Diabetes, Peripheral Vascular Disease and Limb Amputations
Diabetes patients with peripheral vascular disease quite often present with infectious ulcers on their toes that won't heal, and often actual limb amputations are the only way to stop the infection spreading up their legs and killing them through systemic blood poisoning.
Back in the 1970s and early 1980s I nursed those people, and while limb amputations seems like the very worst thing that could happen to anyone, the relief the patients' felt knowing that the infection that had plagued them for months, if not years, was finally gone helped them on their road to recovery.
Not all of our patients had diabetes, but a huge percentage of them did. In those days they blamed smoking for causing their illnesses, and diabetes for causing complications.
I think we know now that diabetes caused not only their peripheral vascular disease, but the infections and sores that refused to heal which are also symptomatic side-effects of the diabetes itself.
What is Peripheral Vascular Disease?
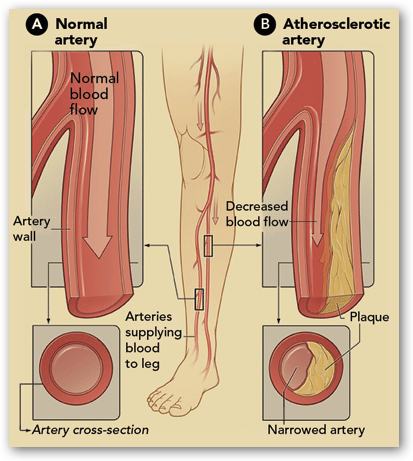
Peripheral vascular disease is the name given to a condition whereby the blood supply to the extremities is not sufficient.
Normally only the legs and feet are involved. Our hands and arms are not terribly distant from our hearts which pump the blood round our bodies.
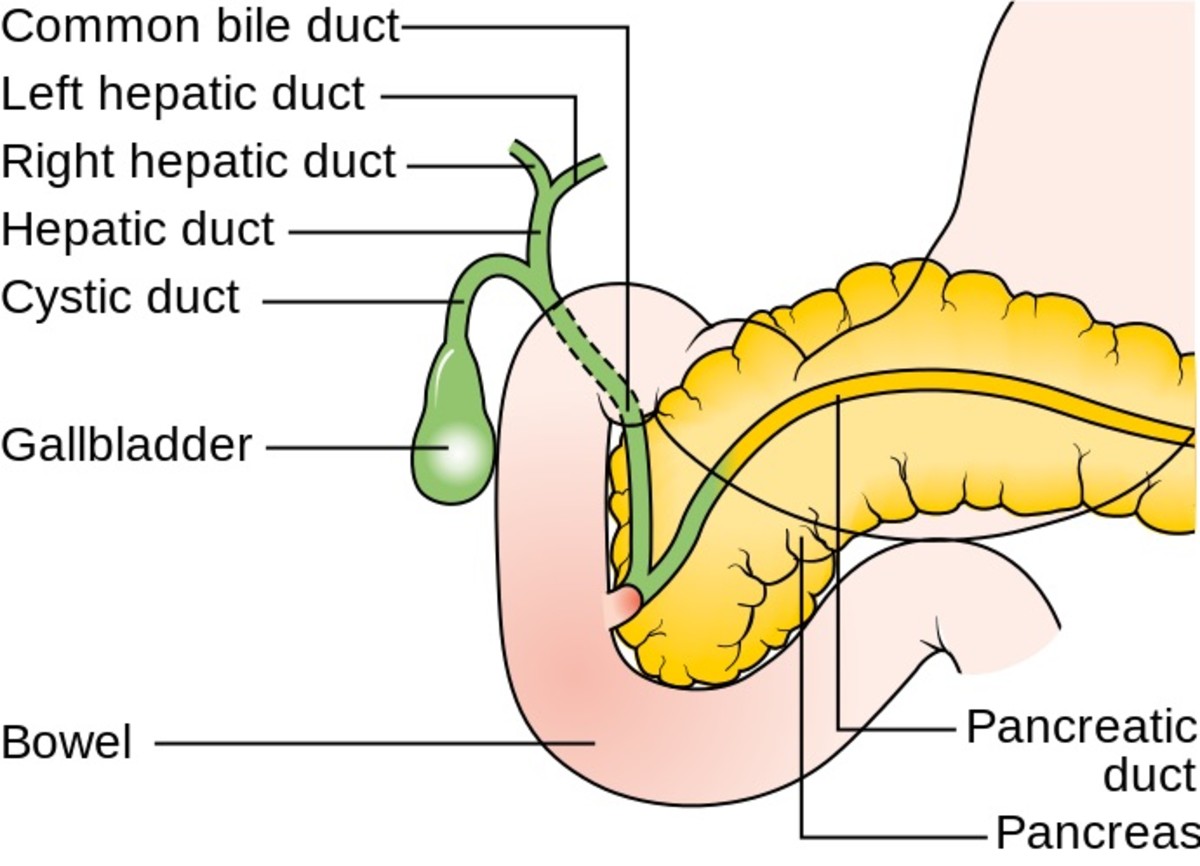
Arteries narrow as they are filled up with deposits, specifically the femoral arteries which run down each leg.
The blood backs up, and while it usually gets through, it leaves the patient with permanently cold feet, and what they call claudication on walking. Claudication is the name for the pains felt at the back of the calves when undertaking moderate exercise.
It is basically a leg cramp as not enough blood is getting through to satisfy an increased demand for oxygen.
It is those cramps, which can make walking very uncomfortable if not impossible, that eventually drives patients to see their doctor.

The doctor determines how severe the claudication is by carrying out various tests. One simple test is one we called 'the toe test'.
The patients hands were placed in basins of warm water, while both toes were clamped with an electrode that took automatic temperature readings.
The readings were monitored every few minutes, and at the end of the test, graphs showed quite a variation in the toe temperature of the affected leg, compared to the unaffected leg.
If the problem is severe, the patient may be referred to a surgeon for various procedures including the renewal of part of the femoral artery.
Post-operatively, these patients were prone to infections, more than the general population, because of their diabetes, but in the main, most people recovered well from this procedure.
Gangrene
The other type of vascular patient we got was the diabetic with the toe sore that would not heal - whether that was an ingrowing toenail or just from a sore that appeared one day and would not heal.
Quite often, by the time they were admitted to hospital, all treatments had been tried by their GP and district nurse, but gangrene had set in and it was our job to stop the spread.
If you have ever seen or smelt gangrene, it is not something you will forget in a hurry. I have never smelled a rotted corpse, but everyone who has will tell you the smell is very distinctive and not one you'd want to meet again.
I imagine it is similar to gangrene which occurs when human cells just rot and die.

Leg Amputations
Normally by the time our diabetic patients had been admitted to our large training hospital, they were already booked in for an amputation.
The surgeons always had the tricky job of deciding how much to cut away. They couldn't risk just taking half a foot away when only the toes were affected, because gangrene spreads so easily and also because healing is very much delayed in diabetes patients.
Normally their decision became either a below or an above knee amputation. They had to cut well up from the gangrene to ensure it didn't spread.
Many of these patients would not survive a second surgery.

While many patients recovered and went on to get new artificial limbs fitted, there were some whose wounds just wouldn't heal.
By this time I was working in a small hospital that was attached to the large teaching hospital, and so we saw the patients that came in for limb fitting as well as those with lingering infections.
We carefully cleaned and de-sloughed their wounds daily or more often if needed, and some did indeed heal after an extended period of time.
A very small percentage couldn't be healed, and faced surgery a second time, with a high mortality rate.
It was depressing for us because with them being long term patients we got to know them well. They felt like part of our family!
Many of our patients had severe diabetes - insulin dependent type 2 diabetes, whose diabetes couldn't be controlled with a strict diabetic diet alone.
If you are newly diagnosed with type 2 diabetes and are reading this, please do not be frightened.
I have written this so that you can know what to look out for.
Difficulty walking any distance without experiencing pain in the lower legs, having permanently cold feet (especially if it is only one) and sores on your toes that won't heal.
If you suffer from any of those symptoms, tell your doctor so that he can be on the look out for complications. Treated early, there is no need to assume the worst.
The most important thing you can do for yourself is to keep your diabetes under control at all times. Don't cheat with the diet. It simply isn't worth knocking your glucose levels up for.