What is Restless Leg Syndrome?

Willis – Ekbom Disease, better known as restless leg syndrome, has become increasingly more common among the population.
It is estimated that approximately seven to 10 percent of the population is affected, and 2.7 percent of those with the disease have severe or daily symptoms. Women are more commonly affected than men.
Despite its name, restless leg syndrome (RLS) can also affect the arms and torso of the body. It is a neurological disorder that causes the irresistible urge to move the legs in response to a sensation that is very uncomfortable. Moving the leg temporarily provides relief from the very odd and uncomfortable sensation, which gets progressively more intense until the individual finally moves the leg. Unfortunately, the relief is short lived, and relaxing actually makes the symptoms worse.
In March 2011, a study was published in the journal Sleep that suggests there are fewer dopamine transporters (DATs) in the striatum of the brain of those people with RLS than those without the syndrome. Although these findings won’t help in diagnosing patients, nor do they give a definitive cause for the disease, but they may prove useful in treating patients with RLS.
Restless Leg Syndrome Symptoms
The sensation of restless leg syndrome varies widely among patients. Because of this the National Institute of Health has developed a set of criteria to help doctors diagnose patients with RLS.
The National Institute of Health states the criteria for RLS includes:
- A need to move the limbs usually accompanied by an uncomfortable or painful sensation.
- The uncomfortable sensation tends to improve with activity. Many patients find relief when moving the affected limb(s) and the relief continues as long as they are moving. In more severe RLS this relief of symptoms may not be complete or the symptoms may reappear when the patient tries to remain still.
- Sensations and the need to move gets progressively worse the longer the patient remains still.
- Symptoms are usually worse at night. Patients with mild or moderate RLS show a clear circadian rhythm to their symptoms, with an increase in sensory symptoms and restlessness in the evening and into the night, making sleep difficult.
In my own experience, the sensation is an uncontrollable urge to move my legs that continues to increase in severity the longer my legs are still. It comes on suddenly, and can last anywhere from a few minutes to a few hours. There have been occasions where the symptoms have disrupted my sleep. The symptoms are not only painful, but also very frustrating and distracting.
Individuals with RLS typically also have myoclonic jerks when sleeping, which can cause sleep disruption. These myoclonic jerks (as well as RLS) are part of a sleep disorder known as periodic limb movement disorder or PLMD. Interestingly, approximately 80 – 90 percent of all individuals with RLS have periodic limb movement disorder.

What Causes Restless Leg Syndrome?
Unfortunately, the exact cause of the condition is unknown in the majority of cases. There are a number of conditions that restless leg syndrome has been associated with including:
- Obesity
- Smoking
- Nerve disease
- Anemia (iron deficiency)
- Diabetes
- Kidney failure
- Polyneuropathy
- Pregnancy
One of the major conditions associated with RLS is pregnancy, which suggests that RLS is associated with circulation.
Patients with varicose veins also have a higher incidence of restless leg syndrome than those without them. Varicose veins are caused by poor venous circulation, and they are most commonly found in the legs; however, they can be found in the arms and other areas of the body as well.
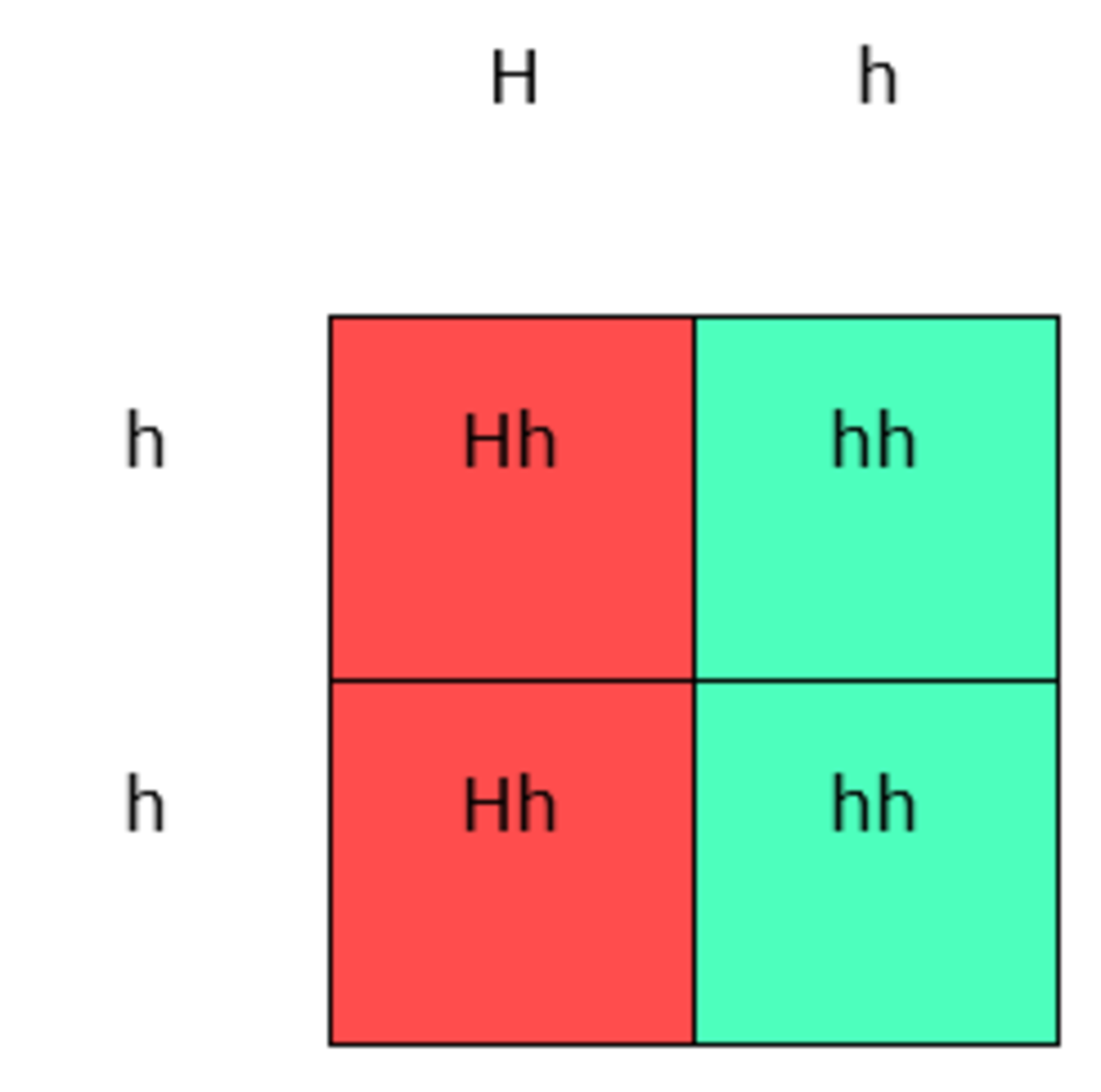
Restless legs syndrome can also be inherited. An estimated 50 percent of those with RLS have family members who also have the syndrome.
Have you or someone you know been afflicted with Restless Legs Syndrome?
Restless Leg Syndrome Treatments
Depending on the cause of RLS, there are a number of different treatments. If the condition is caused by an underlying problem such as anemia, diabetes or kidney failure, treating this condition often resolves the symptoms.
For those patients who do not have an underlying condition causing their symptoms, there are several medications that can help alleviate both the frequency and severity of the symptoms, many of which are used to treat other conditions such as Parkinson’s disease. These medications include:
- Requip (ropinirole)
- Mirapex (pramipexole)
- Sinemet (carbi/levodopa)
- Neurontin (gabapentin)
- Klonopin (clonazepam)
- Halcion (triazolam)
- Lunesta (eszopiclone)
- Ambien (zolpidem)
- Rozerem (ramelteon)
- Restoril (temazepam)
- Sonata (zaleplon)

Pain medications, specifically opioids such as Oxycontine (oxycodone), Ultram (tramadol) and Vicodin (hydrocodone) have been used to relieve the pain associated with RLS symptoms. Unfortunately, they do not decrease the frequency of the symptoms.
There are some medications that may worsen the symptoms of restless legs syndrome. Medications such as antidepressants and anti-emetics (anti-nausea) drugs have been known to increase the severity and frequency of symptoms and are best avoided if at all possible.
Alternative Treatments for Restless Legs Syndrome
For pregnant women, medication is typically not an option. If you are pregnant, or simply prefer natural methods for relieving symptoms, there are a few things you can try at home.
- Baths and massages – the warm water of a bath can help the muscles of the legs (or arms) relax as can massaging the affected limbs.
- Applying hot or cold packs – some patients have found the application of either heat or cold (or alternating the two) can relive the sensations in the limbs.
- Over-the-counter pain relievers – ibuprofen or Tylenol can be helpful in treating painful symptoms.
- Exercise – working out increases endorphins in the brain, which are the body’s natural painkillers. Regular exercise can reduce the frequency and severity of symptoms; however, too much exercise may have the opposite effect.



- Meditation or Yoga – stress exacerbates most health problems, and we all know it causes a multitude of them. RLS is no different. Meditating or practicing Yoga may help alleviate stress in turn alleviating RLS symptoms.
- Get a good night’s sleep – establish a sleep routine, and make sure you’re getting enough quality sleep. Keeping a sleep diary can help you monitor your sleeping patterns, and there’s definitely an app for that.
- Avoid caffeine – or at least cut back on it. Some patients have reported improvement in their symptoms after drastically cutting back on their caffeine intake.
- Avoid tobacco and alcohol – both of which can wreak havoc on your circulation among other things.
- Make sure you’re getting all your vitamins – the majority of the population doesn’t get enough vitamins through their diet and supplementation is necessary. Vitamin C and vitamin E have been reported to help alleviate symptoms.
There are also several minerals that have been reported to help alleviate RLS symptoms. Magnesium, potassium, and calcium are all required for neural signaling to the muscles (among other things). A deficiency in one or more of these minerals may trigger RLS.
Coping with Willis - Ekbom Disease
Realizing you are not alone and that there are other people out there dealing with the same symptoms can go a long way to helping you cope with RLS. Join an online support group, and talk to others about your condition.
Don’t be afraid to seek help. Many patients avoid visiting their doctor for fear of having to explain a symptom that is inherently indescribable, but RLS has received quite a bit of attention by the medical community in recent years. Most doctors now accept RLS as a legitimate condition, and if they don’t, it’s time to find another one.
This content is accurate and true to the best of the author’s knowledge and does not substitute for diagnosis, prognosis, treatment, prescription, and/or dietary advice from a licensed health professional. Drugs, supplements, and natural remedies may have dangerous side effects. If pregnant or nursing, consult with a qualified provider on an individual basis. Seek immediate help if you are experiencing a medical emergency.
© 2013 Mel Flagg COA, CPT, CHC, CNC