Types of Breast Carcinoma - General Introduction
Pre-malignant Breast Disease - ADH/DCIS or ALH/LCIS
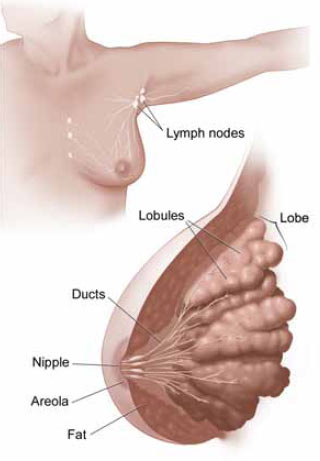
Premalignant breast lesions are the one which have potential to turn into frank malignancy if untreated or un-resected surgically. Turning into malignancy means that the breast disease that was confined to the bounds of a duct within the breast glands had now broken its limits and had invaded into the surrounding connective tissue or fibroadipose tissue of the breast parenchyma. If all this sounds too alienated then let me start with the basics. Developmentally or embryologically, breast is considered a modified apocrine/eccrine gland tissue, which is equivalent to the sweat glands in the skin. The biological reason for breast development is to provide nourishment to the new born in the form of milk. Therefore, the two important components in the breast are.
1. Secretory system
2. Supporting system
The secretory system is composed of cells which help in formation of milk and are called acinar cells. Many groups of acinar cells forms a terminal ductal lobular unit (TDLU) and many TDLUs together form a lobule which drains into a biological conduit or a duct, leading to the way out through the microscopic orifices at the nipple. The supporting system is the fibrous tissue and fat in between the lobules. The interesting part is that both the major components have chemical and molecular cross talk with each other, which determines the development of breasts and response to the hormones, in particular estrogen and progesterone.
The premalignant lesions arising from the secretory ductal system are called "Ductal Carcinoma In-Situ or DCIS" and the ones arising from lobules are called "Lobular Carcinoma In-Situ or LCIS". Now there are two nearly ambiguous terms which are ADH or atypical ductal hyperplasia and ALH or atypical lobular hyperplasia. These two terms are used in pathology diagnosis when qualitatively the histology of lesion looks pre-malignant but there is not enough quantity of disease to classify it as frankly premalignant lesion. For example in ADH the cells look like that of DCIS but the number of bad cells is less than that required to classify something as DCIS. Importantly ADH and DCIS will have different types of treatments as well as different disease outcomes.
There is very good link for the risk assessment of breast carcinoma based on various risk factors.
Types of Breast Carcinoma
The two most common variants of malignant breast disease are the one arising from the ductal unit and the other group arising from the secretory cells of the acinar system. Both the malignant diseases are clubbed under the common broad category of adenocarcinoma.
The one arising from duct is called "Invasive adenocarcinoma - Duct type" and the one arising from the lobule is called "Invasive adenocarcinoma - Lobular type". There can be adenocarcinomas with duct and lobular features and in that case the tumor is called "Invasive Mammary Carcinoma - Mixed type".
In general, adenocarcinoma is the term applied to the cancers which arise from the epithelial cells lining the glands and duct systems in human body. When looked under the microscope by the trained eyes or Pathologist, these lesions are easily picked up and accordingly classified. The classification done by the pathologists will eventually help the oncologist in deciding the type of treatment, follow-up, prognosis, molecular studies to be done and genetic counseling. Therefore, a lot depends on the expertise of your breast pathologist in looking at the MRI guided or ultrasound guided core needle biopsies or lumpectomies. I think that patients should be encouraged to discuss their biopsy results with the Pathologists. This can greatly help in reducing the anxiety associated with all possibilities of ruling out malignant disease.
Other uncommon variants of malignant breast lesions can be Phyllodes tumor or cystosarcoma phyllodes. This is most commonly considered as a borderline malignant disease because it usually does not metastasize to distant organs or lymph nodes but have high incidence of recurrence if incompletely excised. One of the very uncommon but highly malignant breast tumor is called metaplastic carcinoma which have malignant components derived from supporting stroma as well from the ducts. It is more like a mixed variant of highly malignant disease, unfortunately with very poor survival. Diagnosis is most commonly made by biopsy and doing further special studies on the biopsy itself.
What is meant by TNM staging and how it is done?
TNM staging is the evidence based classification of the extent for any malignancy. The staging system is provided by American Joint Committee on Cancer (AJCC) for stratification of patients based on their outcome/prognosis.
[T] stands for tumor characteristics, which are generally the tumor size and whether the tumor is confined or have locally spread into the adjacent tissue, skin and chest wall.
[N] stands for nodal or lymph node involvement by the tumor. N is given different subscript numerical values based on the size of lymph node metastasis, number of nodes involved, laterality of the nodes, anatomical location of the nodes draining the breast and extra-capsular spread beyond the anatomical confines of the particular lymph node.
[M] stands for distant metastasis. It is in two forms [Mx] which is no metastasis after extensive radiological and clinical work-up and [M1] which means that breast carcinoma have spread to distant organs such as brain, lungs, bones, liver, spleen or ovaries etc. Note that metastasis to the lymph nodes under the definition of [N] category are not considered distant metastasis.
Following is how the TNM classification of breast looks like. (Source AJCC and National Cancer Institute). It might look very complicated but it is a crucial factor in deciding the treatment and prognosis. This is routinely done and extensively discussed by every oncologist and pathologist with expertise in breast cancer. Please feel free to ask questions or comment.
T0 (Zero): No evidence of primary tumor.
T1a: Carcinoma in situ (Premalignant lesion).
T1: Tumor size is less than or equal to 2 cm. T1a >0.1 to 0.5 cm; T1b >0.5 to 1 cm;T1c >1 to 2 cm.
T1m1c: Microinvasion of 0.1 cm or less.
T2: Tumor size greater than 2.0 cm but less than 5 cm
T3: Tumor more than 5.0 cm in greatest dimension
T4: Tumor of any size with direct extension to (a) chest wall or (b) skin. The structures included in chest wall are ribs, intercostal muscles, and serratus anterior muscle but not pectoral muscles (flap muscles two types pectoralis major and pectoralis minor).
T4 is further subdivided into T4a to T4d : T4a: Extension to chest wall; T4b: Edema or ulceration of the skin of the nodules confined to the skin same breast; T4c: Presence of both T4a and T4b features; T4d: Inflammatory carcinoma - The diagnosis is made clinically when there is mass lesion and the breast skin is tense, red and looks very warm. This is due to the obstruction of specialized blood vessels called lymphatics by the microscopic tumor clots.
The [N] or nodal attribute is grouped as follows:
NX: Regional lymph nodes cannot be assessed because they might had been very small or previously removed by surgical procedure.
N0: No regional lymph node metastasis(tumor deposits in the lymph node are not seen on pathology slide)
N1: Metastasis to the underarm (axillary) lymph nodes on the same side as that of the tumor and the nodes are not adherent to the fat and therefore can be moved under the skin during examination.
N2: Metastasis to same side axillary lymph node or multiple nodes which are fixed to each other or to other structures and are therefore not movable during examination.
N3: Metastasis to same side internal mammary lymph node(s). These nodes are located alongside the chest bone or sternum.
The [N] status is further sub-classified when looked under the microscope and that makes it further important and complicated. I will not discuss the [pN] (attribute "p" is for Pathology) classification here since it will make the understanding more complicated.
Finally [M] or metastasis is classified as:
M0: No distant metastasis identified
M1: Distant metastasis present (includes metastasis to same side nodes located above the collar bone or supraclavicular lymph nodes)
Earlier a term called Mx, which means MX: presence of distant metastasis cannot be assessed. However, recently there had been recommendation to not use this term.
Conclusions
I have tried to make this article as simple as possible with respect to the important clinical and pathological classification, which have significant impact on the treatment and outcome of the individual cases. Every case is different and is looked at from different patho-physiological points of view. Some cases will respond to the empirical therapies and other might need neo-adjuvant treatments. It is beyond the scope of this article to discuss the entire scenario and management protocols. I will like to discuss more and invite you to give me some suggestions on what you may like to hear more on. The further work-up in breast carcinoma cases is an extensive multidisciplinary approach which includes pathology, oncology, radiology, molecular studies, radiotherapy and genetic counseling based on the type of mutations involved. Early screening and biopsy have helped a lot in picking up this dreaded disease in its very early stage of evolution. This have helped in early treatments and almost complete cure.
Recommended links and readings
Here are some of the recommended books on general awareness about breast carcinoma.
Dr. Susan Love's Breast Book, 5th Edition by Susan M. Love MD
The Breast Cancer Survival Manual, Fifth Edition: A Step-by-Step Guide for Women with Newly Diagnosed Breast Cancer by John Link
Breast Cancer Husband: How to Help Your Wife (and Yourself) during Diagnosis, Treatment and Beyond by Marc Silver