Why I stopped getting mammograms: How to decide on breast cancer screening that's right for you.

Mammography No Longer Gold Standard for Breast Cancer Screening
Are you confused about the changing breast cancer screening guidelines? I can't imagine why.
"Three different groups are recommending three different ages -- 40, 45, and 50 -- when regular breast cancer screening should begin." ("In major shift, new guidelines scale back breast screenings in younger women").
1. The American Cancer Society (ACS) increased the age for mammograms from age 40 to 45 and then every two years at age 55. The ACS no longer recommends breast self-exams or clinical breast exams (doctor or nurse feel for lumps) due to the high false positive rate (finding something that is not harmful but often leads to added screening or even a biopsy).
"After 2003, the society changed its guideline development procedures to be more transparent and evidence-based; these new recommendations are a result." ("Why New Guidelines Probably Won't Mean Fewer Mammograms," Carroll, Aaron, E. The New York Times. Oct 21, 2015).
The revised ACS guidelines are however, for women without risk factors such as the BRCA1 and BRCA2 genetic mutations or a family history of breast cancer.
2. The U.S. Preventative Services Task Force reaffirmed it's position that women between the ages of 50 and 74 get a mammogram every two years. They do not recommend breast self-exams and suggest evidence to support clinical exams is "insufficient."
3. The American College of Obstetricians and Gynecologists maintain their recommendations, an annual mammogram starting at age 40, annual self and clinical breast exams.
“ACOG strongly supports shared decision making between doctor and patient, and in the case of screening for breast cancer, it is essential. We recognize that guidelines and recommendations evolve as new evidence emerges, but currently ACOG continues to support routine mammograms beginning at 40 years as well as continued use of clinical breast examinations.”
In the past earlier detection meant saving more women's lives. New studies show however, early screening hasn't reduced mortality rates but has lead to over diagnosis. In other words, early screening finds small tumors that undetected and left alone likely resolve on their own. Over diagnosis leads to added anxiety for thousands of women, further expensive diagnostic screenings and invasive biopsies.
A paper in The Journal of the American Medical Association noted, data from more than two decades of screening for breast and prostate cancer call that view into question. Besides finding tumors that would be lethal if left untreated, screening appears to be finding many small tumors that would not be a problem if they were left alone, undiscovered by screening. They were destined to stop growing on their own or shrink, or even, at least in the case of some breast cancers, disappear. ("Cancers Can Vanish, But how?" The New York Times. October 26, 2009).
What everyone does agree on is that breast cancer screening no longer meets a one size fits all women approach.
So, how do you decide if you should get a mammogram at age 40, 45, or 50 and if you should get one every year or every other year (most experts agree there is no benefit to mammography after age 74 or within 10 years of life expectancy)?
Unfortunately there's no simple answer. But before I get into some steps that might help you decide, the first place to start is how we view disease prevention.

Focus More on Prevention Rather than Disease
Many experts, including women's health expert Dr. Christine Northrup, agree our focus should be on breast health, rather than on disease.
Women have been scared out of their minds that if they don't get a mammogram at least every couple years (depending on their age) they're playing with some seriously scary odds.
With 40,000 breast cancer deaths a year who can blame us women for being terrified? (although the leading killer of women is heart disease).
But mammography not only isn't saving as many lives as once hoped, it's adding anxiety for women and leading to unnecessary invasive procedures.
Women and health care providers need to focus more on maintaining healthy breasts (lifestyle, diet, hormone balance) and on early detection of breast tissue changes by adding a non-invasive, no radiation test to their routine screening called a thermogram (see "6 tips for healthier breasts" below).
"Instead of just screening for breast cancer, a thermogram can tell you how healthy your breasts are. It also has the potential to truly detect breast cell anomalies long before mammography can detect cancer, when done properly. This allows you to implement lifestyle changes that can improve the health of your breasts proactively instead of waiting for a cancer diagnosis later." ~ Dr. Christine Northrup.
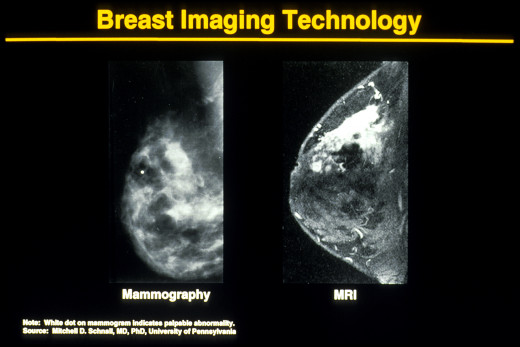
Easy to understand comparison of mammogram, thermogram, MRI and ultrasound for breast screening
5 Steps to Help You Decide on Your Breast Cancer Screening
1. Know your risk but don't let your risk own you.
Only 5-10% of breast cancers are thought to be hereditary. Even if you have the BRCA1 or BRCA2 gene this doesn't mean you will get breast cancer.
There are plenty of steps you can take (See "6 tips for breast health" below) to lessen the odds you'll ever have to go down the road your relatives traveled with breast cancer.
Calculate your breast cancer risk here.
(Personally, I opt out of knowing my calculated risk because if it 's high this information would freak me out. I don't want to freak out. This is where our individual value system and comfort level with breast screening comes in. What feels right for ME might feel wrong to YOU).)
2. Find an open-minded and integrative health care provider
I can't emphasize this enough.
Most people my age (50) and older were taught to defer to their doctor as the ultimate authority on their health. Yet, doctors are trained in different schools of medicine which informs how they view prevention, wellness and disease.
If your insurance covers an integrative physician or you can afford to pay for the doctor's fees out-of-pocket (labs, screening and diagnostic are often covered even if the doctor isn't on your plan), I strongly recommend going to an integrative physician.
Integrative physicians combine holistic healing and where appropriate, conventional practices. They focus on disease prevention and take the whole person into consideration including the complex interaction of lifestyle, nutrition, genetics, the mind (powerful), the digestive, immune and lymphatic systems, toxin load and the patient's hormone/endocrine system.
My doctor, Dr. Sangeeta Pati, and my radiologist are incredibly patient-centric. Both offer breast screening recommendations based on my risk, screening results and personal beliefs. Both explain options and ask what I'm comfortable doing.
Both work on my behalf to (try) to get my insurance company to approve a non-standard MRI and/or ultrasound in lieu of a mammogram. But because insurance companies follow the "gold standard" for breast screening (mammography unless abnormal findings or risk factors call for additional screening, diagnostic mammogram, MRI etc) and in my view, insurance companies have mastered the art of taking our money and then saying NO, getting approval is tough.
Last year when I asked for an MRI? Impossible.
Ask your doctor her opinion on the current (and conflicting) screening guidelines and about steps you can take for breast cancer prevention. If when you ask questions (including her view on breast thermography) your doctor seems dismissive or annoyed, find another doctor.
Seriously.
It's critical your health care provider is a wellness partner rather than some scolding authority figure who takes you for an insolent patient Who Dares to Question the White Coat.
She may not agree with your point of view but she should treat you with empathy and respect (And so to should patients consider their doctor's knowledge, insight and experience, and let me add, human fallibility).
3. Do some homework
This might sound arrogant but your doctor isn't the expert, you are.
I have great respect for the numerous health care practitioners I've seen over decades. A doctor however, is a paid consultant, albeit a highly trained and knowledgeable consultant, but she can't inhabit the the complexities of your body and mind.
Your doctor is in the business of detecting and treating disease in virtually hundreds of patients (and abiding by mounds of suffocating insurance guidelines which can hamper spending adequate time with each patient. This is one reason my physician won't take insurance, but I still file).
Your body, lifestyle, genetics and comfort level with breast cancer screening are therefore, unique to you.
The more informed you are about current research on breast cancer prevention and the screening tools the more in control you are to steer your own wellness.
Research the latest findings on breast health, cancer prevention and detection tools
Use the gold standard research depository, the National Institute of Health's Pub-med to access published peer-reviewed studies. If you want to read a summary of combined research (strength in numbers) Google "meta analysis" for example, of "breast cancer screening." A meta-analysis combines the statistical findings of multiple independent studies and provides an overview of findings to date.
If you prefer to move past the scientific jargon to layman's terms, go to my gurus for health and wellness:
- Dr. Christine Northrup, well-respected women's health expert. Dr. Northrup isn't against mammography but she emphasizes cancer preventation and breast health and is in favor of thermography.
- Dr. Joseph Mercola, an alternative medicine, conventional medicine boat rocker who links all his articles to peer-reviewed research. Dr. Mercola is unequivocably against all mammograms but like Dr. Northrup focuses on prevention and thermography.
- Women in Balance - a vast resource for women's health
- And the gold standard for conventional health findings and recommendations, The National Institute of Health, Mayo Clinic and WebMD.
4. Compare the plusses and minuses of each screening tool
Ask your doctor to explain the strengths and weaknesses of mammography (e.g. 3D tomosynthesis has slightly more radiation than 2D mammography but is more accurate). breast cancer detection tools (mammography, MRI, ultrasound, clinical exam and thermography). If they dismiss the impressive body of research on breast thermography, dismiss them).
(Excellent video that explains differences between each screening tool.)
Mammography MRI, ultrasound, thermogram and a clinical breast exam by a health care provider each have distinct strengths and weaknesses. Each tool reveals different characteristics about your breast tissue.
Thermogram focuses on risk assessment, mammography, MRI and ultrasound focus on disease detection.
Mammogram detects structural issues (micro-calcifications), thermography detects physiological (inflammation, hormonal imbalances) issues. The tools do NOT replace one another. Each tool varies in sensitivity (to pick up the smallest of small) and the specificity (to determine the characteristics of an abnormality).
Here's the challenge, however:
The paradox of multi-modality breast screening is the more screening you do, this almost guarantees something dangerous OR something completely harmless will show up.
Look enough and you'll find "something," something that left undetected in your breast more than likely you'll die with, rather than from. Moreover, added screening adds anxiety, cost and at times, invasive biopsies.
So, what do you do?
5. Finally, do a decision tree to decide your screening
Ultimately while it might be a huge relief to leave all the decision-making up to your doctor, we're all ultimately in control of our own body.
I can't tell you how many times I wanted to tell my doctor and radiologist, "Just decide for me what I should do." I know if I asked right now, my radiologist would recommend (but not push) the 3D mammogram. Last week my sonographer who did my breast ultra sound said, "I've never had a patient come in who did a screening ultrasound but not a screening mammogram."
I was nervous and confused IF and how OFTEN I should get a mammogram (note the three different recommendations I mentioned earlier). I’ve had about 15 or more mammos since I turned 30 (lump in college turned out to be nothing but I started mammo early).
I decided I’m not a mammogram fan anymore for the following reasons:
- I don't want the radiation. (3D mammo I did last year has more radiation than 2D)
- Mammography isn't an ideal detection tool for dense breasts (which I have).
- I don't want the compression. It's not that flattening my boobs into pancakes is painful (for me) it's that there's some risk in compressing (potentially) hidden cancer cells.
"Most frightening, if a woman does have a cancerous lump," writes Sylvia Booth Hubbard in Can Mammograms Spread Cancer? undergoing a mammogram can cause it to spread, explains Dr. Blaylock, author of The Blaylock Wellness Report. 'If you already have a cancer, in addition to being painful the crushing compression the breast undergoes during a mammogram can cause the cancer to spread. Doctors are taught that once a lump is found, you don't press it — not even during an examination — because you will cause the cancer cells to spread.'"
So, every year around my breast screening due date I ask myself the following:
- What are my risk factors?
- What have I learned so far about mammography (risks vs benefits)?
- What does my thermogram reveal about my breast health?
- Do my doctor's recommendations align with my beliefs and comfort level?
I had a scare a couple years ago and this is how I worked through it.
In 2013 my annual thermogram indicated an abnormal finding on my left breast (high vascularity meaning lots of vessels feeding an area. Cancer needs vessels to feed it, which is not to say highly vascular breasts MEAN cancer, it means keep an eye on).
On the other hand, my MRI revealed an abnormal finding on my right breast (tiny calcification). Great, I thought. Two entirely different findings.
(As I mentioned earlier, each screening tool detects abnormalities at a vastly different sensitivity and specificity rate. A thermogram can't detect structural issues (nodules, tumors) an MRI can't detect physiological/functional issues, e.g. inflammation, thus the two different findings).
I should add I'm adopted (no available family history). Also, like most people, I've known several friends and family diagnosed with breast cancer (all doing well).
At one time, my breast cancer screening anxiety level was off the charts. I don't worry (as much). Here's why:
- I have a better understanding how to maintain healthy breasts (see below for "6 tips for healthy breasts")
- Because most "abnormal" findings turn out to be nothing. (I've had three abnormal findings in my lifetime).
- Because I trust thermography to detect early breast tissue changes (inflammation, vascularity) I worry a lot less. (Again, thermography is NOT a detection tool. It can't find lumps, it detects tissue changes and tracks these changes over time).
Still, the I was confused and a little worried about my findings last year So I asked the radiologist:
- What do these findings mean in terms of cancer risk? (My radiologist told me even if it was cancer, it was so tiny we caught it uber early).
- What does the size, internal structure (hard or fluid) and abnormal shape of the finding suggest? (uneven edges indicated abnormal, internal structure indicated nothing to worry about).
- And the big one, do I need to worry? The answer was no. This was a wait and watch. I agreed to do a 6 month follow-up thermogram and MRI (and ultrasound). Six months later, everything was normal.
Do you get a mammogram every year?
6 Tips for Healthier Breasts
1. Add thermography
Thermography is a painless, non-invasive, non-radiation procedure that detects heat and tissue changes which may be (but isn't necessarily) an early indication of a current or future problem.
Thermography provides women with early information about the health of their breasts so they can make lifestyle, hormone, and nutritional changes that may reverse signs of a simmering problem.
"While mammography, ultrasound, MRI, and other structural imaging tools rely primarily on finding the physical tumor, DII is based on detecting the heat produced by increased blood vessel circulation and metabolic changes associated with a tumor’s genesis and growth.
By detecting minute variations in normal blood vessel activity, infrared imaging may find thermal signs suggesting a pre-cancerous state of the breast or the presence an early tumor that is not yet large enough to be detected by physical examination, mammography, or other types of structural imaging. " (Thermography.org).
I include thermography under breast health/prevention because with the guidance of a health care practitioner who is familiar with breast thermography, women can make changes that often reverse early warning signs of potential disease. These changes may include lifestyle and dietary changes, detoxification and balancing hormones.
"Thermography, DeLand said, can detect tissue changes that may indicate tumor development within its first year, whereas mammography wouldn’t pick it up for at least eight years. Only a biopsy can determine whether cancer exists. 'You get one every year, you’re going to see if something starts happening,” DeLand said of thermography. “You’re not going to get into hot water. You’re not going to all of a sudden have something really, really critical if you keep up with your annuals.'"
Thermogram is not a substitute for other screening methods. Thermography can't detect structural issues (nodules, tumors). Doctors use it as an adjunct (in addition) to other screening tools.
If you decide to add thermography to your breast screening protocol be sure to find a medical thermal imaging professional certified by the American Academy of Thermography. A thermographer doesn't interpret, results are sent to a physician trained in analyzing thermal imaging data.
2. Balance your estrogen to progesterone ratio
The hormone replacement issue is wildly misunderstood. Yes it's true, excess estrogen and/or low progesterone (estrogen dominance) does increase breast cancer risk.
But women. if you need hormone replacement (HRT) please don't be afraid. The misleading Women's Health Initiative (WHI) study threw everyone into unnecessary anti-HRT hysteria.
The WHI studied older women who took synthetic hormone replacement, notably Premarin (estrogen) and Provera (progestin) which are not remotely close in molecular structure to what your body recognizes as natural.
"In 2008 a large French study of 54,548 women (Fournier, A; Int J Cancer 2005) who were on average 53 years old, looked at breast cancer risk in relation to different types of hormone replacement therapy. The results showed that women on HRT combinations containing synthetic estrogens and progestins, had increased risks for breast cancer, while those using bioidentical combinations did not have any increase in risk for breast cancer. Fournier also concluded that when combined with synthetic progestins, even short-term use of estrogens might increase breast cancer risk." (Women in Balance. "Hormone Balance: The Key to Breast Cancer Prevention)"
For women who need HRT (pre or post menopausal or women with symptoms or women who had a hysterectomy) bio-identical hormone replacement is not only safe but can save lives.
Follow the guru of bioidentical hormones Dr. John Lee. Dr. Lee gives the all important rules for who and how hormone replacement should be used. (Use the least amount to alleviate symptoms. Stay balanced. Monitor levels regularly).
Hormones are powerful chemicals that unlock numerous processes in the body and with the right kind in correct and monitored doses, bioidentical hormones can protect women from breast cancer.
(And, balanced hormones make women feel good. I have a life long pituitary disorder so I've been on some form of HRT for 30 years. Estradiol, progesterone, DHEA and testosterone. All monitored by my doctor.)
Get your hormones checked annually.
My doctor, an integrative MD, requires complete blood work, including hormones, every 6 months. Keep estrogen levels in check. (There is a good protective estrogen and a bad estrogen. Ask your doctor to measure both).
Moreover, our culture is swimming with estrogen-like substances called xenoestrogens (plastics, soy, etc) so it's not just what our body produces, but what our body is exposed to that affects our hormone levels.
3. Add adequate Vitamin D3
I take 5,000 mg of vitamin D3 per day. I follow the Vitamin D Council's guidelines, not the RDA.
"There are vitamin D receptors in breast tissue, and vitamin D can bind to these receptors. This can cause cells like oncogenes to die or stop growing, and can stop the cancer cells from spreading to other parts of the body. Therefore, it is thought that vitamin D may help in protecting against breast cancer, by making cells in the breast smarter."
See: Vitamin-D-May-Stimulate-Anti-Breast-Cancer-Protein
4. Eat a low inflammatory diet
Notably the Mediterranean Diet which is linked to lower incidence of breast cancer.
"Indeed, the study found that the greater the percentage of calories that came from extra-virgin olive oil in the women's diets, the lower their risk of developing breast cancer, Martinez-Gonzalez told Live Science. 'For every additional 5 percent of calories from extra-virgin olive oil, the risk was reduced [by] 28 percent,' he said. However, the researchers do not know if the lower risk may have been lowered due to the extra-virgin olive oil on its own, or if it was the effect of oil working in combination with the rest of the diet, he said."
5. Manage your mindset and stress.
I know, the relentless drum of "reduce stress" -- stresses you out.
You live in day to day reality not some utopian bubble where everyone sits around singing Kumbaya. You deal with kids and jobs and baseball schedules and carpools and bosses and broken water heaters and sickness and aging parents and obnoxious neighbors and traffic snarls and debt and falling finances.
But, whatever it takes, grab some quiet time to chill, breathe, meditate, pray, write or just think about why you're grateful. All of these actions stimulate a more positive mindset and restores the body and mind.
Ask for help.
Ask your spouse, friend, neighbor, mother, babysitter. Ask for help. Ask for help.
Learn the art of the polite "NO". Women aren't great at asking for help or saying no. We shoulder the load and then soldier on. But over time our bodies and mind always pay the piper.
“What we showed for the first time is that chronic stress causes cancer cells to escape from the primary tumor and colonize distant organs,” said Erica Sloan, a Jonsson Cancer Center scientist involved with the study. “We showed how stress talks to the tumor and helps it to spread.” In fact, the study found a 30-fold increase in cancer spread throughout the bodies of stressed mice compared to those that were not stressed.
6. Begin dry brushing your breasts to improve lymphatic flow
When I first heard heard about dry brushing I thought, how bizarre.
Dry brushing is a quick and simple technique to promote healthy breasts. Before I tell you HOW, here's a brief description of your lymphatic system courtesy of The Cancer Research UK website:
An area of breast tissue, under the skin, leads into the armpit (axilla). The armpits have many lymph glands, also known as lymph nodes. There is also a chain of lymph nodes that runs up the centre of your chest, by your breast bone. This is called the internal mammary chain. The diagram shows the network of lymph glands around the breast.
The lymph glands are part of the natural drainage system of the body called the lymphatic system. The lymphatic system is made up of a network of lymph glands, connected throughout the body by tiny tubes (vessels) called lymph vessels. Lymph is a yellow fluid that flows through the lymphatic system and eventually drains into veins. This system helps to get rid of waste products from the body.
Tissue fluid bathes the body's cells, drains into the lymphatic system and then circulates again. Lymph glands are important in cancer care because any cancer cells that have broken away from a tumour can be carried by the tissue fluid to the nearest lymph glands. So doctors always examine the lymph glands. If you have cancer, but no cancer cells in any of the nearby lymph glands, your cancer is less likely to have spread.
So, dry brushing is a simple technique to do before you get into the shower to increase circulation and and promote lymphatic flow and drainage.
How?
Take a long handled natural bristle shower brush and with mild pressure you should feel but shouldn't hurt, sweep up from your lower side rib to under your armpit to across your chest (above your breast) and down in between your breasts (sternum region). Do this 5-10 times on each side just before you get into a warm shower. It took me less than 2 minutes.
Summary
- Focus more on breast health than breast disease.
- Do your homework on breast cancer prevention and screening. Resource only credible sites. Limit your time online to avoid self-diagnosis hysteria.
- Know your risks but don't let your risks own you.
- Find an integrative healthcare provider.
- Compare breast cancer detection tools.
- Add annual thermography with an AAT certified thermographer with training in breast thermography.
- Eat good stuff, notably foods from the Mediterranean diet.
- Add vitamin D3 in adequate doses.
- Manage stress by whatever means possible.
- Ask for help. Ask for help. Ask for help.
- Smile. Laugh often and big.
The more you know, the better off your breasts