Prevention Of Tetanus (Lockjaw) And A Review On Other Clostridial Diseases
Antitetanus Vaccine Administered On A Child

Prevention Of Tetanus
Tetanus is an easily preventable disease. Clinical tetanus does not confer immunity and therefore the patient should be actively immunized when he recovers. Three subcutaneous injections of adsorbed toxoid in a dose of 0.5ml at monthly intervals produces lasting immunity. As a part of the total immunization program for children, the first dose may be given as the DPT vaccine at the fourth month of life and two further doses at monthly intervals. If the full course of DPT vaccine is given, the child gets life-long immunity. Boosters are needed once every 5 to 10 years. When severe injuries are sustained, one dose of 0.5ml ot toxoid may be given as a precautionary measure. Passive immunization can be achieved in non-immunised subjects by the administration of 250 IU of TIG or 3000 IU of ATS after test does. The immunity lasts for about two weeks. Passive immunization is given along with a booster does of toxoid in separate syringes at different sites to non-immunised individuals who sustain injury. Active immunization of pregnant women ensures adequate antibodies in the neonate and prevents tetanus neonatorum. Primary care of the wound like surgical toilet and penicillin therapy considerable reduce the risk of tetanus.
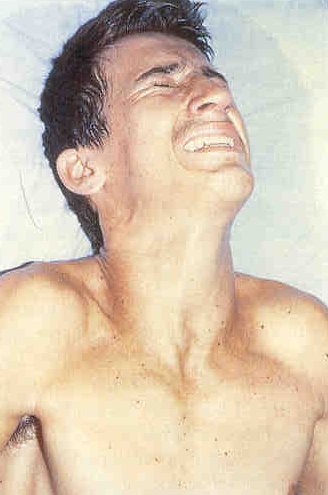
Tetanus Manifestations
Infectious Diseases
Gas Gangrene (Clostridial Myonecrosis)
This disease is caused by several clostridia which grow symbolically with a mixed bacterial flora. The main pathogens are Clostridium welchii (60%), C. edematiens, C. septicum (20 to 40%) and rarely C. histolyticum.
Pathogenesis: Necrosis of tissue brought about by anoxia, ischemia or injury is complicated by clostridial infection which may be exogenous (introduced along with the wounds) or endogenous (derived from the intestinal tract). The organisms multiple locally and produce toxins which diffuse out and lead to generalized toxemia. The affected tissues are avascular and appear as if cooked.
Clinical features: After an incubation period of 1 to 4 days, the wound becomes swollen and tender and exudes brownish foul-smelling fluid. Due to the presence of gas, crepitus may be felt. Blebs filled with purplish foul-smelling fluid develop. These blebes reputure and ulcerate. General symptoms such as restlessness and fever develop and the patient may rapidly go into shock and anuria.
Diagnosis: The condition has to be diagnosed clinically. The organism can be identified by culture. X-ray of the affected part shows gas in the tissues. Gas in the tissues may occur in other conditions such as surgical emphysema and infections by streptococcal, staphylococci and E.Coli.
Treatment: Early institution of therapy is most important for success. Shock is treated on the lines of septic shock. Penicillin which is the drug of choice is given intravenously in a dose of 2 mega units, 2-hourly. Other antibiotics may be tried depending on the sensitivity tests. Antitoxin is available for intravenous used (anti-gas gangrene serum- AGGS). It should be given in a dose of 40,000 units initially to be followed by 20,000 to 40,000 units repeatedly till the condition improves. Keeping the patient under hyperbaric oxygen (3 atmosphere pressure) remarkably improves the result of therapy and this should be instituted wherever it is available. Surgical excision of dead tissue and removal of foreign bodies should be undertaken after administration of AGGS. Gas gangrene can be prevented by taking proper care of the wound and early recognition of the condition.
© 2014 Funom Theophilus Makama