In the Midst of a Ms Relapse - My Personal Experience

A Lengthy Exacerbation Has to Be Treated
Yes, right now as I type, I am undergoing a flare-up of my MS. Actually it has been going on for a couple of months at least, but being the pro that I envision myself to be, I thought I'd ride it out hoping it would reverse itself of its own accord. Well, it didn't!
You see we "pros" don't let every little problem get us all worked up. We know there are going to be good days and bad days, symptom-wise. We take it a step further by reminding ourselves there will even be bad weeks strung together that don't necessarily have to send us running to the neurologist for assistance.
For example, my mom passed away a year and a half ago. It was very stressful. I fully prepared myself for a flare-up and when it hit, I rode it out by resting and grieving and taking it easy with myself. It eventually passed and I regained what I temporarily loss.
Why I Stopped Chill-Laxing
If, I'm such a "pro", and have mastered the art of chill-laxation, why am I headed to the neurologist in a week? Frankly put, chill-laxing has not obtained the optimum results I had hoped for.
Every now and then, no matter how much I do, it just isn't enough and I must accept the fact that I too must do something I dread. In my case it will probably mean doing another 3-5 day pulse of mega-steroids and going through the wonderful roller coaster ride that is solu-medrol IV treatment.
I'll have to be up for days at a time, recover from the lack of sleep, yada . . yada . . yad . . but so be it, as my way has not worked.
I've managed to keep my MS at bay for about 3 years now, without any steroids. I knew it wouldn't go on forever, especially since I am not currently taking any injectables that slow down the progression of my MS. Statistically speaking, I'm ahead of the came. ( I injected Copaxone for 7 years, read about that experience in this hub.)
My Symptoms
Actually, that was me I described up above. Two opposite sides of the body- left arm, right leg. Two opposite body parts- arm and leg. One body part limiting my ability to function in a normal way for a normal amount of time. Of course, my "normal" bar is set much lower than a healthy person's bar, but even for me, my activity is greatly impaired and not improving.
When you rate the intensity of an attack you determine what you can do, how long you can do it, and whether or not the use or function is slowly getting better or not.
In my case, I seem to feel better for a day or so and think, "good, its going away" only to find it is back in a day or so and leaving me a little more depleted as time goes on. It has been so gradual for me that I underestimated my flare-up. If it wasn't for an e-mail I received to update my profile on a MS website I joined, I don't know how long it would have taken me to realize this flare has been going on too long.
Usually my bad flare-ups slap me in the face. POW! Its just there demanding my attention. Not so with this flare. It has been insidiously gaining ground on me, creeping along ever so slowly, advancing at an almost indistinguishable pace. Hard to spot when you look for galloping, attention-grabbing, in your face, sort of symptoms.
Thanks to my chart update, I recognized my decline from just a few months back. Asked if I have been able to care for normal duties and functions around the house, the answer is NO. Asked if I could walk unaided for a certain length, the answer again was NO. Hmmm, I thought, this flare-up needs my thoughtful attention, I've chill-laxed long enough.
The Definition of an Exacerbation
Now technically speaking, any non-sensory problem that lasts 24 hours or more is a flare-up or an exacerbation, or an attack, or even a relapse. You can pick the noun you prefer, I like flare-up.
So, excluding sensory issues such as numbness, tingling, burning, itching etc. and after determining you are not having a pseudo exacerbation, you may consider yourself in flare-up mode if what you are experiencing lasts longer than a day. (I'll cover pseudo flares in another article.)
Whether that sends you running to see your doctor is a horse of another color. Based on that criteria, I'd be making an appointment almost monthly, as I can easily exhibit symptoms for 24 hours or more on a monthly basis. No thank you. If I truly am experiencing a relapse and it lasts a couple of days or so, I know I can ride it out and not even remember it happened by the time it has eased up for a day or so.
But then again, I am a pro. Pro's learn to deal with a lot without reacting in a panicky sort of way. We've learned to chill-out or "chill-lax" as the late, Bernie Mac would say.
For a MS newbie, unused to the body acting in such unpredictable, unexpected, and unwanted ways, a symptom flare-up is scary and dreaded.
What does it mean? Am I going to totally lose a function? Is this the start of something that is cascading? If I do nothing, will I get sicker?
Not to mention when a newbie has to endure a loss of function in totally unrelated areas of the body, say a weakness in the left arm and a left hand tremor, in addition to weakness in the right leg, which prevents standing for longer than 15 minutes at a stretch.
Putting yourself in the place of someone newly diagnosed with MS, can help you to understand why they may feel shall we say, tense, right? So it is totally understandable that it will send them running to their doctor or neurologist to get the flare-up analyzed.
Quite frankly, I think it is the correct decision, since a newly diagnosed person needs to be tracked to determine with as much certainty as possible, what type of MS they have.
You Know You're In A Flare When . . .
You know you're in a flare when you call your doctor and you get a quick appointment. Usually neurologists, especially MS centers are booked all the time. You have to wait anywhere from 1 month to 6 months to get a follow-up appointment. That changes when you describe symptoms indicating a flare, then you get pushed to the front of the list and get the next open spot, or cancellation. When I reported my leg weakness and problems standing and walking, I was given a cancelled spot and told not to miss it because the doctor was booked until November. I was told I was probably in a flare since I was having trouble walking and that she wanted to make sure I got in as soon as possible.
She even apologized that she couldn't get me in sooner. That's another clue you are in a serious flare. Caring and knowing professionals understand your symptoms are no little deal, and get you in ASAP.
I'm Not Scared
I guess that's the "pro" in me. I've been more incapacitated than this, in the past. My first experience was terrifying for me. I have a fear of losing the use of my legs and when it first occurred I thought, "Oh no, here it comes!" However, I've seen the lesion heal, and although it is still there, it becomes inactive to the point that it doesn't affect me all the time. As long as it stays that way, I think my leg function will be OK. Of course I can't become overconfident and ignore obvious signals that the lesion is active again. I know it is active again right now, so whether I want to or not, I've got to follow my neurologist's recommendation which will probably be to get the inflammation down, by an IV of solu-medrol.
More on Causes of Flare-Ups
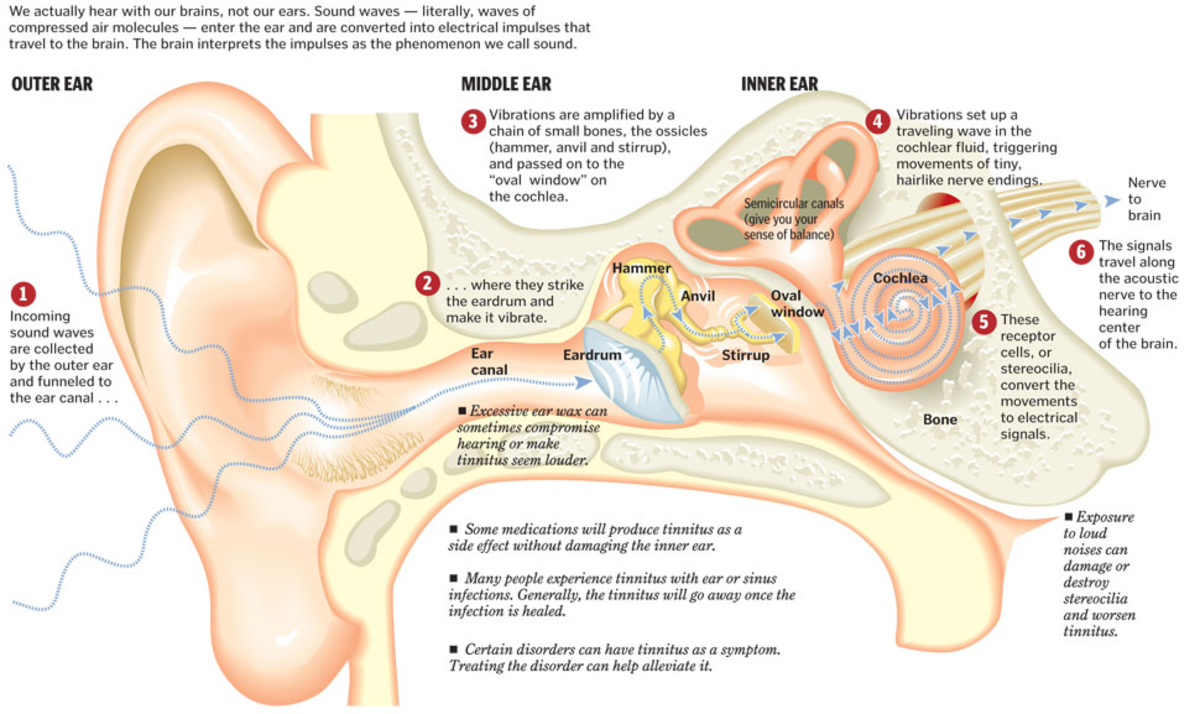
Flare-ups boil down to inflammation of the CNS (Central Nervous System). This swelling or inflammation damages the myelin (the protective covering of the nerves) which slows or disrupts the transmission of nerve impulses and causes symptoms of varying degrees at varying locations.
That is quite a mouthful, but it just means any body part or muscle controlled by nerves can be attacked at any time for any reason. The longer your initial symptoms last, the better the chance the symptom will remain with you for life. Which is why newbies are urged to get on an injectable as soon as possible, to slow down disease progression.
Since every part of the body is controlled by nerve impulses from the brain down the spine to the muscles and nerves controlling the muscles, every part of the body is up for grabs.
That reality is disconcerting, but you know you have gained "pro status" when it doesn't keep you up at night, thinking about all the what ifs.
What's Next For Me
Well like I said, I'm off to my neurologist next week, where I will be given a thorough exam to see what I can and cannot do, and how my reflexes are holding up. He'll take a history of this flare, no doubt tell me I need to be on something. I'll remind him I'm waiting for the pills to be approved by the FDA and let him know that steroids have always helped me. He'll probably agree that I should do a pulse and I will then be set up with my Home Nursing Care institution for the steroids. Of course there is always the off chance he will just give me a whole bunch of steroid pills to take, I wouldn't mind that at all.
Whichever he decides, this time I'll write about it from the time the script is sent out until I have finished the process, that way anyone wondering what it is like will have all the details.
I will be continuing this subject in a new series of articles designed to cover the initial visit with my neurologist, right on through each day of my steroid use. It will therefore be at least a 4-part series.
Please click here for Part One.