What are the Effects of Antibiotics on Good Microflora
Microflora
Microflora is a generic term for the microbes; bacteria, fungus, and
viruses. Every human born both acquires beneficial microflora from
their mothers and/or picks them up in the first few months of life.
These microflora are vital to human health.
Scientists know that an adult human being has about ten trillion living cells. An additional hundred trillion cells are these acquired germs and make up the bacteria, fungi, and viruses that every human being plays host to. These "foreign" cells are collectively referred to as microflora.
Microflora live both within us and on our skins. Often taking up space that harmful or damaging germs would otherwise occupy. In so doing microflora actually lend a hand in protecting human health by being hostile to invading germs or simply by occupying (and fighting off invaders) space that would otherwise be populated by toxic or damaging germs.

Beneficial Germs
Since the microflora in humans have evolved right along with us, they act in beneficial ways. Some aid our digestion, others act as barriers to outside disease, others still help fight off foreign or invading microflora.
This is all well and good, but what happens when some of that microflora are wiped out?
The Health Hazards of Antibiotics
Health scientists already know that in some circumstances a rigorous course of antibiotics will kill all bacteria, even the 'good' ones. In some situations, Candida albicans, a fungus typically present in the gut, but kept in check by other microflora, can take over the formerly occupied space and cause serious health problems...even death.
Other times, a rigorous course of antibiotic treatment can kill all but the most hardy germs. This too can have a negative effect. Making the human undergoing the treatment a breeding-ground for virulent germs that are antibiotic resistant.
Because the conditions these microflora thrive in cannot be recreated in the lab, healh-science has yet to classify all of the microbes we live with. In
short, science does not yet know all of the bacteria occupying inner
human space nor does it understand the role each of these might play in
the overall health of the human body. Further still, without a good "roadmap" to all of the microflora present in the human body it's impossible to determine how they interact with each other and protect the host....us.
Despite this lack of knowledge,
it is quite possible that most of the bacteria we are born with are not
only not harmful, but might be downright beneficial to a healthy life. As with the case above, by occupying a niche in our bodies these microflora crowd out or deny space to harmful viruses, bacteria, or fungus.
Antibiotic Effect

Antibiotics: Staph & Tuberculosis
In the recent past antibiotics have been over-prescribed1 leading to versions of tuberculosis and staph that defy all attempts to kill them. This development is the direct effect of antibiotics that are prescribed such that they do not kill all of the bacteria present. This in turn leaves only the strongest version of these two germs alive while killing off the weakest 99%. Of course the remaining 1%, able to withstand almost any anti-biotic, survives and reproduces...with devastating results.
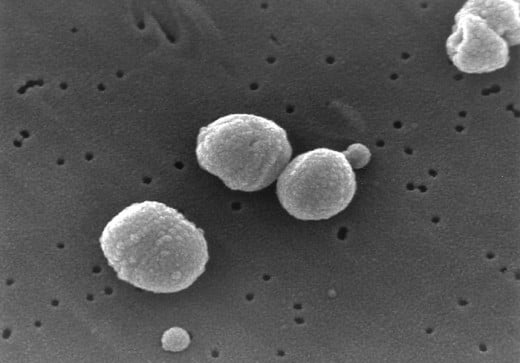
Methicillin-resistant Staphylococcus aureus
(MRSA), is a bacteria that has become resistant to all current forms of
antibiotic. In fact, the number healthy people contracting this untreatable
bacterial
infection have reached frightening proportions. In 2007 Monina Klevens
at the Centers
for Disease Control and Prevention found that 19,000 deaths were caused
by MRSA. in the United States. To put this figure into perspective this is
more deaths than those attributed to HIV/AIDS. That means that 20% of
those who contract MRSA die from it. A staggering figure.
Other bacteria, notably Helicobacter pylori, when found in "reasonable amounts" the human host, has been linked to reduced incidents of asthma and skin allergies. That H. pylori has been disappearing in the human population might be at least partially responsible for the increased number of people suffering from allergies. Also, because H. pylori is linked to the production of the hormone ghrelin, the death of this bacteria may also be responsible for the increase in the number of obese people in the U.S.
Ghrelin helps to regulate both fat development and hunger.
On the flip-side an overabundance of H. pylori has been linked to intestinal inflammation and ulcers. It has also been implicated in the reduction of stomach acids and stomach cancer.
Streptococcus pneumoniae - Pneumonia Infections
A vaccine for the treatment or prevention of pneumococcal disease has been a success. The vaccine has drastically reduced the number of cases of pneumonia and infection.
However, streptococus pneumoniae is not only present in every human alive, it is also a direct competitor to staphycocus aureus....including the strain that is resistant to antibiotics.
In short the loss of the pneumonia causing bacteria is giving the staph bacteria a space to grow and flourish.
Allergies and Hygine
Improved sanitation and the large number of cleaners currently available have likely saved thousands of lives. They may even have made the rest of us healthier and extended our lives.
But microbiologists are finding benefit to the "dark side" of cleanliness. Those microbiologists who support this view assert that over-cleanliness has resulted in a substantial increase in the number of people who suffer from allergies. One line of research indicated that pregnant lab mice2 exposed to "barnyard dirt" gave birth to pups with a greatly reduced incidence of allergies and asthma.
Possible Solution: Targeted Antibiotics
Antibiotic: A substance or compound that kills or inhibits the growth of bacteria.
The definition above indicates that "antibiotic" is a generic term not solely reserved for those drugs based on methicillin or it's derivatives.
Because
"broad-effect" antibiotics have such a negative effect on our symbiotic
bacterial health, killing all bacteria; both good and bad, health science is now looking at antibiotics and vaccines that
stop short of killing the offending germ. They are also researching antibiotics and/or vaccines that target just one specific
germ. The idea is to prevent the strongest of the offending germs from surviving the course of treatment and then proliferating.
With the advent of AIDS and the research created to stop the disease, much has been learned about viruses, bacteria, and other microflora. One lesson learned is that it's possible to simply deny a harmful germ the elements it requires to reproduce. So, rather than killing the offending germ, it's simply prevented from replicating. This method works on all versions of the germ, including those that are strong enough to survive a course of antibiotics.
In stopping short of killing the microflora health science can simply cause the offending germ to stop reproducing without actually killing it. This helps prevent a rebound effect from the one percent of germs that survived the attempt to kill them off.
The other alternative is to create a vaccine or antibiotic that kills only one particular germ and no others; with the same net effect, no rebound.
Coda
Because so much of the microflora within the human body cannot be properly studied directly, scientists are currently using a "black box" model. In other words the effects on the overall system, the human body, are noted when changes to the microflora occur. When changes occur to the microflora the effect to the entire body is logged and studied.
Disclaimer
The author has not been compensated monetarily, via discounts, or freebies for the contents of this article.
The author may be compensated for attached ads, the contents of which the author has no control over.
Footnotes
1Of course, doctors did not know at the time that they were over-prescribing. That revelation is a recent development.
2 Typical lab-mice are born, weened, and raised to adulthood in a bacteria free environment. This means that the mice themselves are microflora free.