Stirring Up Controversy with Breast Cancer Screening
In 1969, at the age of 50, my mother was diagnosed with breast cancer. She went into the hospital for surgery and had a modified radical mastectomy. Her cancer, in its early stages, showed up in only one breast, and had not spread to any lymph nodes – but the surgical team removed both breasts.
My mother did not require chemotherapy, radiation, or any follow-up drug therapy. She did not have any physical therapy. For the most part, she stoically bore the pain, anguish and loss of her disease. Not a very expressive woman, Mother might not have attended a breast cancer support group, even if one had been available. And she never once considered consulting a plastic surgeon to discuss reconstructive surgery.
My mother just celebrated her 90th birthday two months ago. I’m so glad she survived breast cancer and never had a reoccurrence.
Giant Pink Ribbon in Louisville, Kentucky

What We Didn't Know
In 40 years, some things have changed with thinking about breast cancer, but in a way, so much is the same. While treatment modalities are starkly different than what my mother experienced, researchers still don’t have adequate knowledge about the causes of breast cancer or its prevention.
My sister was the first and only person in our family to voice her doubts about the diagnosis of cancer for our mother. Years later, she wondered and speculated. There is such a thing as denial, and it can be strong around the presence of any chronic disease. The possibility of breast cancer for any woman is enough to make the denial come out even more forcefully.
So, about 13 years after my mother lost her breasts, I posed this cancer diagnosis question to a new gynecologist I was seeing for a routine check-up. She said, “Yes, the pathology findings can occasionally go either way – the pathologist is under pressure to make a decision while viewing ambiguous evidence.”
Sadly, my mother does not have a copy of her pathologist’s report, so there is no way to know what kind of breast cancer cells she had. If only I knew, I might be able to make some sense of how a woman today – like me -- would be treated for her condition. I don’t question her pathologist’s findings – I simply ponder “what might have been and could be.”
Mother on Her 90th Birthday

The New Mammography Standards
The uncertainty this disease provokes is enough to make anybody’s head spin around, and the recent report last month from the U. S. Preventive Services Task Force (USPSTF), which recommended changes in screening mammography standards, provoked widespread outrage from U.S. senators, doctors, and women who had their own stories about friends and family members who’ve endured breast cancer.
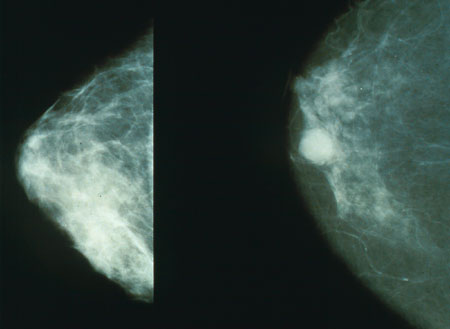
The task force revised its recommendations previously published in 2002, because of updated research. The guidelines now recommend that women ages 40-49 not be mass-screened with mammography; that women ages 50-69 have a mammogram every two years; and no particular recommendations for women over 70 due to the lack of strong evidence. If a woman is in her forties, she should discuss with her physician the relative risks and benefits of mammography at her age, and make her own choices.
Harms vs. benefits is a consideration with any type of health screening procedure. It is a fact that younger women who are pre-menopausal have very dense breast tissue, tissue that makes it very difficult to distinguish a tumor on a mammogram. Pre-menopausal women are also more at risk with radiation exposure than are older women. More than 80% of all breast cancers are discovered by the women themselves, not by imaging techniques.
What Harm Can It Do?
So, from the words of the task force, here are some of the harms associated with screening mammography for breast cancer:
-
Psychological harm (yes)
-
Unnecessary imaging tests and biopsies (been there, done that)
-
Inconvenience due to false-positive screening results
-
Over-diagnosis (weigh the harms associated with treatment of cancer that would not become clinically apparent during a woman’s lifetime, or if it did, would not have shortened a woman’s life) ( Could my mother have been a victim of over-diagnosis?)
-
Radiation exposure (a real concern that should not be lightly dismissed by any woman)
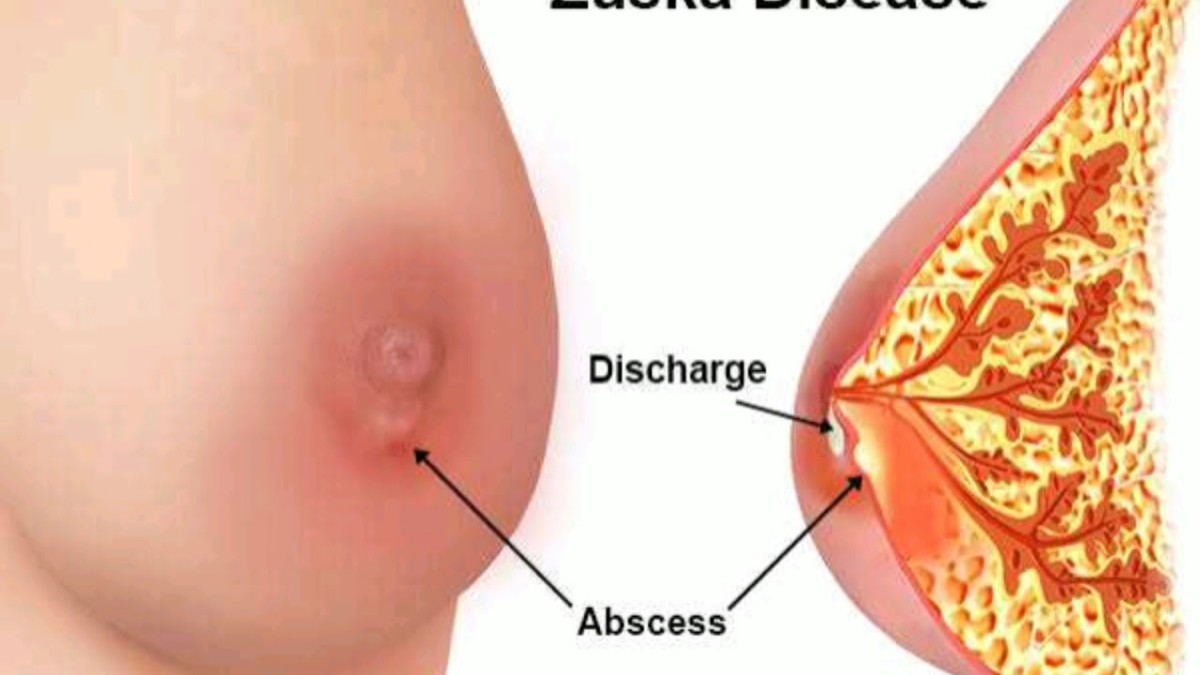
Left: Normal Breast Tissue Right: Breast Cancer
Thoughts From A Prominent Doctor
Dr. Susan Love, the recognized breast cancer expert, reacting to the uproar that resulted from the new mammography screening recommendations, said this:
The public anger at these recommendations is understandable. But it should not be directed at an honest effort to evaluate the benefit of mammography, but at the fact that we still don't know the cause of breast cancer or how to prevent it. Early detection is not our best prevention -- it's not even prevention. It just finds cancers that are already there.
Dr. Love went on to say that scientific thinking about breast cancer has changed over the decades. No longer can researchers visualize breast cancer as a disease that always spreads, inexorably and inevitably, toward a takeover of all the breast tissue and beyond. There are five varieties of breast cancer, some of them very aggressive and some that may not have the ability to spread (for instance, the DCIS type).
I think I understand what Dr. Love is saying, and it makes sense. Dr. Love has her own foundation dedicated to the eradication of breast cancer. She supports the position of public health experts while acknowledging that we still wish we knew more about this disease.
Dr. Love did not speculate very much on the causes of public outrage, only the results.
Patient Having a Mammogram
What Screening Has Come To Mean
I believe it was inevitable that many women, though not all of them, felt like pillorying the members of the task force. Think about it – how many years is it now that women have been exhorted to have the yearly screening mammograms? I had my first baseline mammogram at age 35, due to my family history, and one almost every year afterward.
For years now, we’ve seen the ubiquitous pink ribbons for breast cancer awareness. They are iconic on bracelets, hats, T-shirts, wristbands, and bumper stickers. October has been Breast Cancer Awareness Month for a long time. Americans have viewed countless images, innumerable personal stories, and plenty of public service announcements on television. The Susan G. Komen Foundation, right over in the next county from me, has done stellar work to bring awareness of this dread disease to women of every age.
But still we have the disease. And screening mammography, having improved over time with research funding, does catch some cancers. It is a simple, though painful, procedure that gives many women reassurance that they are doing something to help prevent breast cancer. Mammography is a quick test that doesn’t inconvenience women much. And it has become an entrenched, though far from perfect, technology that younger women will have a hard time giving up as our country moves to health care cost containment. This goes for any diagnostic test that’s been around forever.
In my opinion, a mammogram is pretty easy. A television ad gets your attention, and you go have the radiography done. Less easy is doing your own personal inventory to see how you can improve your lifestyle, and therefore, your chances of being cancer-free. Exercise definitely plays a role in prevention, as does diet. But try getting people to make a sweeping, permanent life change with just a jingle and a few media images.
How Radical Was This?
Lest I forget. In 1976, seven years after my mother’s breast cancer surgery, I was still seeing the same OB/GYN who was her physician at the time of her diagnosis.
He had me sit across from him in his office, and said, “There have been some intraductal changes in your breast tissue. I believe you should consult with a surgeon about the possibility of having a prophylactic mastectomy. If not, given your family history, you’re probably going to get breast cancer before age 40.”
Now, I’m not sure where he got such a guideline. Did he talk to colleagues or did he trust emerging research of the time? My family history is not terribly strong. Actually, I’m in the moderate risk category. And as the science later revealed , only women with the mutant genes BRCA1 or BRCA2 should consider a prophylactic mastectomy, and then, only after lots of soul-searching and extensive research. But at the time, I suppose it was more difficult to measure risk.
I’m glad I didn’t listen to that doctor. I am in my mid-fifties and I’ve never had breast cancer. Neither has my sister or any of our seven female cousins, who range in age from late 40’s to about age 60.
That anecdote just reveals how reactionary some doctors were about this terrible disease. That the recently revised guidelines from an expert panel provoked anger from some physicians is surprising in a way, since the guidelines were established using evidence-based medicine, a construct that is now prevalent in the curriculum of most medical schools. Apparently, evidence-based medicine should be trusted, but only when it doesn’t unsettle some of your pet notions.
What's In Store
Twenty years from now, neither breast cancer or any other disease will be treated the same way. The paradigm will have changed once more, and much of the research of the 20th century will reside in the archives of medical historians. I’m not going to wring my hands and nervously run in circles over such a simple change in screening guidelines. I don’t think the report’s timing had anything to do with the current health care plan being debated in our Congress, nor do I think the panel has conspired to deprive anyone of screening mammography who needs it. Personally, I plan to learn even more about disease prevention and how I can optimize my chances for good health.
And, I have made a decision to go for a mammogram only every two years.
Links
- Mammogram Debate Shows Why Reform Will Fail - Forbes.com
Why can't we control costs? Because experts who write perfectly reasonable guidelines get branded death panels. - Breast Cancer Screening Advice that Doesn't Make Sense | Psychology Today
Breast Cancer Screening Advice that Makes No Sense By Ira Hyman... - Screening for Breast Cancer: Recommendation Statement
Recommendations on screening for breast cancer from the U.S. Preventive Services Task Force (USPSTF). - Craig Bowron: Mammography Debate: Even Physicians Can Get Emotional About Science
Politicians are incapable of giving the public any bad news, and the insurance and health care industries care about profits. That leaves physicians and scientists to lead us through health care reform.
Hubs
- Mammography Controversy Screening & Homeopathy
THINGS TO THINK ABOUT ~ Check out the Anti-Radiation Bra Below Listen to the Diane Rehm Show Is this a Political Issue? Are Women the Guinea Pigs? Video: Watch Mammography Procedure ... - BREAST CANCER - Prevention and Tips for Natural Cure
. Are you among the women who avoid mammograms or you belong to the group that have routine mammograms? Are you doing regular self-exam of the breasts? On November 16, the US Preventive Services Task... - Breast Cancer Treatment - Things The Doctors Don't T...
I am 38 years old and was diagnosed with Breast Cancer 14 months ago. I have learned a lot while going through breast cancer treatment and I want to share my experiences and what I've learned that doctors don't tell you...