prevention measure that cam save money and suffering for at least the next 100 years, in which we may find still easier and less expensive preventative measures.
Moral of the Story
If individuals will ask for a Reynolds Risk Score and if it can be incorporated as a standard practice in American Medicine and in any national health plan to be instituted in the future of America, then we will have a powerful tool against the Number One Cause of Death in our country.
REFERENCES
- Alter D.A.; Naylor C.D.; Austin P.C.; Tu JV. “Biology or bias: practice patterns and long-term outcomes for men and women with acute myocardial infarction.” Journal of the American College of Cardiology. 19 June 2002. 39 (12):1909-1916
- Anderson R.D. and Pepine C.J. “Gender differences in the treatment for acute myocardial infarction: bias or biology?” American Heart Association’s Circulation. 2007. 115(7):823-826
- “Heart Disease and Stroke Statistics – 2004 Update.” Learn and Live.2004. [American Heart Association; Lori Mosca, MD, MPH spokesperson.]
- loadable/heart/1079736729696HDSStats2004UpdateREV3-19-04.pdf Retrieved 8 Mar. 2007.
- Murasko, J.E. “Gender differences in the management of risk factors for cardiovascular disease: the importance of insurance status.” Social Science and Medicine. Oct. 2006. 63(7):1745-56.
- Ridker Paul M. , MD, MPH; Buring, Julie E., ScD; Rifai, Nadir, PhD; Cook, Nancy R., ScD.
- “Development and Validation of Improved Algorithms for the Assessment of Global Cardiovascular Risk in Women.” Journal of the American Medical Association. 2007. 297:611-619
- Sarafidis, P.A.; McFarlane, S.I.; Bakris, G.L. Gender disparity in outcomes of care and management for diabetes and the metabolic syndrome. Current Diabetes Reports. June 2006. 6(3):219-24.