Lymphedema Prevention and Lymphedema Management After Breast Cancer
This article is about lymphedema prevention, and lymphedema management after breast cancer. I have previously overviewed this topic in my hub, Post Op Management Strategies After Mastectomy, which summarized what I learned as an occupational therapist working with clients after mastectomy and lumpectomy.
What is Lymph and Lymphedema?
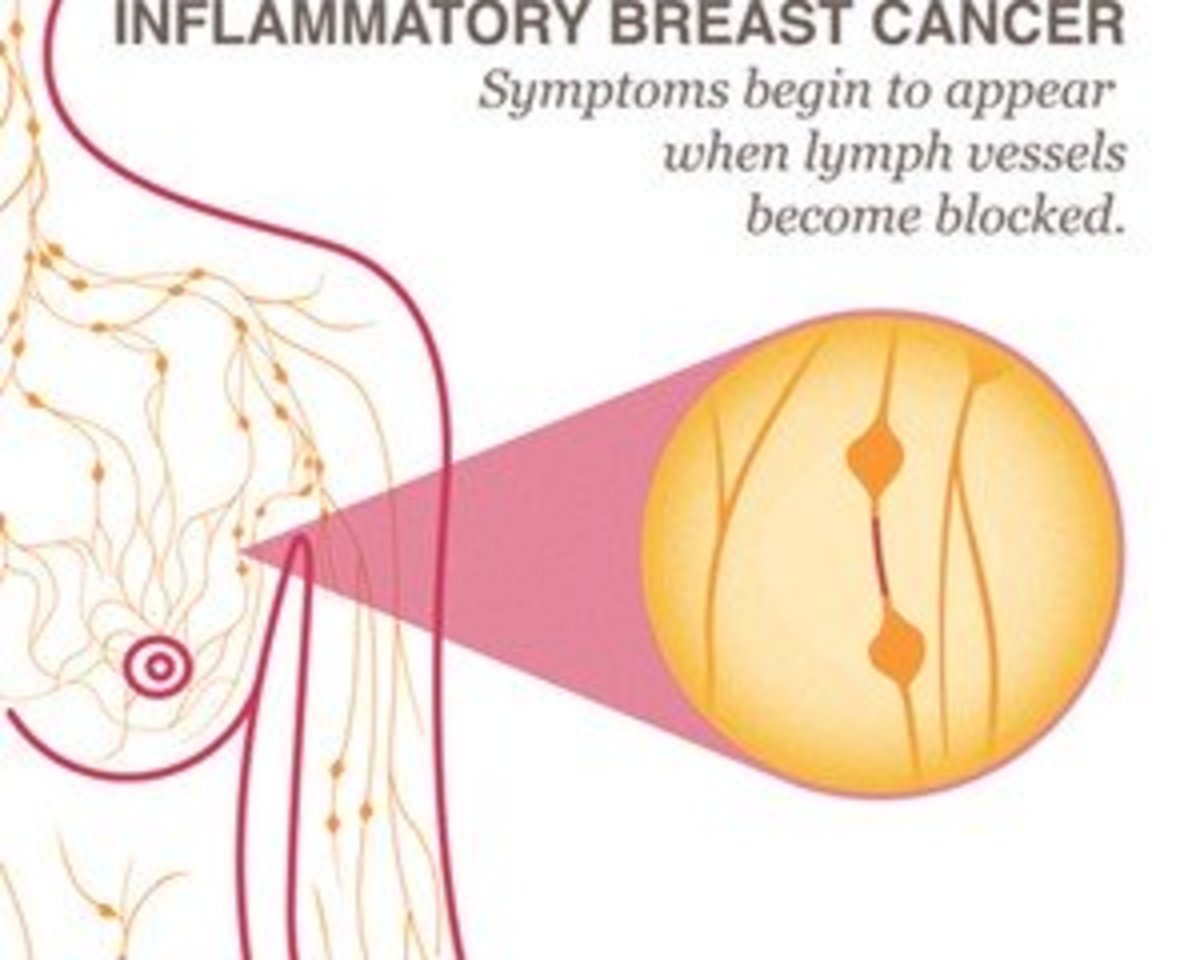
Lymph is a body fluid which acts as a scavenger to remove potentially harmful materials from the body. The fluid collects in the vessels of the lymphatic system, not unlike blood flowing through the circulatory system. Lymph nodes filter and process toxins before returning lymph fluid back to the blood stream at the subclavian veins (for upper extremities). The lymphatic system is crucial to immune function and circulation.
On their website, the Mayo Clinic says “lymphedema is caused by a blockage in your lymphatic system…The blockage prevents lymph fluid from draining well, and as the fluid builds up, the swelling continues.” I would propose that in some cases, the lymphatic system is not so much blocked, as it is overwhelmed. As swelling progresses, the normal function of the system is further compromised.
The result of compromise to the lymphatic system is lymphedema, which manifests as persistent swelling of an extremity. In the case of breast cancer, this is usually the side of the mastectomy or lumpectomy.
In general, lymphedema results from known trauma. A severe shoulder injury from a car accident is traumatic to the arm and chest. I have seen this in my clinic. One client had a shoulder injury from a motorcycle crash. He needed surgery, which was delayed for a week due to massive swelling of his arm. At the point I saw him, it had been a month since his accident, and his chest and entire arm were swollen and hard. I referred him to a local physical therapist who specialized in lymphedema.
An insect or spider bite can be traumatic to an arm or leg. Insect bites are often presumed when a client develops lymphedema that cannot otherwise be explained.
Surgical removal of a breast is a lot of tissue trauma. Add to this the removal of lymph nodes. Now we have a compromise to the lymphatic system, and a reduction in the number of filters for the fluid collected by our scavenger system.

Relative Risk Levels for Lymphedema
Over time, I developed my lymphedema risk levels, based on experience, logic, intuition, and collaboration with a local compression garment fitter. If you find something better, I’m all eyes and ears.
As a general rule, I would say risk of lymphedema would be lower after lympectomy than after mastectomy, simply based on tissue trauma. Mastectomy and reconstruction done at the same time is a tremendous amount of tissue trauma.
The big players in lymphedema risk however are the lymph nodes. The more nodes removed, the less your ability to filter impurities and toxins from the lymph fluid and return it to the blood stream. In my logic, this is a matter of math: how many nodes were removed regardless of how many nodes had cancer.
Many surgeons will remove one lymph node, a “sentinel” node for biopsy. If this node is clear of cancer cells, they may not remove any additional nodes. I would assess risk of lymphedema as “very low” with a single node excision, although the risk would be higher than in a person who had no surgery and no nodes removed. Up to about 5 or 6 nodes, I would still consider lymphedema risk to be low.
I consider lymphedema risk to be “moderate” is cases of removal of up to 10 to 12 lymph nodes. In my experience, when surgeons report they removed “all accessible nodes”, that number is generally reported to be around 22 to 25 nodes. Based on averages, the removal of more than 12 nodes means you have lost half of your clean-up crew, thereby increasing your risk of lymphedema substantially, and falling into my “high risk” category.
General Strategies for Lymphedema Prevention
Lymphedema prevention is crucial. Treatment is time consuming and costly, and frankly speaking, experienced lymphedema specialists can be difficult to find. Even in a city the size of San Antonio, we only have a few that I would send my favorite aunt to (all my aunts are my favorite).
There are some key points of general lymphedema prevention, which simply put is: avoid additional trauma, and broaden your definition of “trauma”. Here are things to avoid to the surgical side, or in the case of bilateral mastectomy, the side with the greater number of lymph nodes excised:
Shots and immunizations
Having blood drawn
Having blood pressure checked
Exposure to sunlight
Exposure to insect bites
Exposure to harsh chemicals
Over-activity
Bad posture
This is a good list for general circumstances. If you are having a heart attack, or if you might have a life threatening injury, then think to yourself “I will live” or “I will not die”. Please don’t worry about telling emergency responders that they are taking your blood pressure in the wrong arm. If however you are in the doctor’s office for routine medical care, by all means insist they avoid your “mastectomy arm” when drawing blood or checking your blood pressure. If they have difficulty finding a vein, ask for a more experienced phlebotomist to try again before agreeing to have blood drawn on your “protected side”.
I would caution you about activity. Too much activity too soon after surgery contributes to increased scaring. I would also caution about excessive and prolonged arm use for the long haul. Avoiding overuse is tricky, because we often don’t know we over did it until a day or so later when we become aware of sore muscles. Be particularly conservative with sporadic activities, like spring cleaning, power washing the house, or yard work. I would limit heavy arm use to small increments, and gradually work up to a still conservative level over time. I would also include sports in this category. If you are right handed, and your surgical side was the right, don’t go out and hit tennis balls for an hour.
Poor posture can impede circulation. A big culprit is forward posture at the shoulders, which can restrict circulation and nerve supply in the upper chest. Stands to reason that poor posture could impede lymph drainage as well. A simple rule of thumb is to try to line up your shoulders with your ear hole. You can read more about posture in my ergonomics hub.
You probably noticed my use of the terms “mastectomy arm,” “protected side,” and “surgical side”. I encourage you to use a term with no negative connotations. Avoid terms like “bad arm” or “weak arm”. It’s a small point, but an extension of having a positive attitude.
Compression Garments for Lymphedema Prevention
Early in my career, I attended two overview presentations on lymphedema management. There were a couple take home lessons I never forgot. One was that sometimes even young healthy people develop lymphedema for reasons that we never determine. This is not the rule however. We can usually link it with some form of trauma. We also know clients with breast cancer are on the short list of those who develop lymphedema, which is linked to factors related to their breast cancer surgery.
The second take home lesson was that after breast cancer, even if only one lymph node was excised, clients should still have a compression sleeve for lymphedema prevention.
The sleeve should be worn for air travel, when outdoors or otherwise exposed to prolonged sun or insects, or if prolonged exposure is possible or likely. Use sunscreen and insect repellant, wear your compression sleeve, and wear a long sleeve shirt. An off the shelf compression sleeve is fine for these purposes, if you can find one to fit. I particularly like the Jobst Ready-to-Wear compression sleeves. Compression of 15 to 20 mmHg is sufficient. These precautions should be taken for low risk associated with the removal of one to six lymph nodes.
For moderate risk of 10 to 12 nodes excised, I recommend a compression sleeve of 20 to 30 mmHg. You should put the sleeve on upon rising and wear it 8 to 12 hours. Do this most days, for at least three to six months. If you have had 15 or so nodes excised, I would advise adhering to a stricter wear schedule of at least 12 hours, rarely missing a day, for at least six months.
With most of your lymph nodes removed at 16 or more, you are at high risk for lymphedema. You would need 30 mmHg or more compression. This will possibly mean a custom made sleeve. Put your sleeve on when you rise, when it is presumed your swelling will be at its lowest. Wear the sleeve during your waking hours. Keep to a strict wear schedule for at least a year.
The above are general recommendations, but remember everyone should wear a sleeve when flying or visiting high altitudes, and when exposed to prolonged sunlight or insect exposure.
If you are relatively slim, and don’t have a tendency in general circumstances to swell, you may not need a gauntlet or glove. Compression for your hands is indicated if you tend to swell out the bottom of your sleeve, i.e. into your hands.
I advise against the one piece sleeve and gauntlet. I have found that clients do not like these. Generally it is harder to keep gauntlets and gloves clean than it is your sleeve. There may be times when you don’t feel you need your glove. You will remove gloves often for handwashing. You may find that you purchase two to four gloves for every single sleeve due to wear and soiling.
I don’t like the sleeves with the silicone band. The purpose of the band is to keep the sleeve from rolling down. I feel that this extra tightness can impede the flow of lymph fluid on its way to the upper chest to drain in the subclavian vein. If you are heavy, or otherwise have trouble with the sleeve riding down, consider a sleeve with cap. The cap is like the sleeve of a shirt, and has a strap to secure under the opposite armpit.
If you notice swelling, then perhaps you are not wearing your compression garment enough, or your sleeve may not offer enough compression. Swelling can also be a sign that you are being too active. Immediately step up your precautions. You can develop lymphedema at any time, even 10 or 20 years after your initial surgery. If swelling persists, consult your doctor for a consult to a lymphedema specialist.
An Easy Exercise
The booklet given to breast cancer patients by the American Cancer Society has a lot of helpful information, including exercises. These are recommended for your initial post-operative recovery, but I find one of the exercises especially good, and recommend it at any time you feel that you may have some swelling.
Hold your arm straight up overhead. Open and close the hand 12 to 15 times. Begin with one set, three times a day. As tolerated, increase to three sets of 12 to 15 reps, done three times a day.
Do I Have Lymphedema?
How do you know if you have lymphedema? When does it start? That’s a great question, but unfortunately as a medical community, we are not good at early diagnosis of lymphedema. Most clients are referred for lymphedema management with fairly advanced or obvious lymphedema.
In talking to a couple of clients who developed lymphedema, it seems that it can start as swelling to all or part of the arm. The swelling tends to be firm, and described as “tight,” “uncomfortable,” or painful. This differs from typical swelling which tends to be spongy, and usually is not painful except in the extreme.
While you may have some swelling of your arm &/or hand immediately after surgery, this should resolve in a couple weeks. In my client population, seldom did anyone complain of any significant or notable swelling. Though swelling that is present post-op, and persists may be lymphedema, in my experience, lymphedema tends to occur later after surgery. I’m guessing 6 to 24 months after surgery may be common for those who develop lymphedema. Lymphedema can occur at any time however, even 20 years after breast cancer and surgery.
What Should I do if I Think I Have Lymphedema?
If you think you may have lymphedema, see your doctor as soon as possible and insist on a therapy consult. Call around and find a therapist who has extensive experience in lymphedema management. This means that a substantial percentage of their caseload is lymphedema care, or a veteran therapist who has seen a multitude of lymphedema patients over a period of years. This could be an occupational therapist or a physical therapist.
Many therapy clinics will advertize that they can provide this service. It does not mean that they should. Lymphedema is a very serious condition, requiring expert skill level. It is not entry level practice, meaning OTs and PTs do not graduate with these skills, it is an advanced area of practice. Lymphedema management is not an area a therapist can dabble in.
There are actually many massage therapists who are skilled in lymphedema management, but this is not covered by most health care plans.
Bottom line is, you have to do your homework. Don’t be afraid to make some calls, and ask some specific questions. Do you have a therapist who is experienced in lymphedema management? How many lymphedema patients per year? How many years of experience as a therapist? How many years of lymphedema care?
Therapy is often recommended three to five days a week, with special wrapping of your extremity after, which often means 90 minute appointments. Your lymphedema specialist will decide what type of compression garments you need, including what amount of compression. They may also recommend a different night sleeve, and a compression pump.
Talk to Your Health Care Provider
This article is not intended to be a substitute for professional medical advice, diagnosis or treatment. Consult your doctor. Consider asking for an occupational therapy or physical therapy consult.
More Breast Cancer Hubs
- The Gift That Cannot Be Returned - Breast Cancer by Jerilee Wei
What if you were given a gift you did not want? This was a gift that no one would want. Just what do you do with it? That is the position I found myself in and this is the true story of the power of a gift that keeps giving..... - What are the Symptoms of Breast Cancer? by Uninvited Writer
Thinking you may have breast cancer can be the scariest thing in the world. Before you panic, learn the symptoms of breast cancer and when you should visit a doctor. - Breast Cancer - Twice bitten by cindyvine
Breast Cancer again! The first time they told me I had breast cancer was on the 24th December 2003. It had come as such a complete shock that it devastated me. I'd had a blocked duct removed two weeks...
Breast Cancer Hubs by Lily Rose
- Breast Cancer Treatment - What Things The Doctors Don't Tell You
I am 38 years old and was diagnosed with Breast Cancer 26 months ago. I'm ready to share my experiences and what I've learned about what to expect from, and things that the doctors don't tell you about, breast cancer treatment. - Breast Cancer Treatment - What Else They Don't Tell You About: Shingles and More
Part two of my breast cancer journey through breast cancer treatment and what I've learned that the doctors just don't tell you... - Breast Cancer Info - My Favorite Online Resources and Products
After my breast cancer diagnosis I immediately took to the internet to gather breast cancer info...here's a list of online cancer resources and products...